Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Yedi Herdiana and Version 2 by Sirius Huang.
Gastroesophageal reflux disease (GERD) is a common esophageal disorder characterized by troublesome symptoms associated with increased esophageal acid exposure. The cornerstones of therapy in this regard include treatment with acid-suppressive agents, lifestyle modifications, and dietary therapy, although the latter has not been well defined. As concerns regarding long-term proton pump inhibitor (PPI) use continue to be explored, patients and healthcare providers are becoming increasingly interested in the role of diet in disease management.
- esophageal disorder
- lifestyle modifications
- food industry
- long-term PPI
- processing technology
- dietary treatment
1. Introduction
Gastroesophageal reflux disease (GERD) is a prevalent condition characterized by troublesome symptoms and esophageal inflammation caused by the reflux of stomach contents [1][2][1,2]. Common symptoms include burning chest pain, regurgitation, and difficulty swallowing, while extraesophageal manifestations such as coughing and hoarseness can also occur [3][4][5][3,4,5]. Unhealthy dietary patterns high in fat, sugar, salt, and cholesterol contribute to the increasing incidence of chronic diseases like GERD within the aging global population. In Asia, particularly in Japan, there has been a rapid rise in GERD cases, which are often aggravated by high-fat meals [6]. The complications of GERD include esophagitis, hemorrhage, stricture, Barrett’s esophagus, and adenocarcinoma [7]. GERD is a significant health and social issue that negatively impacts quality of life [8][9][10][8,9,10].
GERD symptoms can be influenced by multiple risk factors [6][11][6,11]. Additionally, specific types of food and beverages, such as fast food, tea, oily food, and carbonated drinks, have been associated with an increased prevalence of GERD. Certain conditions like hiatal hernias, pregnancy, lifestyle choices, and certain medications can also trigger acid reflux and increase the risk of developing GERD [12]. Epidemiological studies have revealed several potential risk factors for GERD, including excess adiposity, diabetes, alcohol consumption, and coffee and caffeine consumption [12]. Sociodemographic factors such as age, marital status, and employment status have also been associated with GERD [13].
The treatment options for managing the symptoms of GERD encompass pharmaceutical, surgical, dietary, and lifestyle interventions. The primary approach in treating GERD involves using proton pump inhibitors (PPIs) to reduce acid secretion and reflux. However, previous studies have indicated that a notable proportion of patients (20–30%) continue to experience persistent symptoms despite receiving standard treatment with PPIs. Furthermore, approximately 47.8% of individuals who initially achieved complete resolution of GERD symptoms experienced symptom recurrence after discontinuing PPI therapy. It is worth noting that the long-term use of PPIs has also been associated with an increased risk of foodborne infections. Additional treatment options include acid-suppressive therapy and implementing lifestyle modifications [6].
2. Pathophysiology of GERD
GERD occurs when the contents of the stomach reflux into the esophagus, causing bothersome symptoms and potential long-term complications. Typical GERD symptoms include heartburn and acid regurgitation, while atypical manifestations encompass noncardiac chest pain, coughing, and laryngitis [14][16]. Mechanistically, GERD and its associated complications arise when the esophageal mucosa is abnormally exposed to refluxed stomach contents. GERD can arise due to a weakened gastroesophageal barrier, the ineffective clearance of refluxed fluid, or changes in the composition of the refluxed fluid. Repeated exposure to these factors leads to alterations in the integrity of the esophageal lining and the cellular makeup of the tissue [15][16][17,18].
The pathogenesis of GERD involves various mechanisms, such as motor dysfunctions, hiatal hernias, and impaired mucosal resistance (Figure 1) [17][19]. The following factors may contribute to the development of GERD.
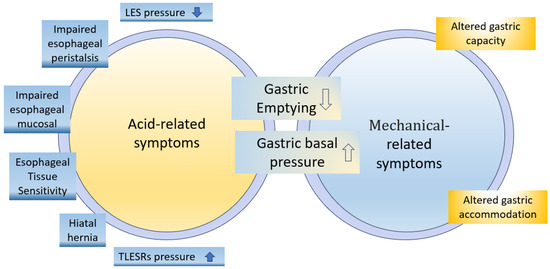
Figure 1. Pathophysiological mechanisms involved in development of upper gastrointestinal (GI) symptoms [17].
-
Lower esophageal sphincter dysfunction
The lower esophageal sphincter (LES) prevents stomach contents from refluxing into the esophagus. It contracts between meals and relaxes during swallowing or transient LES relaxations (TLESRs). People with GERD experience symptoms when the LES relaxes more frequently. LES tone is influenced by neural, hormonal, and dietary factors [6]. TLESRs are triggered by gastric distention from food or air intake, which is influenced by dietary factors and medications. Frequent TLESRs unrelated to swallowing can lead to the reflux of stomach contents into the esophagus due to the higher intragastric pressure than LES pressure in individuals with GERD symptoms [6][16][18][19][6,18,20,21].
- 2.
-
Enhanced proximal postprandial gastric acid pocket (PPAGP)
Below the LES lies the PPGAP, where, after a meal, highly acidic stomach contents can accumulate if they do not mix well with the consumed food. In individuals with GERD, the PPGAP is larger, more acidic, and persists longer than in those without GERD. For individuals with a hiatal hernia, the PPGAP can push upwards through the LES, leading to GERD symptoms. Understanding the PPGAP helps explain why some people experience reflux symptoms after eating [20][21][22][22,23,24].
- 3.
-
Delayed gastric emptying
In approximately 26% of GERD patients, delayed gastric emptying prolongs the retention of acidic food in the stomach, thereby increasing reflux risk. Delayed emptying raises stomach pressure, relaxing the LES and allowing acid into the esophagus, thus contributing to GERD symptoms [15][23][17,25]. Peristalsis helps minimize reflux duration by propelling contents upwards, while factors like large food boluses or increased viscosity can slow down contractions. Increased intra-abdominal pressure or food retention inhibits reflux. Refluxed stomach fluid contains irritants like gastric acid, digestive enzymes, and bile salts that can potentially harm the esophageal mucosa. Changes in dietary intake can alter the secretion of these components, and undigested food particles may also contribute to reflux, with varying effects on the underlying mucosa [6][24][6,26].
- 4.
-
Impaired esophageal peristalsis
About 21% of GERD patients are afflicted with impaired esophageal peristalsis, which normally helps clear stomach acid from the esophagus. This reduced clearance of refluxed acid causes the esophageal tissues to be exposed to acidic gastric contents for longer durations, leading to increased damage and more severe GERD symptoms [25][26][27,28]. Alongside esophageal peristalsis, the neutralization of gastric acid by salivary bicarbonate plays a protective role in the esophagus. Nevertheless, when peristalsis is impaired, the salivary bicarbonate may not be sufficient to counteract the damaging effects of the refluxed acid [27][29].
- 5.
-
Impaired esophageal mucosal defense against the gastric refluxate
The esophageal mucosa is a protective barrier against the substances encountered during GERD. This barrier comprises various structural and functional components that defend against the refluxate, including acidic gastric fluid (hydrochloric acid and pepsin) and alkaline duodenal fluid (bile salts and pancreatic enzymes). Prolonged exposure to the refluxate can breach this defensive barrier, resulting in mucosal damage. In addition to refluxate, drugs can also contribute to esophageal wall damage by directly affecting the esophageal mucosa, creating an acidic or alkaline environment exerting caustic effects. Drug-induced esophagitis can manifest as self-limiting inflammation, but if it persists, it can lead to complications such as severe ulceration, strictures, and, rarely, perforation. It is important to note that GERD can further worsen drug-induced esophagitis, exacerbating the associated symptoms and complications [28][29][30,31].
- 6.
-
Hiatal hernia
A hiatal hernia is often observed in association with GERD and can exist without causing symptoms. However, it plays a crucial role in the development of GERD by interfering with the function of the LES. Research by Patti et al. found that patients with confirmed GERD, regardless of whether they had presented a small hiatal hernia, exhibited similar abnormalities in LES function and acid clearance. However, patients with large hiatal hernias had shorter and weaker LESs, leading to increased reflux episodes. Moreover, the study noted that patients with large hiatal hernias experienced more severe esophagitis. Another study by Ott et al. revealed that 94% of patients with reflux esophagitis had hiatal hernias, highlighting the strong association between the two conditions [30][31][32,33].
- 7.
-
Esophageal Tissue Sensitivity
Individuals with GERD may have heightened sensitivity in their esophageal tissues to even small amounts of acid, resulting in symptoms such as heartburn, chest pain, and regurgitation. Gastric acid increases sensitivity to reflux, enhancing the perception of reflux symptoms. Acid-induced hypersensitivity is more significant in the proximal esophagus due to acid’s damaging effects on the mucosa, impairing barriers and exposing mucosal nerves to toxic refluxate [32][34].
3. Complexity of GERD
The complexity of this disease and the multiplicity of its clinical manifestations hinder the development of a singular diagnostic test [33][35]. Several factors influence the association between diabetes and acid reflux. Firstly, diabetic neuropathy, i.e., nerve damage caused by diabetes, can increase the likelihood of experiencing acid reflux. Additionally, certain medications used for acid reflux treatment, like PPIs, have been linked to a higher risk of developing type 2 diabetes [34][35][36][36,37,38]. Conversely, having type 2 diabetes can also raise one’s likelihood of experiencing acid reflux due to the damage high blood sugar levels inflict on the gastrointestinal tract. Patients with DM are at a greater risk of GERD than those who do not have DM [37][39]. Obesity, a significant risk factor for both conditions, further strengthens their connection [12].
GERD is common among people with asthma and can worsen and trigger asthma attacks. Treating GERD improves the respiratory symptoms of asthma patients [38][40]. Possible GERD–asthma symptoms include reflux-related respiratory issues, worsened asthma after meals or lying down, nocturnal asthma, and poor responses to bronchodilators [39][41]. GERD increases the risk of contracting respiratory infections, including pneumonia, due to refluxate aspiration into the lungs and impaired lung defense mechanisms [40][42].
Barrett’s esophagus is a condition where the normal lining of the esophagus is replaced by different tissue. It can lead to esophageal adenocarcinoma, a type of cancer, in 3–5% of patients [41][43]. Barrett’s esophagus develops from progenitor cells at the esophagogastric junction as part of a wound-healing process, replacing damaged squamous epithelium caused by GERD [42][44].
The oral and maxillofacial manifestations of GERD consist of dental erosion, xerostomia, mucositis, aphthous-like ulcerations, a persistent sour taste, burning mouth, hyperesthesia, bruxism, and temporomandibular disorder [43][45]. GERD can cause dental problems by exposing tooth enamel to stomach acid, leading to erosion and increased vulnerability to tooth decay [44][45][46,47]. GERD can result in tooth sensitivity, enamel erosion, and changes in tooth appearance. Acid reflux can also irritate the gums, causing inflammation, tenderness, and an increased risk of gum disease [46][48].
GERD disrupts sleep due to nighttime heartburn and regurgitation. Managing GERD through lifestyle changes and medical treatments improves sleep. GERD can cause dysphagia, chronic cough, and sinusitis [2]. Treating GERD and sleep apnea is crucial. Esophagitis associated with GERD requires comprehensive evaluation beyond acid reflux alone [47][49].
4. Dietary Factors Pertaining to GERD
The literature on dietary intervention in relation to GERD varies, but some common recommendations can guide patient care [6]. Diet plays a significant role in gastrointestinal health, with certain foods worsening GERD symptoms [6]. High-fat meals, alcohol, chocolate, and carbonated beverages can reduce esophageal sphincter pressure and increase acid exposure [6][48][6,50]. Consuming a healthy diet with high fruit and whole grain content, like the Mediterranean diet, may improve GERD symptoms. Improving dietary habits can be a cost-effective strategy with which to reduce the occurrence of GERD instead of relying solely on medication [48][50].
GERD management entails a comprehensive approach involving optimizing meal sizes, timing, and macronutrient composition. Prioritizing the reduction in meal size, the consumption of simple sugars, and late-night eating helps to mitigate GERD symptoms [6][49][6,51]. Caution should be exercised with high-calorie, large-volume, and high-fat meals, as these dietary factors have been linked to exacerbating esophageal reflux [50][52]. Adopting a slow eating pattern also represents a potential lifestyle modification that may help alleviate GERD symptoms [51][53]. Scientific evidence supports the notion that fat does not significantly impact esophageal sensitivity to acid [52][54].
Furthermore, establishing regular eating patterns is crucial to effective GERD management [53][54][15,55]. Esophageal acid exposure (EAE) may be more severe after consuming a high-calorie diet than a low-calorie diet with the same fat content. However, patient classification variations and test meal component differences have led to discrepancies between studies [53][15]. Calorie density plays a role in determining the severity of esophageal acid exposure during GERD after a meal. At the same time, the percentage of fat content in one’s diet significantly impacts the frequency of reflux symptoms [55][56]. Moreover, a positive relationship exists between high-calorie foods and non-erosive reflux disease (NERD) [56][57].
Fox et al. found causal links between higher BMI, type 2 diabetes, and an increased risk of GERD. These factors play significant roles in GERD development [12]. GERD is extremely common, and even modest weight gain has been associated with higher symptom burden and objective evidence of reflux observed via endoscopy and physiological measurements [50][52].
GERD management entails the avoidance of trigger foods like spicy food, citrus fruits, tomatoes, onions, garlic, chocolate, mint, caffeinated beverages, alcohol, and carbonated drinks [48][50], prioritizing the consumption of lean proteins and emphasizing the intake of whole grains and fiber-rich foods like oatmeal and brown rice instead [6][57][6,58]. In one study, individuals with the highest intake of fruits and vegetables demonstrated a 33% lower risk of developing GERD [58][59]. Additionally, it is recommended that one opts for low-fat dairy products and restricts their consumption of high-fat foods, oils, and fried foods. Adopting a dietary pattern that includes smaller, more frequent meals may help mitigate stomach pressure, while ensuring proper hydration between meals is crucial for effectively managing GERD [59][60].
The intake of functional foods is very beneficial; for instance, in reference to calcium (dietary calcium intake of 700–1000 mg per day or supplementary calcium intake of 1000 mg per day significantly increases the risk of cardiovascular disease and coronary heart disease [60][61]), acquiring calcium from dietary sources is generally considered safe and beneficial. Calcium-rich foods include dairy products, leafy green vegetables, fortified plant-based milk alternatives, and certain fish. It is recommended that individuals meet their calcium requirements through a balanced diet rather than relying solely on supplements [61][62].
In the study conducted by Özenoğlu et al., it was found that diets rich in vegetables, fiber, antioxidants, and caffeine did not exhibit a significant association with an increased risk of dysphagia, which is a symptom commonly associated with GERD [48][62][50,63]. GERD is strongly associated with dietary and lifestyle patterns [63][64]. It positively correlates with alcohol consumption, higher stress levels, education, inadequate sleep, sedentary and physically demanding jobs, nighttime work, lack of exercise, and increased abdominal pressure (e.g., obesity or pregnancy) [56][57].
5. Management Treatment of GERD
The Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) has established evidence-based guidelines for managing GERD patients. Nevertheless, additional studies with a low risk for bias are required to further enhance and refine these guidelines [64][65].
GERD management encompasses various diagnostic approaches, including medical history consideration, physical examination, upper endoscopy, pH monitoring, esophageal manometry, and the barium swallow test. These diagnostic tools help assess the severity of GERD and inform treatment decisions [65][66].
Lifestyle modification is an important aspect of managing GERD. Avoiding reflux-triggering foods and drinks and eating smaller, more frequent meals can help reduce the chance of reflux. Guidelines suggest that individuals avoid lying down immediately after eating and elevate their heads off their beds by 6–8 inches while sleeping. Maintaining a healthy weight through regular exercise and a balanced diet is also recommended for GERD management [66][67][67,68].
Medication plays an important role in managing GERD. The pharmacological targets in this regard have included, firstly, gastric acid neutralization (antacids); secondly, gastric acid secretion reduction (H2 receptor antagonists or PPIs); thirdly, the installation of a physical barrier against refluxate (alginates); fourthly, improved gastric emptying and upper gut motility (prokinetics); and, finally, more recently, in adults, anti-depressant drugs [68][69][69,70]. Surgical intervention may be required in severe cases of insufficient medications and lifestyle changes. The most common surgical procedure for GERD is fundoplication, in which the upper part of the stomach is wrapped around the lower esophagus to strengthen the LES and prevent reflux [33][35]. Surgical treatment is considered a last resort for managing GERD. It is recommended when optimal medical therapy fails, long-term dependence on medication is necessary, the degree of nonadherence to medical therapy is significant, or life-threatening complications occur [70][71][72][71,72,73]. Laparoscopic approaches have become more common and offer similar reflux control and quality-of-life outcomes when compared to open surgeries [73][74][74,75]. Robotically assisted laparoscopic surgery for anti-reflux and hiatal hernia procedures is becoming more widespread [75][76].
Attending regular check-ups with healthcare professionals is important for the effective management of GERD. These appointments allow for the monitoring of symptoms, the evaluation of treatment effectiveness, and the assessment of any complications or progression of the condition.
