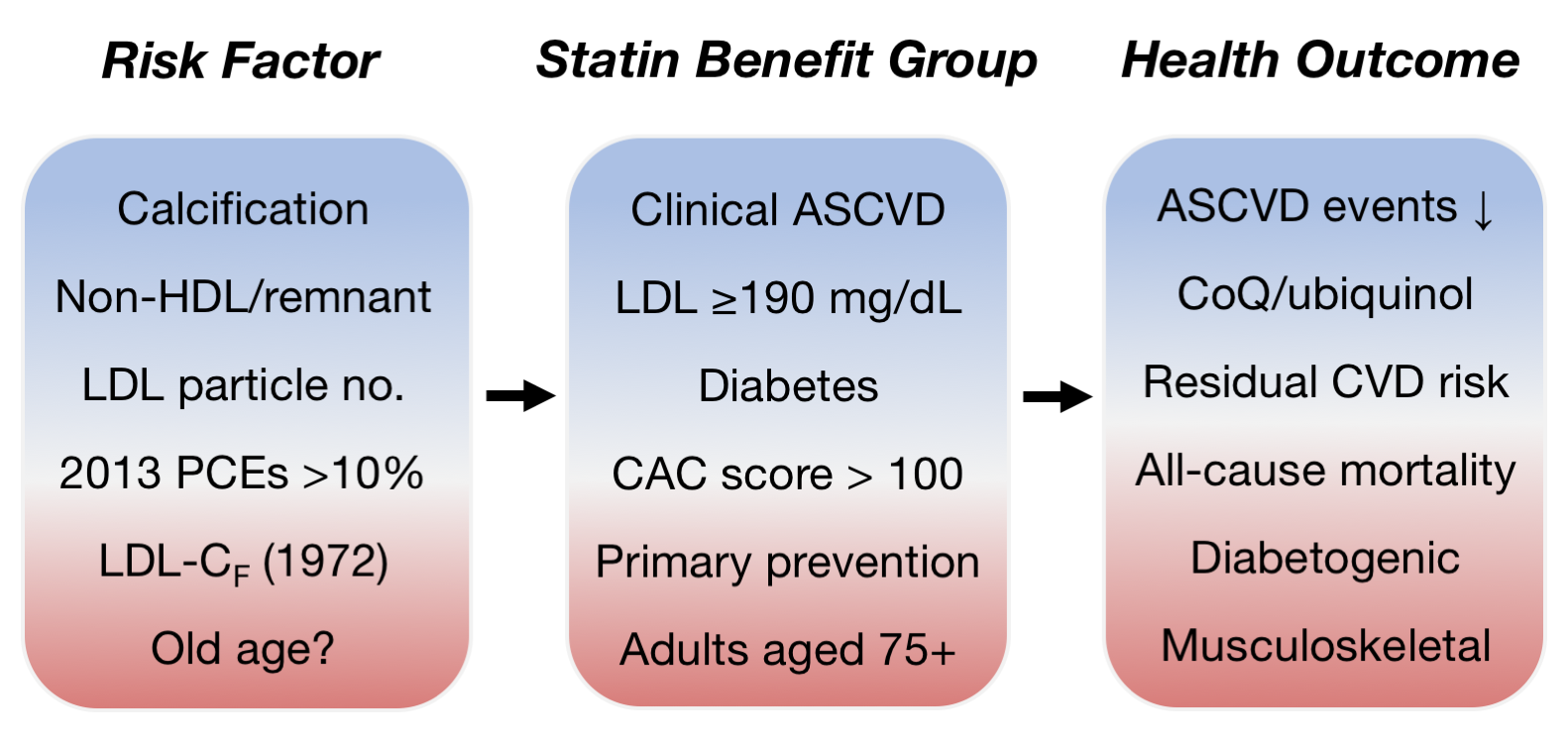
Ample evidence supports the use of statin therapy for secondary prevention in patients with a history of atherosclerotic cardiovascular disease (ASCVD), but evidence is wanting in the case of primary prevention, low-risk individuals, and elderly adults 65+. The efficacy of statins can be contrasted for distinct subsets of patients based on age, diabetes, ASCVD, and coronary artery calcium (CAC) status. Most cardiovascular risk calculators heavily weight age and overestimate one’s absolute risk of ASCVD, particularly in very old adults. Improvements in risk assessment will enable the identification of specific patient populations that benefit most from statin treatment. Derisking is particularly important for adults over 75, in whom treatment benefits are reduced and adverse musculoskeletal effects are amplified. The CAC score stratifies the benefit effect size obtainable with statins, and CAC > 100 can be regarded as a significant patient benefit group. Robust biomarkers, improved risk estimator tools, and personalized, evidence-based approaches are needed to optimally reduce cardiovascular events and mortality rates through administration of cholesterol-lowering medications.
- cardiovascular disease
- statins
- primary prevention
- geriatrics
1. Introduction
Atherosclerotic cardiovascular disease (ASCVD), a leading cause of morbidity, accounts for 1 in 3 deaths in U.S. adults. Statin drugs inhibit the body’s endogenous synthesis of cholesterol, lowering plasma levels of low-density lipoprotein cholesterol (LDL-C). Statins have become a mainstay in the primary prevention and treatment of existing ASCVD, and are now one of the most commonly prescribed drugs in the world. From 2002 to 2013, statin use among US adults 40 years and older almost doubled, from 22 to 39 million adults, or 28% of the population. The Medical Expenditure Panel Survey found that statin use for primary ASCVD prevention in adults 80 years and older increased four-fold, from 9% in 1999 to 34% in 2012. The 2013 American College of Cardiology/American Heart Association (ACC/AHA) guidelines for the management of blood cholesterol identified 13 million Americans as newly eligible for consideration statin therapy based on a 10-year ASCVD risk ≥7.5%, which is a lower threshold compared to other international guidelines. Given the potential adverse effects of statin use, recent meta- and post-hoc analyses have attempted to address whether available clinical evidence supports such widespread use, particularly in low-risk individuals.
Early statin trials excluded elderly patients, and less evidence exists overall for the efficacy of statins in older adults. While no randomized controlled trials (RCTs) have been conducted using statins in patients older than 80 years at baseline, the independent STAREE (NCT02099123) and PREVENTABLE (NCT04262206) trials are currently assessing high intensity statin therapy compared to placebo in adults 70+ and 75+, respectively. Most meta-analyses of statin use to date have included participants for both primary and secondary prevention, with fewer adults over 65 being represented. To balance the potential benefits and harms from statin therapy, efficacy must be compared across different patient groups of varying cardiovascular risk.
2. Statin Efficacy in Elderly Patients
2.1. Primary Prevention of ASCVD
Ponce et al. performed a comprehensive meta-analysis of 23 RCTs comprising 60,194 patients aged 65+[1]. Cohort data was collated for each of five patient groups: ages 65–75, ages 75 and over, patients with diabetes, patients without diabetes, and patients with hypertension. For primary prevention in those with no history of ASCVD, statin use was found to reduce the risk of coronary artery disease [CAD; relative risk (RR): 0.79, 95% confidence interval (CI): 0.68–0.91] and myocardial infarction (RR: 0.45, 95% CI: 0.31–0.66) relative to placebo in all patient groups. However, Forest plot analysis revealed that statins did not significantly reduce the risk of heart failure (RR: 1.04, 95% CI: 0.80–1.35), all-cause mortality (RR: 0.95, 95% CI: 0.84–1.07), or cardiovascular mortality (RR: 1.01, 95% CI: 0.83–1.24) overall or in any patient group. The one RCT of adults ≥75 reported an increase in all-cause mortality for 40 mg/day pravastatin vs. usual care [hazard ratio (HR): 1.34, 95% CI: 0.98–1.84].
Other meta-analyses of primary prevention in the elderly have similarly reported statistically significant RR reductions for ASCVD events but not mortality rates. A meta-analysis of JUPITER and HOPE-3 cohorts aged 65–69 and 70+ by Ridker et al. found non-significant reductions in all-cause mortality[2]. An earlier meta-analysis was performed of 24,674 adults 65+ spanning 8 RCTs as a single cohort (mean age 73 ± 2.9 years)[3]. Statins significantly reduced the rate of myocardial infarction and stroke but not all-cause or cardiovascular mortality. These findings support the conclusion that the benefits of statin therapy are less than maximal in elderly (65+) patients for primary prevention. The weakening dependence of mortality on cholesterol levels at ages over 60 is one explanation for the abatement of statins in extending elderly lifespan.
2.2. Primary Prevention in Very Old Diabetes Patients
Limited placebo-controlled RCT data is available for elderly patients with diabetes and very old adults aged 75+. Ramos et al. conducted a retrospective study of 46,864 participants 75 years and older with no history of ASCVD for a median follow-up of 5.6 years[4]. To prevent survivor bias and covariate measurement bias, a new-user study design was employed in which new statin users were selected for rather than all statin users. A Cox proportional hazards model was used to calculate the HRs of statin use for outcome events. In patients with diabetes aged 75–84, statins were modestly effective in reducing ASCVD [HR: 0.76, 95% CI: 0.65–0.89; 1-year number needed to treat (NNT): 164] and all-cause mortality (HR: 0.84, 95% CI: 0.75–0.94; NNT: 306). The reduction in ASCVD began to lose statistical significance at age 85 and disappeared completely at age 92. The protective effect of statins against all-cause mortality began to lose significance at age 82 in patients with diabetes and disappeared definitively at age 88. In patients without diabetes, statins did not reduce the risk of ASCVD, stroke, CHD, or all-cause mortality for the age groups 75–84 and 85+. Note that under current cholesterol guidelines, most of this population would be eligible for statin treatment, having a 10% risk of ASCVD at 10 years.
2.3. Secondary Prevention of ASCVD
Ponce et al. assessed the effect of statins in the treatment of patients diagnosed with clinically significant ASCVD[1]. RCTs were collected for two patient populations, adults aged 65–75 and patients without diabetes. In contrast to primary prevention, high-certainty evidence was obtained for the use of statins in adults 65 and over for secondary prevention of ASCVD. Compared to placebo, statins decreased the risk of all-cause mortality (RR: 0.80, 95% CI: 0.73–0.89), cardiovascular mortality (RR: 0.68, 95% CI: 0.58–0.79), CAD (RR: 0.68, 95% CI: 0.61–0.77), and myocardial infarction (RR: 0.68, 95% CI: 0.59–0.79). However, evidence was less conclusive for heart failure (RR: 0.79, 95% CI: 0.59–1.06) and stroke (RR: 0.90, 95% CI: 0.79–1.02). No separate data on subgroups, such as those specifically over 75 years of age or patients with type 2 diabetes, was available from the eight trials reviewed.
In 2020, a meta-analysis was performed based on 17 RCTs in elderly patients 65+ for primary or secondary prevention[5]. The substantial statin benefits obtained for secondary prevention closely match the findings of Ponce et al. for ASCVD events and mortality rate. Also in agreement with Ponce et al., in primary prevention statins were observed to significantly reduce the rate of myocardial infarction but not all-cause or cardiovascular mortality.
3. Perspective and Conclusions
Statins are increasingly prescribed using a treat-all approach to prevent ASCVD. The broadening of diagnostic criteria in recent decades has led to their use in low-risk and elderly individuals, dramatically altering the absolute risk reduction and NNT obtained for cardiovascular events and mortality outcomes. Current clinical guidelines emphasize identifying a patient’s family history of dyslipidemia. After excluding familial hypercholesterolemia, however, LDL-C or triglycerides > 90th population percentile associate similarly with CAD risk regardless of family history. Maximal reduction in LDL-C has long been the target of statin therapy. The 2013 ACC/AHA guidelines referenced an oft-cited 28% reduction in RR for ASCVD events per 1 mmol/L (39 mg/dL) reduction in LDL-C. In contrast, a recent meta-analysis of intensive statin therapy for primary and secondary prevention combined found a modest reduction in RR for cardiovascular mortality of 14% for adults whose baseline LDL-C was ≥100 mg/dL[6]. For ASCVD events, all-cause mortality and cardiovascular mortality, the risk reductions reported by the individual RCTs were highly sensitive to the study baseline LDL-C level.
Despite widespread use, current evidence on the benefit effect size does not support the use of statins for primary prevention in very old adults, in whom the significance of adverse effects is amplified. The U.S. Preventive Services Task Force concluded that the evidence does not support statin therapy for primary prevention of ASCVD in adults over 75[7]. The AGREE II instrument was recently used to evaluate 33 international guidelines for ASCVD prevention[8]. Only 18 guidelines were found to provide instructions for discontinuation of statins, which were related to general intolerance or poor health rather than age status. Their findings underscore the lack of a deprescribing tradition and the growing reliance of practice guidelines on low-level evidence and expert opinion.
References
- Oscar J Ponce; Laura Larrea-Mantilla; Bianca Hemmingsen; Valentina Serrano; Rene Rodriguez-Gutierrez; Gabriela Spencer-Bonilla; Neri Alvarez-Villalobos; Khaled Benkhadra; Abdullah Haddad; Michael R Gionfriddo; et al. Lipid-Lowering Agents in Older Individuals: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. The Journal of Clinical Endocrinology & Metabolism 2019, 104, 1585-1594, 10.1210/jc.2019-00195.
- Paul M Ridker; Eva Lonn; Nina P. Paynter; Robert Glynn; Salim Yusuf; Primary Prevention With Statin Therapy in the Elderly. Circulation 2017, 135, 1979-1981, 10.1161/circulationaha.117.028271.
- Gianluigi Savarese; Antonio M. Gotto; Stefania Paolillo; Carmen D'amore; Teresa Losco; Francesca Musella; Oriana Scala; Caterina Marciano; Donatella Ruggiero; Fabio Marsico; et al. Benefits of Statins in Elderly Subjects Without Established Cardiovascular Disease. Journal of the American College of Cardiology 2013, 62, 2090-2099, 10.1016/j.jacc.2013.07.069.
- Rafel Ramos; Marc Comas-Cufí; Ruth Martí-Lluch; Elisabeth Balló; Anna Ponjoan; Lia Alves-Cabratosa; Jordi Blanch; Jaume Marrugat; Roberto Elosua; María Grau; et al. Statins for primary prevention of cardiovascular events and mortality in old and very old adults with and without type 2 diabetes: retrospective cohort study. BMJ 2018, 362, k3359, 10.1136/bmj.k3359.
- Chuannan Zhai; Kai Hou; Rui Li; Yuecheng Hu; Jingxia Zhang; Yingyi Zhang; Le Wang; Rui Zhang; Hongliang Cong; Efficacy of statin treatment based on cardiovascular outcomes in elderly patients: A standard meta-analysis and Bayesian network analysis. Journal of International Medical Research 2020, 48, 300060520926349, 10.1177/0300060520926349.
- Eliano Pio Navarese; Jennifer G. Robinson; Mariusz Kowalewski; Michalina Kolodziejczak; Felicita Andreotti; Kevin Bliden; Udaya Tantry; Jacek Kubica; Paolo Raggi; Paul A. Gurbel; et al. Association Between Baseline LDL-C Level and Total and Cardiovascular Mortality After LDL-C Lowering. JAMA 2018, 319, 1566-1579, 10.1001/jama.2018.2525.
- US Preventive Services Task Force; Kirsten Bibbins-Domingo; David C. Grossman; Susan J. Curry; Karina W. Davidson; John W. Epling; Francisco A. R. García; Matthew W. Gillman; Alex R. Kemper; Alex H. Krist; et al. Statin Use for the Primary Prevention of Cardiovascular Disease in Adults. JAMA 2016, 316, 1997-2007, 10.1001/jama.2016.15450.
- Milly A. Van Der Ploeg; Carmen Floriani; Wilco P. Achterberg; Jonathan M.K. Bogaerts; Jacobijn Gussekloo; Simon P. Mooijaart; Sven Streit; Rosalinde K.E. Poortvliet; Yvonne M. Drewes; Recommendations for (Discontinuation of) Statin Treatment in Older Adults: Review of Guidelines. Journal of the American Geriatrics Society 2019, 68, 417-425, 10.1111/jgs.16219.