Ruthenium-106 brachytherapy emits beta radiation (Ru-106 gives off radiation in the form of high energy electrons called beta particles as it decays into rhodium-106 and then into palladium-106, which isn't radioactive) and is used for tumors up to 5 mm in height due to the limited range of radiation penetration, but in some centers, it is used to treat thicker tumors. Therefore, ruthenium is intended for the treatment of small and some medium-sized tumors.
- uveal melanoma
- radiation therapy
- brachytherapy
1. Introduction
Uveal melanoma (UM), is the most common primary intraocular malignancy in adults, with the highest incidence of 5–10 per million Whites per year, . The eyeball is the most common extracutaneous location of melanoma [1][2][3][4][5][6][7][8][1,2,3,4,5,6,7,8]. Usually, it is located in the choroid (90%), and less often in the ciliary body (6%) and iris (4%) [9]. The peak of incidence falls in the sixth to the seventh and, to a lesser extent, the third decade of life [2]. Uveal melanoma metastasizes distantly via blood vessels, most often to the liver (93%), lungs (24%) and bones (16%). It can also spread locally and infiltrate extraocular structures. Extraocular infiltration is associated with a higher risk of distant metastases and worse prognosis. Melanoma metastases are found in most patients at the time of their death [10][11][10,11]. They can even be detected severalmonths to even many years after successful treatment of the primary cancer, which may be associated with their presence, but also the inability to detect them at the time of therapy [1]. The prognosis in patients with confirmed distant metastases is very poor, and the 1- and 3-year survival rates are approximately 21% and 4%, respectively [12]. Unfortunately, there are currently no effective treatments for distant metastases, which are less susceptible to chemotherapy than skin melanoma metastases [13]. Recently, there have been studies presenting therapies with the use of Tebentafusp and giving hope for improving this situation [14]. This bispecific glycoprotein 100 peptide-HLA-directed CD3 T-cell engager was approved by the Food and Drug Administration (FDA) in 2022. for patients with unresectable or metastaticTebentafusp is a breakthrough new therapy indicated for the treatment of HLA-A*02:01–positive adult patients with uveal melanoma that has spread to other parts of the body or can’t be removed with surgery. In the same year, it received a positive response from the European Union Committee for Medicinal Products for Human Use for the treatment of uveal melanoma [15]. UM shows specific chromosomal abnormalities. The most significant is the complete or partial loss of chromosome 3. Other common genetic changes are deletions in 1p, 6q, 8p and 9p, and additions in 1q, 6p and 8q [16]. There have been publications describing familial cases of UM belonging to the familial BAP1-associated cancer predisposition syndrome inherited in an autosomal dominant manner [16][17][16,17].
The treatment uses surgical methods, which include, tumor endoresection (during pars plana vitrectomy) or egzoresection (under tha scleral flap), enucleation, and conservative methods, such as brachytherapy (BT), proton therapy (PT), stereotactic radiotherapy (SRT), stereotactic radiosurgery (SRS), transpupillary thermotherapy (TTT) and photodynamic therapy (PDT) and combined methods. Many factors are taken into account when planning a treatment strategy, including the size of the tumor, its location and the general condition of the patient. Initially, the treatment of choice in uveal melanoma was enucleation. Over time, brachytherapy began to play a dominant role [1][4][18][1,4,18]. The increase in the popularity of brachytherapy was largely influenced by the publication of the results of the Collaborative Ocular Melanoma Study (COMS), which showed the lack of an advantage of enucleation over brachytherapy in terms of distant metastases and survival in the case of small- and medium-sized tumors [3][11][3,19]. In a COMS study, tumor size was defined as follows: small: 1.5–2.4 mm in height and 5–16 mm in diameter; medium: 2.5–10 mm in apical height and ≤16 mm in diameter; and large: >10 mm in apical height and >16 mm in diameter; these terms will be used to describe tumors of these dimensions in the remainder of this article, unless otherwise noted [3,11]. Brachytherapy has gradually become the most commonly used treatment for choroidal melanoma. It involves suturing a plate containing a radioactive isotope to the sclera in the place where the base of the tumor is located. After a few days to inactivate the tumor, the applicator is removed from the sclera [1][19][1,20]. In Europe and Asia, the most commonly used radioactive isotope is ruthenium (106Ru), which emits mainly beta radiation (Figure 1). In North America, iodine (125 I) is dominant, which emits mainly gamma radiation (Figure 2). Less frequently used isotopes are Pd-103, Sr-90, Ir-192, Cs-131, Au-198 and others. There are different sizes (10-25mm diameter) and shapes of plates, e.g., round, or with a notch for the optic nerve, dedicated to the treatment of tumors located close to the optic disc. The time of exposure to radiation is several days and depends on the thickness of the tumor and the activity of the applicator. Treatment planning is carried out using specialized computer systems (Figure 3 and Figure 4) [9][18][19][9,18,20]. Local tumor control, depending on the source of radiation, ranges from 59–98% for ruthenium-106 [20][21] to 76–100% for iodine-125 [21][22]. Brachytherapy can also be combined with other methods, e.g., TTT, and this combination is called “sandwich therapy” [1][18][22][1,18,23]. This method is dedicated especially to tumours located close to the optic disc. TTT, and this combination is called “sandwich therapy” [1][18][22][1,18,23].
a.

b.

Figure 1.
a. and b. Ruthenium-106 applicator.

Figure 2.
Iodine-125 applicator (metal shell and polymer insert with spaces for iodine seeds).
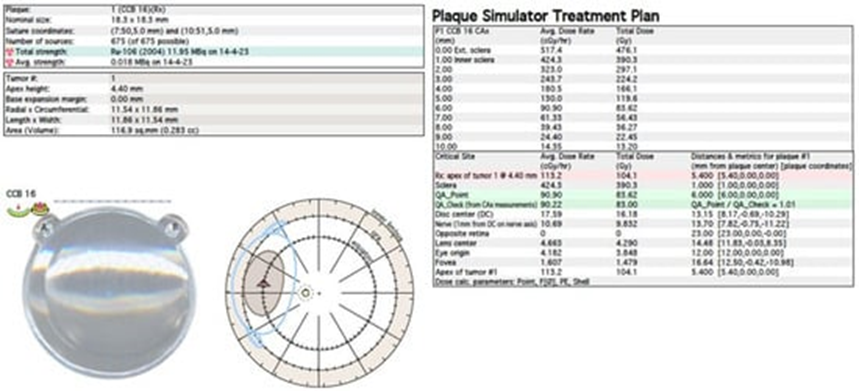
Figure 3.
Ruthenium-106 brachytherapy planning system in Plaque Simulator 6.8.5—planning cards.
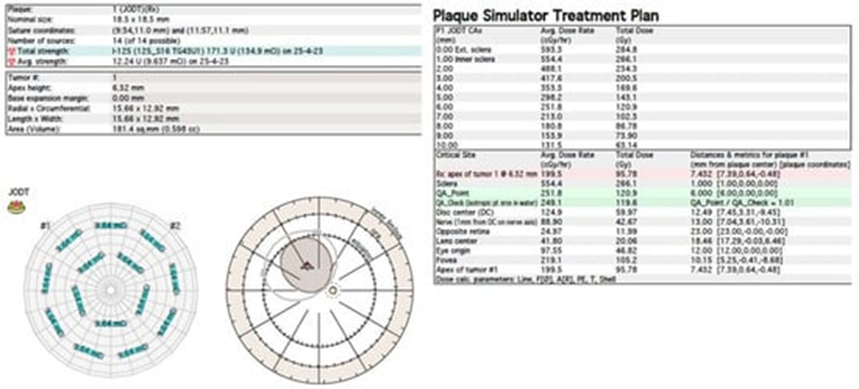
Figure 4.
Iodine-125 brachytherapy planning system in Plaque Simulator 6.8.5—planning cards.
Another method of irradiation is radiation therapy from an external source. Among this group, proton therapy is the most common. It is also much less frequently used method than brachytherapy. It uses a beam of protons, which, owing to the Bragg peak phenomenon, allows the irradiation of the tumor mass to an equal extent while sparing the surrounding healthy tissues. It’s development gave hope for reduction in post-radiation complications and thus better eye function after treatment. Before using this method, the patient first undergoes a surgical procedure of the placement of a few tantalum markers by sutures to the outer sclera to localize the base of the tumor, which is visualized by transillumination. Measurements of the distance between the structures of the eyeball are also performed using ophthalmic imaging techniques, such as magnetic resonance (MRI), ultrasonography (US) and fundus photography. As in the case of brachytherapy, treatment planning is carried out using specialized computer systems (Figure 5) [1][18][19][1,18,20]. Proton therapy has excellent local tumor control of 95% [23][24].
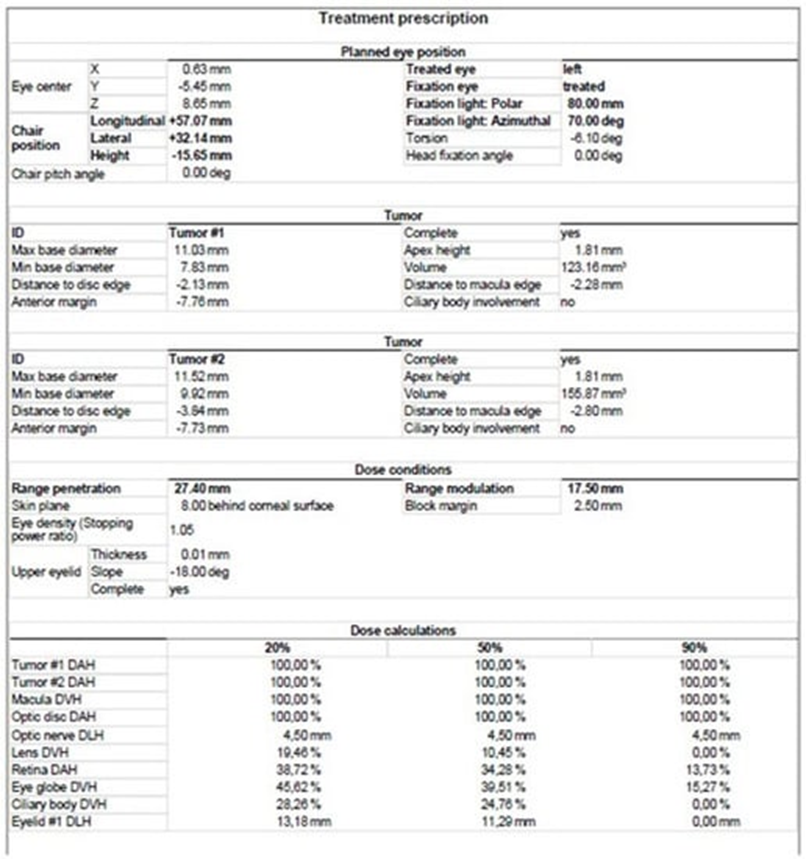
Figure 5.
Proton therapy planning system in Eclipse Ocular Proton Planning version 13.5.01−planning card.
Stereotactic radiotherapy (SRT) and stereotactic radiosurgery (SRS), which also represent external-source radiotherapy, have gained popularity in the treatment of uveal melanoma in recent years. Irradiation of the tumor can be performed in a single session with a high dose of photons (SRS) or in a fractionated form (SRT) [11,20,25,26,27,28]. The main advantages of these methods include their minimal invasiveness, excellent local tumor control, relatively wide availability and low costs [20,25,26,28,29]. Some researchers have indicated their disadvantages in the form of lower precision and the associated higher number of post-radiation complications, mainly secondary glaucoma and enucleation compared with brachytherapy and proton therapy [11,20,30]. Other studies report no significant differences in the rate of complications between these therapies [18].
Most of the studies on choroidal melanoma therapy published so far have focused on comparing patient survival, risk of distant metastases and local tumor control after various treatments. Less attention has been paid to the problem of visual acuity (VA) deterioration after therapy. This is understandable, as the priority is to save the patient’s life. Nevertheless, the deterioration of eye function caused by radiation complications in the form of damage to structures such as the macula, optic disc and lens is a serious problem [9,11]. After brachytherapy, 49% of eyes experienced vision loss within three years and 68% within ten years. In addition, 45% of patients were qualified as blind (20/200 or worse) within three years post-treatment [31].
2. Ru-106 Brachytherapy
Ru-106 brachytherapy emits mainly beta radiation and is used for tumors up to 5 mm in height due to the limited range of radiation penetration, but in manysome centers, it is successfully usused to treat thicker tumors (Figure 6). Therefore, ruthenium is intended for the treatment of small and some medium-sized tumors [19][31][20,32].
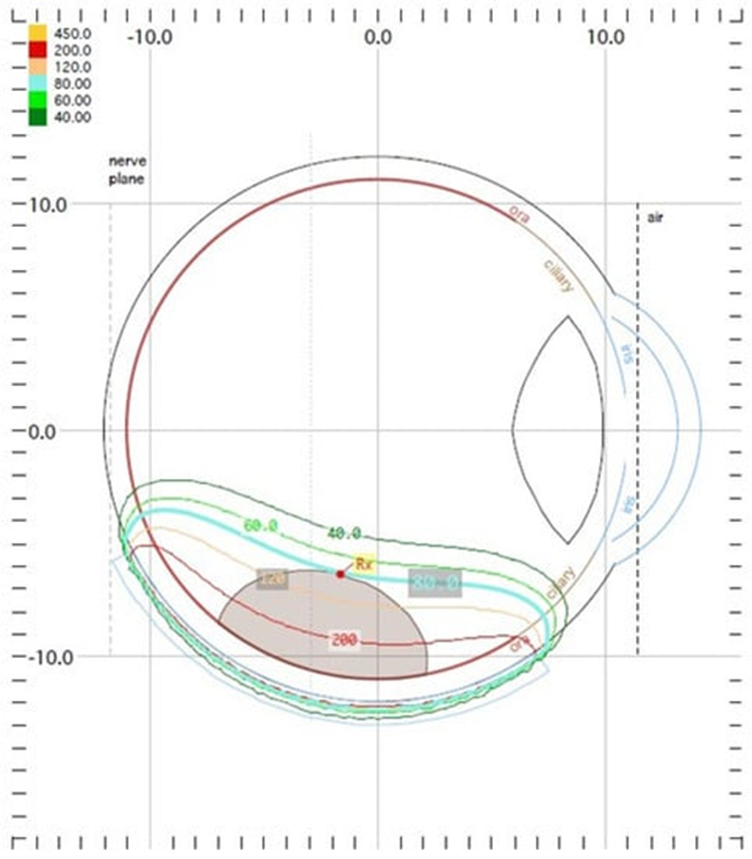
Figure 6. Ruthenium−106 brachytherapy planning system in Plaque Simulator 6.8.5−dose distribution presentation.
Ruthenium−106 brachytherapy planning system in Plaque Simulator 6.8.5−dose distribution presentation.
The use of Ru-106 for thicker tumors was explored by Cennamo et al., who enrolled 350 eyes with small- and medium-sized tumors (measuring up to 6.5 mm in apical height) after Ru-106 plaque brachytherapy for uveal melanoma with a total dose of 100 grays (Gy) to the tumor apex in a retrospective study. Radiation complications were found in 63% of patients: 38% showed radiation maculopathy, 11% had optic neuropathy and 14% developed cataracts. At baseline, the mean best*corrected visual acuity (BCVA) according to the Early Treatment of Diabetic Retinopathy Study (ETDRS) in affected eyes was 0.32 ± 0.30 logarithm of the minimum angle of resolution (logMAR). The mean follow-up was 4 years (3 months to 9 years). The posttreatment BCVA was 0.40 ± 0.25 logMAR. The patients who presented radiation-related complications showed reduced visual acuity (0.7 ± 0.85 logMAR) [33].
Mirshahi et al. conducted a study in which Ru-106 was also used to treat tumors thicker than 6 mm. They analyzed the medical records of 234 patients undergoing Ru-106 plaque brachytherapy for UM. The target dose to the apex was 100 Gy. The median follow up was 54.2 months (range: 6–194.5 months). Visual acuity (logMAR) was 0.673 ± 0.70 at baseline and 0.963 ± 0.80 at the final examination (excluding enucleated eyes). VA was >20/200 at the baseline in 60.3% of patients and at the last examination in 44.2% of patients. VA was >20/40 at the baseline in 28.6% of patients and at the end of follow up in 18.1% of patients. The following radiation complications were found in patients: 108 eyes (46.2%) developed cataracts, and radiation retinopathy was found in 58.1%, radiation maculopathy in 29.9% and radiation neuropathy in 20.1% of patients. Radiation neuropathy was associated with the total scleral dose (B = 0.001, 95% CI: 0.001 to 0.001, p-value = 0.036) and distance to the optic nerve head (B = −0.292, 95% CI: −0.226 to −0.358, p-value <0.001). After adjusting for baseline VA, the final logMAR BCVA was associated with radiation maculopathy and neuropathy, and the rate of legal blindness (BCVA < 20/200) was 44.8%. Interestingly, there was no significant association between the final VA and various tumor dimension and location groups [34].
O’Day et al. decided to assess the long-term visual outcomes after ruthenium plaque brachytherapy for posterior choroidal melanoma. Anterior tumors involving the iris and ciliary body were excluded from this study. A total of 219 patients with choroidal melanoma were treated with ruthenium plaque brachytherapy between January 2013 and December 2015. The baseline visual acuity was ≥6/12 in 168 (76.7%), 6/18–6/60 in 43 (19.6%) and <6/60 in 8 (3.7%) eyes. A dose of 80 (9.1%), 100 (89.5%) or 120 (1.4%) Gy to the apex was prescribed. The median follow up was 56.5 months (12–81 months). The final visual acuity was ≥6/12 in 97 (44.3%) patients, 6/12 to 6/60 in 57 eyes (26.0%) and <6/60 in 55 (25.1%) eyes. Ten (4.6%) eyes were enucleated. The most common radiation complication was radiation maculopathy, which affected 53 (24.2%) patients. Statistical analysis revealed that close proximity to the optic disc and fovea and a large or notched plaque type were associated with poorer final visual acuity (<6/12) upon long-term follow up. A distance of 5.0 mm or more from the optic nerve and fovea was the most significant positive prognostic factor in terms of preservation of vision. The results also showed that using smaller applicators allowed maintaining better vision than using larger ones [35]. However, it should be noted that the reduction in plaque size was limited by the size of the tumor.
