Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Marwan Habiba and Version 2 by Jessie Wu.
Both endometriosis and adenomyosis are often referred to as “enigmatic diseases” since understanding their pathogenesis remains elusive. Both endometriosis and adenomyosis are relatively common among women of reproductive age and are leading causes of pelvic pain, infertility, and menstrual disorders. They impact negatively on patients’ quality of life, productivity, and well-being. Endometriosis, and perhaps adenomyosis as well, entails a heavy economic burden to society as a whole.
- adenomyosis
- archimetra
- archimetrosis
- archimetrium
- endometriosis
- pathogenesis
- tissue injury and repair
1. Structural Aspects
There is evidence that the myometrium is not uniform. The orientation of the muscle fibers in the uterus has been reported to vary from the innermost layers, where the muscle direction is mostly circular, to the interconnected crisscross middle and main layer of the uterus. Leyendecker and co-workers referred to the main component (the middle layer) layer as the stratum vasculare [1][20]. This separates the subserosa (the outermost layer) or the stratum supravasculare from the innermost layer, which they referred to as the stratum subvasculare. However, the boundaries between these layers are not defined histologically [1][20]. Structural studies have shown that the transition in the myometrial layers is gradual, with no discernable histological demarcation between the inner and outer zones [2][21]. As an example, the concept of the junctional zone that designates the endometrium–myometrium interface (EMI) is based on MR imaging [3][22], not on histologically identifiable features. The classic studies of uterine vasculature, such as those reported by Sampson, show that the rich vascular network of anastomosis that contains the arcuate arteries lies between the outer and middle third of the myometrium [4][5][6][23,24,25]. Blood vessels run medially from that network to supply the myometrium and terminate by supplying the endometrium. Based on its vasculature, Sampson divided the myometrium into three zones: the peripheral or outer third, which is supplied by the peripheral arteries; the arcuate zone, which is the narrow area containing the main vessels; the radial zone, which corresponds to the inner two-thirds of the myometrium, supplied by the radial vessels. This vascular distribution is at variance with the description of the stratum vasculare as forming the main bulk of the myometrium.
Leyendecker et al. [7][26] proposed to designate as “archimetra” the endometrial–subendometrial region together with the main bulk of the muscle layer (the stratum subvasculare) and the term “neometra” to be applied to the outer layers of the myometrium. They argued that only the archimetra is of paramesonephric origin and that the neometra is of non-Müllerian origin. However, a different embryonic origin is difficult to substantiate. It is commonly accepted that the mesonephric (Wolffian) duct first develops from the intermediate mesoderm and is critical to the development of the paramesonephric (Müllerian) duct [8][9][27,28]. Epithelial cells of the Müllerian duct develop adjacent to the rostral mesonephric epithelium as invaginations of the coelomic epithelium [10][29]. The mesenchyme that surrounds the Müllerian duct epithelium is derived from mesonephric (Wolffian) mesenchyme and coelomic epithelial cells localized along the length of the mesonephros [11][12][30,31]. Thus, the myometrial layers in the context of “archimetra” and “neometra”, as depicted by Leyendecker et al. [1][20], are at direct odds with that depicted by Sampson [5][24].
There is also evidence that the inner myometrium can develop from endometrial stroma and of the potential existence of smooth muscle metaplasia, i.e., endometrial stromal cells can be coaxed to transdifferentiate to smooth muscle cells [13][14][15][32,33,34]. These findings suggest that the whole myometrium shares a common embryonic origin. It is also well-recognized that adenomyosis is not confined to the inner or to the mid-myometrial layers. Both observations challenge the view that endometriosis and adenomyosis are diseases of “archimetra”.
The archimetra theory is partly based on the work of Werth and Grusdew [16][35], who reported on the features of uterine development from the fetal stage to maturity. This researchtudy included five samples from the end of the third month to the fifth month of gestation. This publication, however, does not contain any claims as to the mesonephric/paramesonephric origin of the myometrium. Interestingly, the authors observed that comparative studies with other species (which they referred to as “genetic studies”, employing the terminology used at the time) add little, if any, to our understanding of the mature human uterus [16][35].
Two additional publications adopted the notion that adenomyosis and endometriosis are “diseases of archimetra” [17][18][36,37]. However, neither of these studies added any original information to support the archimetra hypothesis beyond the TIAR theory.
It has been recently suggested that the stratum vasculare in humans constitutes the main musculature of the uterus and that its (hyper)-contraction manifests as primary dysmenorrhea and leads to uterine injury and also the expulsion of the basal endometrium and the development of endometriosis [19][5]. In support of this hypothesis, it was proposed that the human uterine structure is unique [19][5]. However, there are considerable similarities between the structure of the myometrium in the mouse and the human [20][38]. While it is plausible that the mesh-like structure of the middle layer of the human myometrium evolved secondarily to the fusion between the Müllerian ducts, recent research using three-dimensional reconstruction of the mouse uterus identified a middle myometrial layer that connects the inner circular and the outer longitudinal muscle layers in the bicornuate uterus [21][39]. This finding is critical as it demonstrates that the three-layer myometrium is not unique to Haplorrhines (one of the two suborders of primates, which includes monkeys, apes, and humans) but that it is also shared with some Euarchontoglires (a superorder of mammals, also called “supraprimates”, that includes rodents. See Figure 1). This raises doubt about the proposed notion that the human myometrial structure played a unique role in primate evolution [19][5].
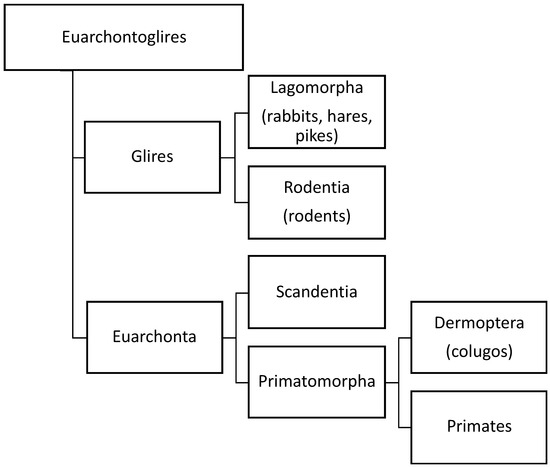
Figure 1. Orders of different species based on our current knowledge of evolution of species. Three-layer myometrium is not unique to Haplorrhines (one of the two suborders of primates, which includes monkeys, apes, and humans), but it is also shared with other Euarchontoglires (a superorder of mammals, also called “supraprimates”, that includes rodents. Adapted from Wikipedia (https://en.wikipedia.org/wiki/Euarchontoglires, accessed on 10 January 2023).
On the other hand, it is not clear whether there is a causal link between myometrial structure and menstruation, and there is no direct information available to compare the myometrium in the majority of mice species, which do not menstruate and the Egyptian spiny mouse (Acomys cahirinus), the only mouse species known to menstruate spontaneously. Thus, the claim that the human uterine structure is unique needs to be substantiated, particularly given that adenomyosis does occur spontaneously in the animal kingdom [22][40]. Furthermore, endometriosis also occurs spontaneously in primates, such as baboons [23][41] and cynomolgus monkeys [24][42], as well as in mice with oncogenic mutations [25][43]. In other words, the putative uniqueness cannot be used as a justification for the hypothesis.
