Characterized in biomedical terms, stretching exercises have been defined as movements applied by external and/or internal forces to increase muscle and joint flexibility, decrease muscle stiffness, elevate the joint range of motion (ROM), increase the length of the “muscle–tendon” morpho-functional unit, and improve joint, muscle, and tendon movements, contraction, and relaxation. The present review examines and summarizes the initial and recent literature data related to
the biomechanical, physiological, and therapeutic effects of static stretching (SS) on flexibility and other physiological characteristics of the main structure and the “joint–ligament–tendon–muscle” functional unit. The healing and therapeutic effects of SS, combined with other rehabilitation techniques (massage, foam rolling with and without vibrations, hot/cold therapy, etc.), are discussed in relation to the creation of individual (patient-specific) or group programs for the treatment and
prevention of joint injuries, as well as for the improvement of performance in sports. From a theoretical point of view, the role of SS in positively affecting the composition of the connective tissue matrix is pointed out: types I–III collagen syntheses, hyaluronic acid, and glycosaminoglycan (GAG) turnover under the influence of the transforming growth factor beta-1 (TGF-β-1). Different variables, such as collagen type, biochemistry, elongation, and elasticity, are used as molecular biomarkers. Recent studies have indicated that static progressive stretching therapy can prevent/reduce the development of arthrogenic contractures, joint capsule fibrosis, and muscle stiffness and requires new clinical applications. Combined stretching techniques have been proposed and applied in medicine and sports, depending on their long- and short-term effects on variables, such as the ROM, EMG activity, and muscle stiffness. The results obtained are of theoretical and practical interest for the development of new experimental, mathematical, and computational models and the creation of efficient therapeutic programs. The healing effects of SS on the main structural and functional unit—“joint–ligament–tendon–muscle”—need further investigation, which can clarify and evaluate the benefits of SS in prophylaxis and the treatment of joint injuries in healthy and ill individuals and in older adults, compared to young, active, and well-trained persons, as well as compared to professional athletes.
- stretching
- static stretching (SS)
- joint range of motion (ROM)
- muscle stiffness
1. Introduction
2. Biomechanical Parameters, Healing, and Therapeutic Effects of Stretching
Interesting results arose from numerous recent investigations and various stretching programs applied in medical practice and sports. The biomechanical parameters and therapeutic effectiveness of stretching applications could modify joint, tendon, and muscle flexibility. For this purpose, different variables, such as collagen and elastin syntheses, fiber elongation and elasticity, energy absorption, etc., could be used as mechanobiological, cellular, and molecular biomarkers. Many retrospective and prospective studies have been performed and stratified on the acute and chronic effects of stretching, both under physiological conditions and in pathological states. Progressive static stretching is effective during the prophylaxis of injuries in sports and exercise training [8][9][10][8,9,10]. The healing properties of stretching are of importance in the prophylaxis and treatment of joint injuries when also combined with other rehabilitation procedures (massage, heat/cold, warming up, etc.) [7][11][12][13][14][7,11,12,13,14]. Recent studies have reported a high effectiveness of stretching in the treatment and prevention of contractures and fasciitis, as well as useful methods for application in routine orthopedic and traumatological practice [5][15][16][17][18][19][5,15,16,17,18,19]. As a rehabilitation method, stretching has been applied to improve the biomechanical parameters of muscles, tendons, ligaments, fascia, and joints [4][6][7][9][20][21][4,6,7,9,20,21]. The viscoelastic responses of muscles, tendons, ligaments, fascia, and joints to slow stretching exercises could result in less passive tension, compared to faster procedures [22][23][22,23]. The faster the stretch, the higher the muscle stiffness will be [6]. Most stretching techniques (static, dynamic, ballistic, etc.) have been successfully implemented in clinical practice [2][4][24][25][2,4,24,25]. The effects of stretching on muscle and joint flexibility are closely related to the joint range of motion (ROM), whereby the increased range of motion induces the analgesic effects of stretching. Various stretching techniques have been compared. Unfortunately, the current results of the chronic effects of static stretching (SS) exercises on the muscle strength, flexibility, joint ROM, and muscle power are still controversial [5][18][26][5,18,26].3. Animal, Mathematical, and Computational Models of Stretching
More scientific information is needed for the creation of new, successful mathematical and computational models of stretching [27][28][27,28]. The mathematical and rheological models of the joint cavity capsule and intra-articular synovial fluid turnover (viscosity and permeation of hyaluronan, glycosaminoglycans (GAGs), and albumin) indicate cellular mechanisms of stretching and a role of the intercellular matrix as a selective molecular filter. The specific rheological properties of joint synovial fluid are altered in traumatic and post-traumatic pathological states (different arthroses, rheumatoid arthritis, osteoarthritis, etc.) [29]. In the treatment and prevention of sports injuries, as well as in the development of improved sports programs for injury prevention, static stretching (SS) is very important for the efficient rehabilitation of joints [3][30][31][32][33][34][3,30,31,32,33,34]. Based on the latest scientific findings, especially on the biomechanical contributions in this field, new preventive and therapeutic measures for avoiding stiffness and motion impairment in the joints can be adopted during the early stages of diseases [2][9][15][2,9,15]. The therapeutic effects of stretching have been established in a great number of experimental animal models (e.g., post-traumatic knee contractures in rat and rabbit models, which have significance for humans) [7][35][36][37][38][7,35,36,37,38]. Thus, it is possible to evaluate important data on cellular functions and the intracellular matrix components of joint cartilage, as well as information on the morphological structures and functions of joint capsules, both in healthy controls and in joints that have been modified in the processes of contractures (post-traumatic, myogenic, arthrogenic, etc.) [7][11][36][37][38][39][7,11,36,37,38,39]. Zhang et al. examined the effect of stretching combined with ultrashort wave diathermy on joint functions and clarified its cellular mechanisms in a rabbit knee contracture model [38]. Wang L. et al. [7] studied the effects of different static progressive stretching durations on the knee joint’s range of motion, collagen- and alpha-actin expressions in fibroblasts, inflammatory cell number, and fibrotic changes in the joint capsule (as the result of different static progressive stretching durations applied to a post-traumatic knee contracture in a rat model). The authors concluded that static progressive stretching could improve post-traumatic knee contractures by increasing the knee joint mobility. Numerous animal models that simulate a “knee flexion contracture” and a few models of a “knee extension contracture” have been proposed [11]. The authors determined that the “aggravation of contractures” was correlated with the degree of “fibrosis response” of the joints, which is related to the activation of type I and type III collagen syntheses, as well as to the stimulation of pro-fibrotic gene expression in fibroblasts and chondroblasts. A proteomic analysis of the muscles and joint capsule was performed by the same study group [11]. The expression of transforming growth factor beta-1 (TGF-β-1) was also examined as a significant biomarker of changes in the synthesis and distribution of different collagen types (I–III) in the intercellular matrix. An important fact of clinical relevance is that “extension contracture models” better mimic fractures and the bed-associated immobilization of patients in traumatology than “flexion contracture models”. The main question related to stretching biomechanics is: “Could chronic stretching change the joint–ligament–tendon–muscle mechanical properties?” The effects of stretching were reported for joint resistance and muscle and tendon stiffness, but a large heterogeneity was seen for most of the variables obtained [4]. The same authors analyzed 26 papers regarding longitudinal stretching (static, dynamic, and/or PNF) in humans of any age and with different health statuses. Structural and mechanical variables were evaluated for joints and muscle–tendon units: dynamic stretching, static stretching, flexibility, stiffness, mechanical joint properties, muscle morphology and functional activities, changes in the tendon characteristics, proprioceptive neuromuscular facilitation, etc. [6]. Adaptations to chronic stretching protocols shorter than 8 weeks seemed to occur mostly at the sensory level [6].4. Biomechanical Effects of Static and Active Isometric Stretching Applied to the Human Knee Joint
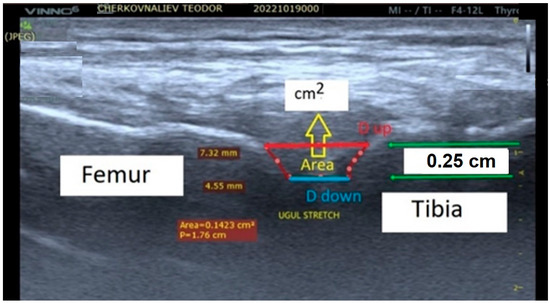
The effects of stretching on muscle properties are clearly described in literature and depend on various factors, including stretching techniques, stretching time, retention time, rest time, and the time difference between the intervention and the measurement [28][40][41][28,40,41]. Most studies investigated the effects of static stretching on the passive properties of the muscle–tendon unit [42][43][44][45][46][42,43,44,45,46]. In a series of studies by Magnusson et al. [42][43][45][46][47][42,43,45,46,47], it was shown that static stretching for 90 s over five repetitions reduced muscle resistance, passive stiffness, peak torque, and stress relaxation. Another team of researchers [48][49][48,49] concluded that changes in the viscoelastic properties of the muscle–tendon unit depend more on the duration of stretching than on the number of stretches. An extension of static stretching time (from five to ten minutes) was shown to reduce tendon stiffness, as measured passively by ultrasonography [48][49][48,49]. The reduction in stiffness might be due to a change in the arrangement of collagen fibers in the tendon [48]. Stretching increased the range of motion of the femoral flexion and the outer rotation [21]. Isometric stretching is a type of static stretching associated with the resistance of muscle groups through isometric contractions of the stretched muscles. Due to the fact that this type of muscle stretching works in an isometric mode, the initiated muscle forces will affect the joints around which the muscles are located. The muscle forces produced by this type of stretching trigger processes within the joint itself. Cotofana et al. [50] demonstrated that the cartilage thickness decreased to 5.2% from a knee load with a force equal to 50% of the body weight. Herberthold et al. [51] evaluated the deformation at a force load equal to 150% of the body weight. TheOur experimental model and working hypothesis estimated that, as the result of active isometric stretching of the adjacent locomotor muscles, changes in the distance between the femur and the corresponding end of the tibia could be observed [28]. The changes in the distance between the two bones would, in turn, be conditioned by several factors: the magnitude of the isometric muscle tension during stretching; the duration and direction of the tension applied; the tendon’s biomechanical properties; and the biomechanical properties of the knee joint (shape, size, viscosity of the synovial fluid, and mechanical properties of the joint capsule elements). Static investigations of knee joint stability are often directed to stretching exercises [28][52][53][54][55][56][28,52,53,54,55,56] and isometric back squats [55]. TheOur study group’s quantitative estimation of the biomechanical processes in human knee joints during active isometric stretching was based on knee joint capsule ultrasound scanning during isometric stretching exercises [28][52][53][56][28,52,53,56]. During a right-lower-limb pose with a 140-degree femur–tibia angle, the distance between the tibia and femur bones forming the knee joint was measured using ultrasound scanning. TheOur experimental model included an ultrasound examination of the knee joint after the isometric stretching of healthy men (n = 10). The changes (in millimeters) in the distances between the femur and tibia were measured with a portable ultrasound system (Vinno 6, China; Figure 1). The apparatus was used for the purposes of theour study in the musculoskeletal mode and in real time with a scanning frequency for the linear transducer of 8 to 10 MHz. The system was able to work in three different upright positions, all with a femur–tibia angle of 140 degrees at rest. In two of the three upright positions, extra loads of 4 and 8 kg were applied vertically down to the lower right limb to induce isometric stretching. Three quantitative parameters—distance up (Dup), distance down (Down), and area (A, cm2)—were measured from the ultrasound pictures (Figure 1). They defined the two displacements (mm) and the area (cm2) between the intra-articular femur and tibia cartilage surfaces.