The bladder is a hollow organ located in the lower abdominal region. The bladder is contiguous with the ureters above, through which urine flows from the kidneys, and the urethra below, which dispels urine from the body. There are four parts to the bladder, the apex or dome, body, fundus, and neck. The apex is the anterosuperior part of the bladder that points towards the abdominal wall. The fundus, or base, is the posteroinferior part of the bladder. The fundus lies on the inferior aspect of the proximal wall while the apex lies on the anterior aspect of the wall, extending towards the pubic symphysis. The body of the bladder is the large area situated between the apex and the fundus. The neck of the bladder is the constricted part of the bladder that leads to the urethra. The upper part of the bladder consists of the apex and body which are above the ureteric orifices. The lower part consists of the fundus, neck, and trigone. The trigone is an inverted triangular-shaped area of space that is made entirely of smooth muscle. Its superolateral angles are formed by the ureteric orifices. The neck lies at the base of the trigone and it is the most inferior point of the bladder.
- bladder cancer
- urothelial carcinoma
- squamous differentiation
- glandular differentiation
- squamous cell carcinoma
1. Introduction
2. Stages of Bladder Cancer
Urothelial carcinomas (UC) can be divided into two categories: NMIBC and MIBC. Approximately 75% of UC are NMIBC [20]. According to WHO classification systems, NMIBC are further divided into three stages: Carcinoma in situ (CIS), Ta (non-invasive papillary), and T1 [21]. These can be further sub-graded as either low or high-grade. Both Ta and CIS are considered non-invasive (Figure 1). Stage CIS is characterized by a flat lesion tumor which remains in the tissue layer from which it originates without spreading into the hollow space of the bladder. Ta, a papillary tumor, grows into the hollow area of the bladder with finger-like projections but does not spread to the connective tissue or muscle tissue of the bladder wall [22]. Cancers in the Ta and CIS stages account for 70% and 20% of all NMIBC, respectively [23]. Tumors in stage T1 spread into the connective tissue layer (lamina propria) under the lining layer of the bladder, but do not spread into the muscle layer. In general, NMIBC is characterized by high recurrence of tumors and a high survival rate after therapeutic mechanisms are employed [24].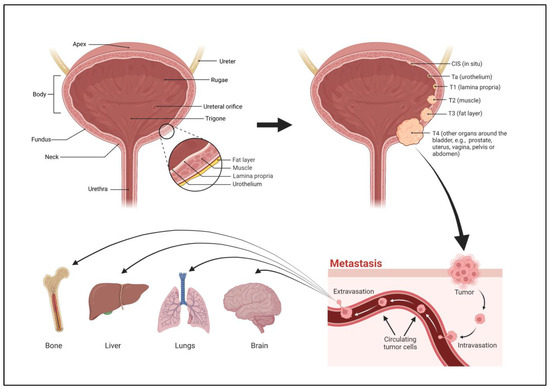
3. Grades of Bladder Cancer
Grading of bladder cancer is differentiated by a pathologist based on histological diagnosis. Low-grade NMIBC is characterized by high recurrence rates, but rare propensity (10–15%) to progress into high-grade BlCa, invade, or metastasize [26]. High-grade NMIBC comprises the tumors that are characterized by a quick progression into invasive tumors, those of the MIBC category [27]. Ta often recurs after surgical resection, but rarely progress to high-grade T1 tumors or to MIBC (seen in <10% of cases). In contrast, CIS tumors progress in about 50% of cases to T1 and then to MIBC. About 80% of MIBC are thought to arise from CIS tumors. Studies have shown that the ability for low-grade BlCa to progress into high-grade BlCa is likely due to acquired TP53 mutations, whereas TP53 mutations are more frequent in high-grade BlCa, and FGFR3 mutations are more frequent in low-grade tumors [28]. Almost all mortality from BlCa results from high-grade disease. It may be noted that the low vs. high grade designation is typically used only for transitional cell carcinoma. For squamous cell carcinoma or adenocarcinoma, a gradation system of well, moderate, or poorly differentiated cancers is used.4. Types of Bladder Cancer
BlCa is a heterogeneous disease with multiple subtypes and variants. The most common histology of BlCa is urothelial carcinoma (UC) (also known as transitional cell carcinoma, TCC) that originates in the urothelial cells of the bladder. UC accounts for up to 90% of all BlCa diagnoses [29]. Certain variants of UC elucidated by the World Health Organization (WHO) are rare and hard to diagnose. UC with squamous differentiation (UCSD) is the most common histological variant, found in T1 tumors 8–15% of the time and 20–60% of the time in MIBC. It presents with a significantly higher pathologic stage than pure UC and is defined as high-grade [30]. UCSD is defined by the presence of clear-cut intercellular bridges, intracellular keratinization, or both [31]. As other works have reported, squamous differentiation is significantly correlated with multiple severe prognostic factors including progression to grade 3, lymphovascular invasion, advanced tumor stage, and lymph node metastasis [32]. UC with glandular differentiation (UCGD) is the second most common histological variant and is found in around 10% of all UC cases. This kind of differentiation is more often visualized as urothelial carcinoma with gland-like lumina [31]. Glandular differentiation can exist either in the form of pure adenocarcinoma (rarer and largely associated with schistosomiasis as well as bladder exstrophy) or UCGD [33]. Secondary to UC is squamous cell carcinoma (SCC) of the bladder. SCC accounts for the remaining 10% of BlCa cases and is more common in Africa where it is associated with the protozoan infection schistosomiasis [12][15]. SCC is largely characterized by keratin deposits [34]. It is of important clinical significance to distinguish SCC from UCSD as the latter is treated similarly to pure UC while the former is resistant to chemotherapy requiring radical cystectomy (RC) without neoadjuvant chemotherapy (NAC) [33]. Chronic irritation of the bladder due to bladder stones, multiple urinary tract infections, or long-term indwelling catheters can lead to SCC and can initiate metaplasia from transitional cells to squamous cells [35][36]. SCC has a significantly worse prognosis than UC [37]. Other, rarer forms of BlCa include adenocarcinoma which is only found in 0.5–2% of all cases and small cell carcinoma which is found in less than 1% of all BlCa cases [38]. Small cell carcinoma is poorly differentiated, and highly metastatic with a poorer prognosis than pure UC [39].References
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer statistics. CA Cancer J. Clin. 2022, 72, 7–33.
- Martin, P.; Hooker, M.; Aktar, M.; Stockton, M. How many workers are employed in California agriculture? Calif. Agric. 2016, 71, 30–34.
- Isharwal, S.; Konety, B. Non-muscle invasive bladder cancer risk stratification. Indian J. Urol. 2015, 31, 289–296.
- Bilim, V.; Kuroki, H.; Shirono, Y.; Murata, M.; Hiruma, K.; Tomita, Y. Advanced Bladder Cancer: Changing the Treatment Landscape. J. Pers. Med. 2022, 12, 1745.
- Park, J.C.; Citrin, D.E.; Agarwal, P.K.; Apolo, A.B. Multimodal management of muscle-invasive bladder cancer. Curr. Probl. Cancer 2014, 38, 80–108.
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249.
- Halaseh, S.A.; Halaseh, S.; Alali, Y.; Ashour, M.E.; Alharayzah, M.J. A Review of the Etiology and Epidemiology of Bladder Cancer: All You Need to Know. Cureus 2022, 14, e27330.
- Baan, R.; Straif, K.; Grosse, Y.; Secretan, B.; El Ghissassi, F.; Bouvard, V.; Benbrahim-Tallaa, L.; Cogliano, V. Carcinogenicity of some aromatic amines, organic dyes, and related exposures. Lancet Oncol. 2008, 9, 322–323.
- Cumberbatch, M.G.K.; Jubber, I.; Black, P.C.; Esperto, F.; Figueroa, J.D.; Kamat, A.M.; Kiemeney, L.; Lotan, Y.; Pang, K.; Silverman, D.T.; et al. Epidemiology of Bladder Cancer: A Systematic Review and Contemporary Update of Risk Factors in 2018. Eur. Urol. 2018, 74, 784–795.
- Rosiello, G.; Palumbo, C.; Deuker, M.; Stolzenbach, L.F.; Martin, T.; Tian, Z.; Gallina, A.; Montorsi, F.; Black, P.; Kassouf, W.; et al. Racial differences in the distribution of bladder cancer metastases: A population-based analysis. Cent. Eur. J. Urol. 2020, 73, 407–415.
- Wang, Y.; Chang, Q.; Li, Y. Racial differences in Urinary Bladder Cancer in the United States. Sci. Rep. 2018, 8, 12521.
- Saginala, K.; Barsouk, A.; Aluru, J.S.; Rawla, P.; Padala, S.A.; Barsouk, A. Epidemiology of Bladder Cancer. Med. Sci. 2020, 8, 15.
- Sui, X.; Lei, L.; Chen, L.; Xie, T.; Li, X. Inflammatory microenvironment in the initiation and progression of bladder cancer. Oncotarget 2017, 8, 93279–93294.
- Manley, K.V.; Hubbard, R.; Swallow, D.; Finch, W.; Wood, S.J.; Biers, S.M. Risk factors for development of primary bladder squamous cell carcinoma. Ind. Mark. Manag. 2017, 99, 155–160.
- Mostafa, M.H.; Sheweita, S.A.; O’connor, P.J. Relationship between Schistosomiasis and Bladder Cancer. Clin. Microbiol. Rev. 1999, 12, 97–111.
- Sharma, P.K.; Pandey, P.K.; Vijay, M.K.; Bera, M.K.; Singh, J.P.; Saha, K. Squamous cell carcinoma in exstrophy of the bladder. Korean J. Urol. 2013, 54, 555–557.
- Talar-Williams, C.; Hijazi, Y.M.; Walther, M.M.; Linehan, W.M.; Hallahan, C.W.; Lubensky, I.; Kerr, G.S.; Hoffman, G.S.; Fauci, A.S.; Sneller, M.C. Cyclophosphamide-Induced Cystitis and Bladder Cancer in Patients with Wegener Granulomatosis. Ann. Intern. Med. 1996, 124, 477–484.
- Suriano, F.; Altobelli, E.; Sergi, F.; Buscarini, M. Bladder cancer after radiotherapy for prostate cancer. Rev. Urol. 2013, 15, 108–112.
- Bhat, S.; Sathyanarayanaprasad, M.; Paul, F. Primary squamous cell carcinoma of bladder exstrophy in an adult. Indian J. Urol. 2015, 31, 142–143.
- Miyazaki, J.; Nishiyama, H. Epidemiology of urothelial carcinoma. Int. J. Urol. 2017, 24, 730–734.
- Yin, P.N.; Kc, K.; Wei, S.; Yu, Q.; Li, R.; Haake, A.R.; Miyamoto, H.; Cui, F. Histopathological distinction of non-invasive and invasive bladder cancers using machine learning approaches. BMC Med. Inform. Decis. Mak. 2020, 20, 162.
- Adamczyk, P.; Pobłocki, P.; Kadlubowski, M.; Ostrowski, A.; Wróbel, A.; Mikołajczak, W.; Adamowicz, J.; Drewa, T.; Juszczak, K. A Comprehensive Approach to Clinical Staging of Bladder Cancer. J. Clin. Med. 2022, 11, 761.
- Blanca, A.; Lopez-Beltran, A.; Lopez-Porcheron, K.; Gomez-Gomez, E.; Cimadamore, A.; Bilé-Silva, A.; Gogna, R.; Montironi, R.; Cheng, L. Risk Classification of Bladder Cancer by Gene Expression and Molecular Subtype. Cancers 2023, 15, 2149.
- Lopez-Beltran, A. Bladder cancer: Clinical and pathological profile. Scand. J. Urol. Nephrol. 2008, 42, 95–109.
- Choi, W.; Porten, S.; Kim, S.; Willis, D.; Plimack, E.R.; Hoffman-Censits, J.; Roth, B.; Cheng, T.; Tran, M.; Lee, I.-L.; et al. Identification of distinct basal and luminal subtypes of muscle-invasive bladder cancer with different sensitivities to frontline chemotherapy. Cancer Cell 2014, 25, 152–165.
- Apollo, A.; Ortenzi, V.; Scatena, C.; Zavaglia, K.; Aretini, P.; Lessi, F.; Franceschi, S.; Tomei, S.; Sepich, C.A.; Viacava, P.; et al. Molecular characterization of low grade and high grade bladder cancer. PLoS ONE 2019, 14, e0210635.
- Kirkali, Z.; Chan, T.; Manoharan, M.; Algaba, F.; Busch, C.; Cheng, L.; Kiemeney, L.; Kriegmair, M.; Montironi, R.; Murphy, W.M.; et al. Bladder cancer: Epidemiology, staging and grading, and diagnosis. Urology 2005, 66, 4–34.
- Neuzillet, Y.; Paoletti, X.; Ouerhani, S.; Mongiat-Artus, P.; Soliman, H.; de The, H.; Sibony, M.; Denoux, Y.; Molinie, V.; Herault, A.; et al. A meta-analysis of the relationship between FGFR3 and TP53 mutations in bladder cancer. PLoS ONE 2012, 7, e48993.
- Kaseb, H.; Aeddula, N.R. Bladder Cancer; StatPearls: Tampa, FL, USA, 2023.
- Minato, A.; Noguchi, H.; Tomisaki, I.; Fukuda, A.; Kubo, T.; Nakayama, T.; Fujimoto, N. Clinical Significance of Squamous Differentiation in Urothelial Carcinoma of the Bladder. Cancer Control 2018, 25, 1073274818800269.
- Amin, M.B. Histological variants of urothelial carcinoma: Diagnostic, therapeutic and prognostic implications. Mod. Pathol. 2009, 22 (Suppl. S2), S96–S118.
- Makise, N.; Morikawa, T.; Kawai, T.; Nakagawa, T.; Kume, H.; Homma, Y.; Fukayama, M. Squamous differentiation and prognosis in upper urinary tract urothelial carcinoma. Int. J. Clin. Exp. Pathol. 2015, 8, 7203–7209.
- Warrick, J.I. Clinical Significance of Histologic Variants of Bladder Cancer. J. Natl. Compr. Cancer Netw. 2017, 15, 1268–1274.
- Martin, J.W.; Carballido, E.M.; Ahmed, A.; Farhan, B.; Dutta, R.; Smith, C.; Youssef, R.F. Squamous cell carcinoma of the urinary bladder: Systematic review of clinical characteristics and therapeutic approaches. Arab. J. Urol. 2016, 14, 183–191.
- Ho, C.-H.; Sung, K.-C.; Lim, S.-W.; Liao, C.-H.; Liang, F.-W.; Wang, J.-J.; Wu, C.-C. Chronic Indwelling Urinary Catheter Increase the Risk of Bladder Cancer, Even in Patients Without Spinal Cord Injury. Medicine 2015, 94, e1736.
- PDQ Supportive and Palliative Care Editorial Board. PDQ Cancer Information Summaries. 2022. Available online: https://www.ncbi.nlm.nih.gov/books/NBK65883/ (accessed on 9 May 2023).
- Bandini, M.; Pederzoli, F.; Madison, R.; Briganti, A.; Ross, J.S.; Niegisch, G.; Yu, E.Y.; Bamias, A.; Agarwal, N.; Sridhar, S.S.; et al. Unfavorable Cancer-specific Survival After Neoadjuvant Chemotherapy and Radical Cystectomy in Patients with Bladder Cancer and Squamous Cell Variant: A Multi-institutional Study. Clin. Genitourin. Cancer 2020, 18, e543–e556.
- Dadhania, V.; Czerniak, B.; Guo, C.C. Adenocarcinoma of the urinary bladder. Am. J. Clin. Exp. Urol. 2015, 3, 51–63.
- Ismaili, N. A rare bladder cancer—Small cell carcinoma: Review and update. Orphanet J. Rare Dis. 2011, 6, 75.
