2. Antioxidants
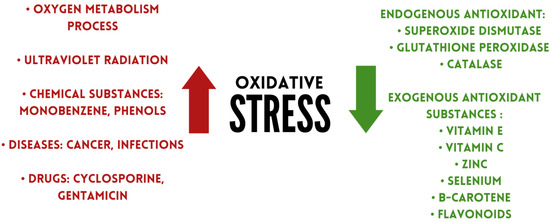
Antioxidants are substances that can remove damage caused by oxidative stress, or prevent or delay it
[14][41]. Under physiological conditions, antioxidants regulate the production of free radicals
[15][42]. Based on their occurrence, antioxidants can be divided into two groups: endo- and exogenic. The first group includes superoxide dismutase, glutathione peroxidase, catalase. Exogenous antioxidants include flavonoids, vitamins, and minerals, among others (
Figure 1)
[16][43].
2.1. Exogenous Antioxidant Substances
2.1.1. Vitamin E
Vitamin E comprises four tocopherols (α, β, γ, δ) and four tocotrienols (α, β, γ, δ). The antioxidant properties of α-tocopherol are comparable to α-tocotrienol
[17][44]. A-tocopherol is the best bioavailable form of vitamin E due to α-tocopherol transfer protein (α-TTP), which has a 100% affinity for α-tocopherol and is the main determinant of α-tocopherol concentration in plasma
[18][45]. Vitamin E can modulate prostaglandin E2 (PGE2) production
[19][46]. PGE2 is involved in enhancing cytokine signalling through gene regulation. It also facilitates Th1 differentiation and Th17 expansion
[20][47]. Additionally, it promotes the production of IL-22 by Th22 cells. In contrast, the improvement of PGE2 inflammation occurs mainly through EP2 and EP4 receptors
[21][48].
L-ascorbic acid is a compound that is not synthesised in the human body, so it must be supplied from exogenous sources. Vitamin C exhibits immunomodulatory and protective effects against ROS
[22][57]. It can have a protective effect on the endothelium, among other things, by decreasing ROS in endothelial cells or neutralising the nitrate tolerance phenomenon
[23][58]. It can act as a cofactor for mono and dioxygenase enzymes
[24][25][59,60]. The hydroxyl groups of ascorbate in the lactate ring are electron donors and proton donors; they convert to the diketone moiety of dehydroascorbate (DHA), and therefore have a protective effect on cells. Such action of hydroxy groups is shown against superoxide radicals, singlet oxygen, and hydrogen peroxide
[26][61]. Due to molecular stabilisation, the resulting ascorbyl radical is hardly reactive
[27][62]. A high concentration of vitamin C has a protective effect on neutrophils against ROS. It also affects neutrophil leukocyte chemokinesis and chemotaxis
[28][63]. In IBD, up to one fifth of patients with active inflammation may be vitamin C deficient, which may also be associated with feelings of increased fatigue and impaired wound healing
[29][64]. The cause of vitamin C deficiency in patients may be due not only to the active form of the disease, but also to the avoidance of fruit and vegetable consumption
[30][65]. A study by Miyake et al. showed that a higher intake of vitamin C and vegetables may be associated with a lower risk of UC
[31][66]. Other researchers have reached similar conclusions
[32][67]. Patients with C
rohn’s disease (CD
) also show reduced vitamin C intake
[33][68]. Jo et al. studied the effect of vitamin C deficiency in induced inflammatory bowel disease by administering DSS to mice. They observed that deficiency of the compound caused a decrease in mucin, while it increased IL-6 production and oxidative stress
[34][69]. The
SLC23A1 polymorphism may result in a decreased activity of the ascorbate transporter and its reduced intracellular amount
[35][70]. Good dietary sources of vitamin C include berries, citrus fruits, parsley
[36][71].
2.1.23. Zinc
Zinc is a trace element that must be supplied to the body in order for it to function properly. Zinc deficiencies can lead to malfunctioning of T and B lymphocytes and to abnormal maturation and differentiation of them
[37][72]. In addition, they can cause decreased phagocytosis and PMN (polymorphonuclear cells) chemotaxis, and also affect monocyte adhesion to the endothelium
[38][73]. Zinc has also been shown to preserve redox metabolism. An example is the increase in intracellular zinc in granulocytes caused by H
2O
2. Zinc can also be released in increased amounts from metallothionein (MT) through ROS induction
[39][74]. Zinc can increase IFN-γ (interferon gamma) secretion from peripheral blood mononuclear cells (PBMCs)
[40][75]. Deficiency of the element can lead to increased production of TNFα and IL-6
[41][76]. The antioxidant activity of zinc occurs indirectly. Its antioxidant functions are multiple, including increasing glutathione (GSH) production or as a cofactor of antioxidant enzymes
[42][77]. The element is also essential for maintaining normal intestinal barrier function, as its deficiency can reduce the function of the tight junction resulting in increased permeability. Additionally, the repair of the intestinal barrier requires the presence of zinc
[43][44][78,79]. Zinc is also responsible for the proper functioning of intestinal alkaline phosphatase
[45][80]. Deficiencies are more common in patients with IBD than in the general population
[46][81]. In patients with IBD, microelement deficiencies can increase the risk of complications of the disease, as well as hospitalisation
[47][82]. Therefore, screening is recommended, especially during disease exacerbations, to identify possible deficiencies
[48][83].
24.1.34. Selenium
Selenium was discovered in 1817
[49][84]. Biologically, it is found in the form of 25 selenoproteins and occurs in humans as an element with immunomodulatory effects, among others. It mainly neutralises organic hydroperoxides and hydrogen oxides
[50][85]. It has been shown to act on immune cells, such as NK cells and T lymphocytes, by affecting selected cell signalling pathways or antioxidant functions
[51][52][86,87]. The element also modulates redox signalling and counteracts ROS
[53][88]. The main compound in the selenoprotein group is glutathione peroxidase (GSH-Px). It consists of 4 units containing selenocysteine, which are antioxidant
[54][89]. It can regulate free radical production when there is inflammation
[55][90]. In addition, it can support immunoglobulin production
[56][91]. Selenium is also essential for the metabolism of some intestinal microorganisms
[57][92]. Cytoplasmic ROS activate the NF-κB signalling pathway and are subsequently involved in the expression of IL-2 and IFN-γ. Therefore, it is important to monitor selenium levels in IBD
[58][59][60][93,94,95]. Yan et al. tested whether there was a correlation between serum selenium levels and disease activity in CD patients. After including 135 patients in the study, they observed that serum concentrations of the element were inversely correlated with the severity of the disease course, indicating that selenium could be a factor along with other factors for monitoring disease activity
[61][96]. Some researchers indicate that it is possible to enhance the effect of a probiotic by adding selenium to it, which may also mitigate the inflammation that occurs
[62][63][64][97,98,99]. This could be due, among other things, to an increase in
SIRT1 gene expression
[65][100]. Keshteli et al. in their study observed that a diet containing anti-inflammatory ingredients altered the composition of the intestinal microflora in patients with UC and led to metabolic changes, which consequently supported the maintenance of clinical remission
[66][101]. In addition, adequate selenium levels can reduce the risk of cardiovascular disease in patients with IBD
[67][102]. Short et al. in their study observed that selenoprotein P (SEPP1) has a significant role in the regulation of intestinal homeostasis and thus the occurrence of inflammation and indirectly colorectal cancer
[68][69][103,104].
2.1.45. Betacarotene
Β-carotene is a vitamin A provitamin and belongs to the carotenoid group. It has a C40 in its structure including two β-ion rings
[70][105]. By scavenging superoxide radicals and quenching singlet oxygen, it is considered a compound with antioxidant properties
[71][106]. The antioxidant properties of the compound depend on its conformation. Hydrogen abstraction reactions are more exothermic in water compared to gaseous media
[72][107]. Β-carotene shows positive effects in many diseases, such as diabetes and skin diseases
[73][74][108,109]. Carotenoids also show beneficial effects on the gastrointestinal tract
[75][110]. Honarbakhsh et al. investigated whether carotenoids can have a positive effect on improving intestinal dysfunction. They showed that in the presence of vitamin A deficiency, the administration of β-carotene can reduce intestinal ROS and levels of pro-inflammatory cytokines. In addition, the compound may also have the effect of reducing the permeability of the intestinal barrier
[76][111]. Cheng et al., using epithelial cells in vitro, also observed an improvement in intestinal barrier function by enhancing tight junction function. They also found that with LPS- (lipopolysaccharide) induced colitis, β-carotene can reduce inflammation by down-regulating the toll-like receptor 4 (TLR4) pathway
[77][112]. In addition, provitamin A can exhibit IL-6 and TNF-α lowering abilities
[78][113]. Inflammatory bowel disease can also be alleviated by decreasing PGE2, nitric oxide (NO) production, and modulation of certain signaling pathways
[79][80][114,115]. Other studies, in animal models, have shown that β-carotene administration can modulate the composition of the intestinal microbiota, which could significantly benefit patients with IBD
[81][82][116,117]. Good dietary sources of β-carotene include vegetables (carrots, kale, parsley, chard) and fruits (apricots, melon)
[36][71].
2.1.56. Flavonoids
Flavonoids are compounds made up of a benzopyrone ring that contains polyphenolic or phenolic groups. They have a variety of uses and actions
[83][118]. The main groups of substances belonging to the category of flavonoids are: anticyanins (examples of bioactive substances: cyanidins, pelargonidins), flavanols (e.g., catechin, epicatechin), flavonols (e.g., quercetin, kaempferol), flavones (e.g., luteolin, apigenin), flavanones (e.g., naringenis, naringin), and isoflavones (e.g., daidzein, genistein)
[84][85][119,120]. Due to the presence of a hydroxyl group in the β-ring and a double bond, flavonoids exhibit antioxidant abilities against peroxynitrite, superoxide, or hydroxyl radicals
[86][121]. The antioxidant role of flavonoids is exerted by chelating metal ions, trapping reactive oxygen species, detoxifying enzymes, and increasing the production of antioxidant enzymes
[87][122]. They also inhibit the expression of pro-inflammatory mediators such as the NF-κB cascade, and inhibit the release of pro-inflammatory cytokines
[88][123]. In addition to their pro-inflammatory properties, the compounds show the ability to regulate tumour-associated macrophages (TAMs)
[89][124]. The anti-inflammatory effects of flavonoids focus primarily on inhibiting the activation of intracellular protein complexes containing PRRs (pattern recognition receptors) and inflammatory molecules. This occurs by decreasing the expression of components of the inflammasome, resulting in inhibition of caspase-1 activation and the secretion of pro-inflammatory cytokines
[90][125]. Flavonoids also show non-direct effects on the gut. In their work, Wang et al. show that citrus flavonoids can exert positive effects on maintaining normal intestinal barrier functions by regulating the expression of TJ (tight junction) expression. They mainly point to nobiletin as the bioactive component of flavonoids, which shows effects similar to those of an anti-inflammatory drug. In addition, citrus flavonoids show regulatory effects on mucin expression and secretion and on shaping the composition of intestinal microflora
[91][92][126,127]. Due to their properties, flavonoids may exert beneficial effects on the course of IBD by, among other things, protecting against functional and morphological changes in the vascular endothelium
[93][128]. Furthermore, they may counteract colonic inflammation by activating the AhR/Nrf2/NQO1 pathway as well as limiting the action of the NLRP3 (NLR family pyrin domain-containing-3) inflammasome
[94][129]. Due to all these factors, antioxidants can reduce the disease activity index
[95][96][130,131]. The main sources of flavonoids in food are herbs, vegetables, fruits, nuts, cereals, coffee, and tea
[97][132].
2.2. Endogenous Antioxidant Substances
Despite the fact that excessive and uncontrolled oxidative stress has destructive properties for the digestive system, antioxidant defence systems can counteract the undesirable effects of ROS
[98][99][133,134]. The main defence mechanism of the body involves the production of endogenous antioxidants, including superoxide dismutase (SOD), glutathione peroxidase (GPX), and catalase (CAT)
[100][135].
2.2.1. Superoxide Dismutase
Superoxide dismutase (SOD) is responsible for transforming superoxide radicals into hydrogen peroxide (H
2O
2) and molecular oxygen (O2)
[101][136]. Hydrogen peroxide is subsequently converted by catalase and glutathione peroxidases
[102][137]. The excessive and uncontrolled production of H
2O
2 can be potentially harmful to cells. In contrast, an optimal concentration of hydrogen peroxide may have a signalling effect
[103][138]. Superoxide dismutase exists in three isoforms: SOD1, SOD2 and SOD3. SOD1 is present mainly in the cytosol of liver and kidney cells, as well as in the central nervous system and erythrocytes. SOD2 is predominantly found in mitochondria. SOD3 is found in blood serum, tissues, and body fluids (including synovial fluid and cerebrospinal fluid)
[104][139].
2.2.2. Glutathione Peroxidase (GPX)
Glutathione peroxidase is a broad family of compounds with peroxidase activity
[105][148]. GPX has the ability to catalyse the conversion of glutathione to oxidised glutathione (GSH) and can also reduce H
2O
2 to water molecules and lipid hydroperoxides to stable alcohols. Humans have eight GPX isoforms, many of which contain selenocysteine residues
[106][149]. GSH, as a soluble antioxidant, has been shown to be less active in experimental mouse models of inflammatory bowel disease
[107][150].
2.2.3. Catalase
Catalase is located mainly in peroxisomes
[108][155]. CAT is responsible for breaking down H
2O
2 into water and molecular oxygen, thus preventing cell damage resulting from the Fenton reaction. In the Fenton reaction, which requires the presence of transition metal ions such as iron or copper, a highly reactive hydroxyl radical (HO) may be formed. In some cases, where catalase is absent, its functions can be performed by glutathione peroxidase
[109][156]. Catalase can also act in a so-called peroxidative mode, in which its functions involve the breakdown of small substrates such as methanol or formate
[110][157]. Another important function of catalase is apoptosis
[111][158]. A study showed that CAT activity in erythrocytes increases in patients with UC
[112][153]. In contrast, another analysis found persistent inhibition of CAT activity in mononuclear cells in patients with CD
[113][159]. On the basis of this, Iborra et al. showed that the constant decrease in CAT observed in CD patients may be due to genetic changes. Various genetic mechanisms that inhibit this antioxidant may contribute to the pathophysiology of CD
[114][160].