1. Pre-Orthodontic Treatment Care
Typically, patients undergoing orthodontic treatment (OT) often present with oral conditions that require prior clinical care, including dental rehabilitation and management of orofacial pathologies. Laser technology can effectively manage recurrent conditions in the clinical routine. Light therapy can selectively remove carious contaminated tissue, offering an ultra-conservative approach
[1][12]. Additionally, dentin hypersensitivity can be alleviated through light surface treatments. High-power lasers such as Nd:YAG or Er:YAG can reorganize the mineral structure, reducing the movement of tubular fluid, while low-power equipment can stimulate—through photobiomodulation—tertiary dentin formation and provide analgesia
[2][13]. Patients undergoing oral surgeries or experiencing postoperative complications can benefit from both high- and low-power laser treatments, as they can help alleviate pain and promote tissue healing
[3][14]. For patients with painful TMD, PBMT can be beneficial in reducing pain, modulating inflammation, and promoting muscular relaxation
[4][15]. It is important to emphasize that these applications represent a few examples of the many ways in which light therapies can enhance treatments in the general practice of dentistry
[5][4].
2. Pain Control of Orthodontic Activation Responses
Pain response is the most common adverse reaction to OT
[6][16]. It frequently leads to treatment interruption or even reluctance to initiate OT, as patients are concerned about the impact the orthodontic appliance may have on their daily activities
[7][17]. Orthodontic pain is typically associated with tooth discomfort following orthodontic activation, but it can also involve other distressing sensations, such as mucosal ulcers and periodontal lesions caused by the appliances
[8][18].
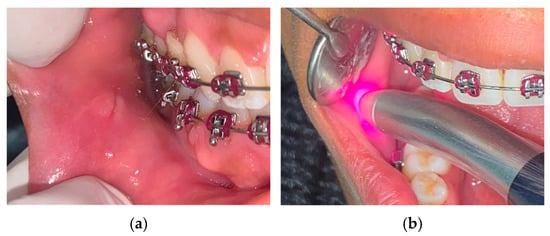
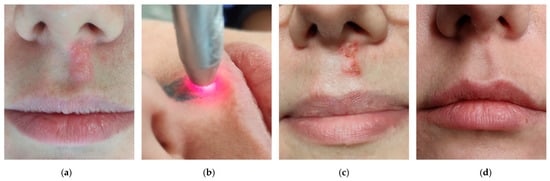
At the onset of treatment, the presence of orthodontic devices in the oral cavity (such as brackets, aligner attachments, or removable appliances) can cause trauma to the oral mucosa, resulting in ulcerations (
Figure 1). An ideal treatment for traumatic ulcers should provide rapid pain relief and optimized tissue repair. Currently, the only therapeutic option that meets these criteria is PBMT. Its mechanism of action involves accelerated extracellular matrix deposition and fibroblast proliferation for tissue repair
[9][19]. Additionally, there is evidence of direct inhibition of pain signaling at the irradiated site, promoting analgesia without any side effects, drug interactions, or age restrictions
[10][20]. Aggarwal et al.
[11][21] demonstrated in a sham-controlled, split-mouth study design that a single session of infrared light PBMT eliminated pain in 93% of patients. Regarding wound healing, a randomized clinical trial (RCT) showed a 70% reduction in the time required for epithelial reconstitution. The current literature supports the superiority of PBMT over topical drug therapy for recurrent aphthous ulcers
[12][13][14][15][22,23,24,25].
Figure 1. Photobiomodulation therapy for traumatic ulcers. (a) Traumatic injury on buccal mucosa associated with the orthodontic appliance. (b) PBMT for analgesia and tissue repair (Laser Duo; MMO, São Carlos, Brazil).
After orthodontic activation (OA), the periodontal ligament initiates a pro-inflammatory cascade to restore tissue dynamics. Vascular changes and the release of neurogenic and pro-inflammatory mediators may trigger local pain [16][26]. The gold standard for pain control after orthodontic procedures is the use of analgesic or anti-inflammatory drugs. However, not all patients accept frequent medication use, and the effects of such pharmaceuticals on tooth movement are controversial [17][27].
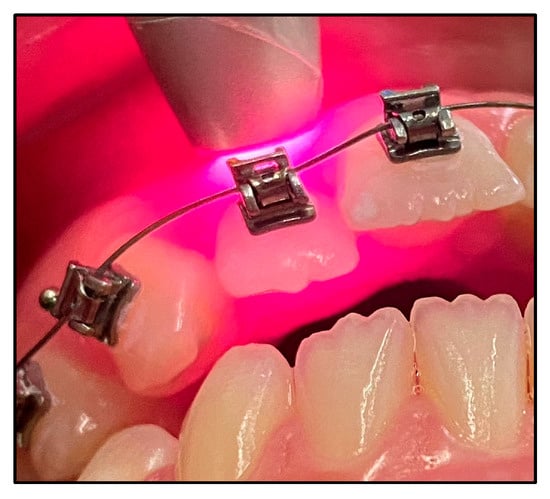
Several studies have shown that PBMT is a non-toxic and effective alternative for pain management after orthodontic activation [18][19][20][21][28,29,30,31]. With just one session of irradiation immediately after orthodontic activation (Figure 2), PBMT can significantly reduce pain sensitivity by altering the depolarization threshold of nerve endings in the periodontal ligament. It also promotes pain relief by modulating the production of pain mediators and stimulating the peripheral release of endogenous endorphins [10][22][23][20,32,33]. PBMT reduces the number of pain signals that reaches the brain and prevents sensitization of central neurons. Brito et al. [18][28] conducted a double-blind RCT and reported that patients who received irradiation after initial alignment arch placement expressed pain relief at 6, 24, 48, and 72 hours compared with controls. This analgesic effect has also been observed with the placement of interdental separators, reducing the need for medication [24][25][34,35].
Figure 2. Photobiomodulation therapy for orthodontic activation pain control.
Photobiomodulation therapy for orthodontic activation pain control.
3. Photobiomodulating Tooth Movement
The duration of orthodontic treatment is a major concern for orthodontic professionals and patients because the appliances have a significant impact on patient quality of life related to oral health [26][36]. Considerable efforts have been made to develop treatments that can facilitate tooth movement, including techniques such as corticectomy and microosteoperforation. Studies conducted in animal and human models have already shown that PBMT is a promising adjunctive tool for improving tooth movement (Figure 3), demonstrating efficacy, safety, and most importantly no side effects [27][28][29][30][31][32][33][34][35][8,10,37,38,39,40,41,42,43].
Figure 3.
Photobiomodulation therapy for orthodontic tooth movement.
Orthodontic mechanics is based on periodontal tissue remodeling through activation of various components such as periodontal fibroblasts, osteoblasts, osteocytes, osteoclasts and vasculature alterations. In vitro and in vivo studies suggest that PBMT promotes cell differentiation, activates osteoclasts and osteoblasts, stimulates collagen synthesis, and promotes angiogenesis, thereby creating a conducive environment for tooth migration [20][30].
One of the papers by Ghaffar et al.
[36][44] investigated the effect of PBMT on the tooth alignment in patients undergoing OT for class I malocclusion correction of 4–10 mm crowding in an RCT. The study found that complete alignment was achieved in an average of 68.2 days in the experimental group compared with 109.5 days in the control group. Thus, PBMT reduced the time required to treat of mild to severe crowding by 37.7%. A split-mouth RCT by Zheng and Yang
[37][45] found that PBMT reduced the time needed for canine retraction by an average of 35% over four weeks. Significant changes in bone remodeling markers, such as decreased OPG levels and increased levels of IL-1β and RANKL, were found in the irradiated side, suggesting that PBMT influences bone turnover and leads to enhanced tooth migration. Systematic reviews claims that PBMT can reduce treatment time by 20-40% without signs of periodontal damage or root resorption
[21][29][30][31][32][33][34][35][31,37,38,39,40,41,42,43].
4. Assisting Tool in Rapid Maxillary Expansion
Rapid maxillary extension (RME) affects not only bony structures but also adjacent soft tissues. Because it relies on bone remodeling, it is a pro-inflammatory treatment, often associated with pain and discomfort
[38][46]. Low-intensity laser light is known for its ability to stimulate osteoclast differentiation and activation, osteoblast proliferation, collagen synthesis, angiogenesis, which, in conjunction with other tissue effects, lead to accelerated bone remodeling, repair, and maturation (
Figure 4)
[39][47].
Figure 4.
Photobiomodulation therapy during rapid maxillary expansion.
Sasaki et al.
[40][48] showed in an RCT that the PBMT group experienced an acceleration of the opening process of the midpalatal suture, beneficial to prevent unwanted dental side-effects. Cepera et al.
[41][49] studied the influence of PBMT on palate bone density in patients undergoing RME. The authors observed that patients who underwent twice-monthly PBMT after achieving adequate screw activation showed optimized bone density recovery during the retention period. PBMT stimulates bone formation and minimize treatment relapse. Several authors have discussed the potential use of PBMT to reduce the time required for maxillary bone consolidation
[42][43][44][50,51,52]. However, further research is needed to support the reduction in the RME-retention phase.
5. Postoperative Care with Lasers
Photobiomodulation can significantly improve the postoperative phase of surgical procedures such as tooth extraction, orthognathic surgeries, or other that may lead to complications and impact the quality of life of patients.
The immediate postoperative period is usually associated with inflammatory symptoms, such as swelling, pain, and decreased mandibular function. PBMT not only modulates the inflammatory course, but also promotes analgesia, and tissue repair [45][46][53,54].
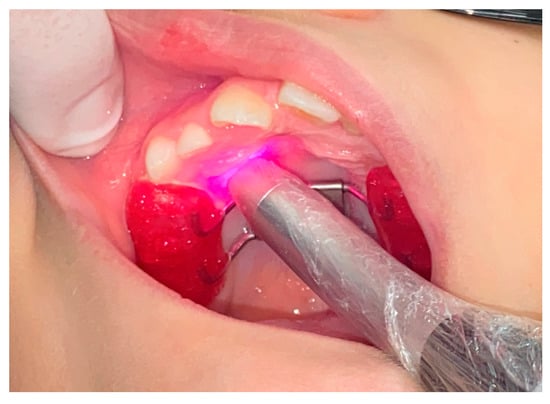
Eshghpour et al. [47][55] demonstrated the effectiveness of PBMT in alleviating pain and edema after the removal of impacted third molars in a split-mouth RCT (Figure 5). Domínguez Camacho et al. [48][56] defends that PBMT is an important adjunct to oral anti-inflammatory drugs to reduce post-surgical edema in orthognathic surgery patients. Feslihan and Eroğlu [49][57] states that PBMT is an alternative to corticosteroids after impacted third molar surgery, as it has similar clinical efficacy in controlling pain, swelling, and trismus. Considering the side effects of anti-inflammatory drugs, PBMT has increasing relevance to modern dentistry [50][51][52][53][58,59,60,61].
Figure 5. Photobiomodulation therapy for postoperative care. (a) One day after impacted 38 extraction, first session of PBMT. (b) Three days after surgery, second session of PBMT. (c) Seven days after surgery, zero discomfort reported.
Photobiomodulation therapy is highly recommended to treat paresthesia and paralysis, one of the most persistent complications after major orofacial surgery. With the appropriate parameters, laser light helps restore neurosensory function by optimizing regeneration of peripheral axons and promoting sprouting of adjacent new nerve endings [46][54]. Oliveira et al. [4][15] noted that the success rate of PBMT in nerve repair depends on the time interval from nerve injury to initiation of treatment. Considering that the orthodontist determines the appropriate surgical time for each case during her OT, it is important that the professional also schedules PBMT sessions to ensure the patient's optimal recovery.
6. aPDT to Manage Infections during Orthodontic Treatment
Infections are relatively common during OT because proper hygiene is difficult to maintain due to the presence of orthodontic appliances. It is estimated that about 15% of orthodontic patients experience complications that require professional intervention. In the United States alone, this costs over $500 million annually and requires the equivalent of 1,000 full-time dentists
[54][62]. Oral infections during OT can cause significant discomfort, pose risks to the patient's overall health, and interfere with the OT chronogram. An interesting approach to treat infectious complications is the aPDT due to its technical ease, efficacy against a wide range of microorganisms (including bacteria, viruses and fungi) and non-inducible antimicrobial resistance properties. In aPDT, a photosensitizer is applied to the affected area and activated with specific wavelengths of light. This process triggers reactions that generate sufficient amounts of reactive oxygen species to reduce pathogens without host toxicity
[55][63]. Multiple indications for aPDT include herpes labialis (
Figure 6), periodontal disease, gingival abscess, endodontic lesions, alveolar inflammation, peri-implantitis, halitosis, angular stomatitis, candidiasis, vitiligo, deep caries, and others
[56][9].
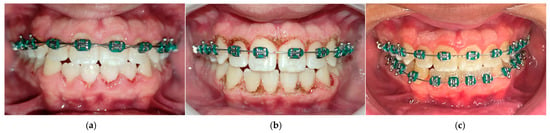
Figure 6. Photodynamic therapy for herpes labialis. (a) Second day of manifestation, scab formation. (b) aPDT.with methylene blue and low-level red laser irradiation. (c) One day after aPDT, crusting phase. (d) Five days after aPDT, completely healed.
Baeshen et al.
[57][64] performed a comprehensive analysis of the impact of aPDT on treating periodontal disease in patients undergoing OT with retainers. When aPDT was performed in conjunction with dental scaling, significant improvements were seen in clinical parameters such as gingivitis, bacterial populations, pro-inflammatory cytokines and pain perception. In an RCT, Alshahrani et al.
[58][65] showed that aPDT is also a viable treatment option for adolescents with halitosis during OT. Combined with the tongue-scratching technique, aPDT effectively reduced the concentration of hydrogen sulfide and oral pathogens. Regarding the incidence of herpes labialis, de Paula Eduardo et al.
[59][66] found that aPDT could effectively reduce the viral titer during the vesicular stage, suggesting that OT could be safely conducted in the same day of the aPDT treatment. The authors also highlighted the potential of the implementation of PBMT to reduce the frequency and severity of recurrent herpetic lesions
[60][67]. Similar to various medical specialties, aPDT has proven to be an excellent tool to control oral infections as it not only provides local antisepsis but also promotes pain relief and stimulates tissue repair.
[56][9].
Given the increased risk of tissue laceration and opportunistic infections during OT, it is of utmost importance to take effective measures to control pathogenic complications, especially during OT. As the literature continues to evolve, aPDT is increasingly recognized as a simple and effective technique to restore oral health and improve quality of life for OT patients
[56][61][62][63][64][9,68,69,70,71].
7. Soft Tissue Management with High-Intensity Lasers Complementing Orthodontic Therapy
High-intensity lasers are a valuable aid in supporting OT and improving outcomes. This technique offers an excellent surgical option for orthodontic patients because it promotes hemostasis during surgery, significantly reduces microbial load, and modulates surrounding tissue to facilitate repair
[65][72].
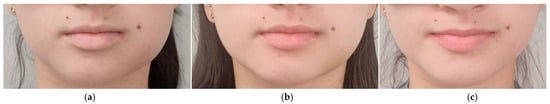
Currently, high-intensity diode and Er:YAG lasers are two of the most commonly selected laser devices for surgical purposes in dentistry
[65][72]. High-intensity diode lasers (800-980 nm) preferentially interact with pigmented tissue, which is primarily absorbed by melanin. When used properly, it penetrates the oral mucosa well without damaging teeth and bones. High-intensity diode lasers are used for gingivectomy, surgical access to impacted teeth, removal of hypertrophic tissue (often caused by orthodontic appliances), contouring of the gingival margin to facilitate bracket attachment (
Figure 7), frenectomy, and gingival depigmentation
[66][67][68][69][73,74,75,76]. On the other hand, the Er:YAG laser (2,940 nm) is strongly absorbed by water and hydroxyapatite. Therefore, it can be used not only for bracket removal in orthodontic patients, but also for osteotomy when accessing impacted teeth
[70][77]. The clinical application of these kind of lasers is based on the photoablation phenomenon: the absorbed light causes rapid evaporation, increasing internal pressure and triggering 'microexplosions' that lead to superficial removal of the irradiated material. Erbium lasers can also be used for soft tissue incisions. However, special attention should be paid to bleed control
[71][78]. Since these devices raise the temperature, they are also very useful for decontaminating infectious processes such as herpetic lesions
[59][66].
Figure 7. Gingival recontouring to facilitate appliance bonding. (a) Pre-gingivectomy. (b) Immediate post-op with high-intensity diode laser. (c) One month after surgery, fixed orthodontic device fully installed.
From a minimally invasive procedure perspective, orthodontists should consider incorporating high intensity laser technology into their clinical routine. By understanding the properties of different light sources and having the appropriate technical training, orthodontists can use lasers to effectively treat both soft and hard tissue, to achieve minimal side effects and make the postoperative period more comfortable for the patient.
8. Braces Removal with the Touch of Light
The removal of orthodontic appliances is traditionally performed using orthodontic pliers, which apply mechanical force to break the adhesion between the appliance and the tooth surface. However, this method can be uncomfortable for the patient and may result in cracks and fractures in the enamel
[72][79]. Therefore, there is a need for alternative methods that allow for the safe removal of appliances without causing damage to the enamel and premature aging of teeth.
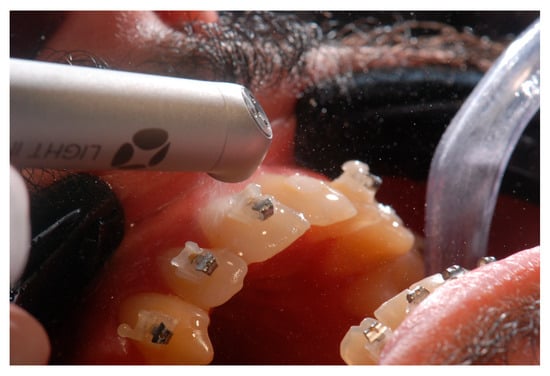
High-intensity lasers offer an effective and safe technique for appliance removal. By using the appropriate parameters, the bond strength can be decreased, facilitating the detachment of orthodontic accessories. Various types of lasers, such as diode, Nd:YAG, CO
2, Er:YAG, and Er,Cr:YSGG, have been described for bracket debonding
[73][80]. In the thermal softening process, the bonding agent is heated until it softens, allowing the bracket to slide off the tooth surface. Diode lasers are currently more affordable, but caution must be exercised due to temperature increase (which can cause pulp damage), since they do not require water spray
[74][81]. The most commonly used lasers for bracket removal are those that act through photoablation, such as erbium lasers (
Figure 8). In photoablation, when the light is absorbed by the orthodontic adhesive, there is a sudden vaporization of the hydroxyl group present in the composite material, resulting in a reduction in shear bonding strength
[48][56]. This process enables the spontaneous detachment of brackets or allows for their removal using college tweezers, eliminating the need for pliers. This procedure is more comfortable for the patient and preserves the enamel structure. Although laser bracket removal is a promising and effective method, it may not be the most practical or cost-effective option for most orthodontists due to limited access to the necessary equipment
[73][75][76][77][78][80,82,83,84,85].
Figure 8.
Ceramic bracket removal with an erbium laser (LiteTouch; Light Instruments, Yokneam, Israel).
The technological revolution witnessed in recent decades has led to unprecedented scientific advancements in dentistry. It is crucial to raise awareness among orthodontists regarding the benefits that laser procedures can offer to OT and the oral health of patients. By utilizing efficient, safe, and comfortable therapeutic procedures, it becomes possible to enhance dental aesthetics and functionality, thereby improving the overall health and quality of life of the population.