There are significant gender differences in the relationship between cortisol and depression. While the results may vary based on the age group and source of the samples, several mixed-gender studies show that there appears to be heightened serum cortisol levels in depressed males compared to depressed females. There are also differences noticed in salivary cortisol reactivity, with male children having increased reactivity, though these differences seem to diminish with age. Significant gender differences can also be seen in glucocorticoid and mineralocorticoid receptor expression. These differences are found both in expression levels as well as epigenetic regulation depending on the disorder and on the brain region.
- :stress
- gender
- depression
- cortisol
- glucocorticoid receptors
- mineralocorticoid receptors
1. Introduction
2. Structure and Function of Glucocorticoid and Mineralocorticoid Receptors in the HPA Axis
The human glucocorticoid receptor (GR) is coded by the NR3C1 gene, which is located on chromosome 5q31.3, and consists of three main structural and functional domains [11,21][6][10]. The human NR3C1 gene consists of 10 exons. Of these exons, the first, exon 1, is an untranslated region (UTR). Meanwhile, the N-terminal modulatory domain (NTD) is encoded by exon 2, while exons 3 and 4 encode the DNA binding domain (DBD). Finally, the hinge region (HR) and ligand-binding domain (LBD) are encoded by exons 5 to 9 [11][6]. In contrast to other steroid hormone receptors such as progesterone and estrogen, there is no F region to be found in the GR. From the NR3C1 gene, the classic GR isoform as well as the non-ligand-binding GR isoform are produced from the alternative splicing of two terminal exon 9s [22][11]. The NTD is where transcriptional activation function 1 (AF1) is located and serves as the site for most post-translational modifications [23][12]. The DBD contains two zinc finger motifs that bind to their target DNA sequences, glucocorticoid responsive elements (GREs) [23][12]. The LBD is where glucocorticoids bind and contains the transcriptional activation function 2 (AF2) that engages in ligand-dependent interactions with co-regulators [23][12]. GRs can be found in relatively high quantities throughout the human brain [24][13], with higher concentrations found in the frontal area, hypothalamus, hippocampus [25][14], and amygdala [26][15]. The mineralocorticoid receptor (MR) is coded for by the NR3C2 gene, which is located on chromosome 4q31. While the MR is structurally and functionally similar to the GR, differences in the LBD lead to the MR having a higher affinity for ligands such as aldosterone [27,28][16][17]. MRs are found throughout the human brain, though they are mainly localized in the limbic region, such as the hippocampus and the dorsolateral septum [29][18]. There have been more discoveries in recent years about the mechanisms of GRs and MRs in relation to HPA activity. Increased microRNA-124 (miR-124) levels have been associated with major depressive disorder [34][19]. MiR-124 directly targets GRs and when inhibited alleviates depressive-like symptoms in mice [35][20]. Furthermore, hypermethylation of NR3C1 exon 1F, which is related to higher basal HPA activity, has been observed in depressed patients who had experienced early life stress [36][21]. Genomic analyses reveal that differences in haplotypes for N3C1 and N3C2 affects stress-induced reactivity to cortisol, which subsequently impacts cognitive behavior [37][22]. Chaperone proteins such as Hsps and FKBPs have also been implicated in major depressive disorders, as certain SNPs for Hsps and FKBPs have been linked to a higher incidence of the disease [38[23][24],39], while increased FKBP51 expression in particular has been observed in depressed patients [40][25]. The role of the GR/MR in the HPA axis under depression is summarized in Figure 1.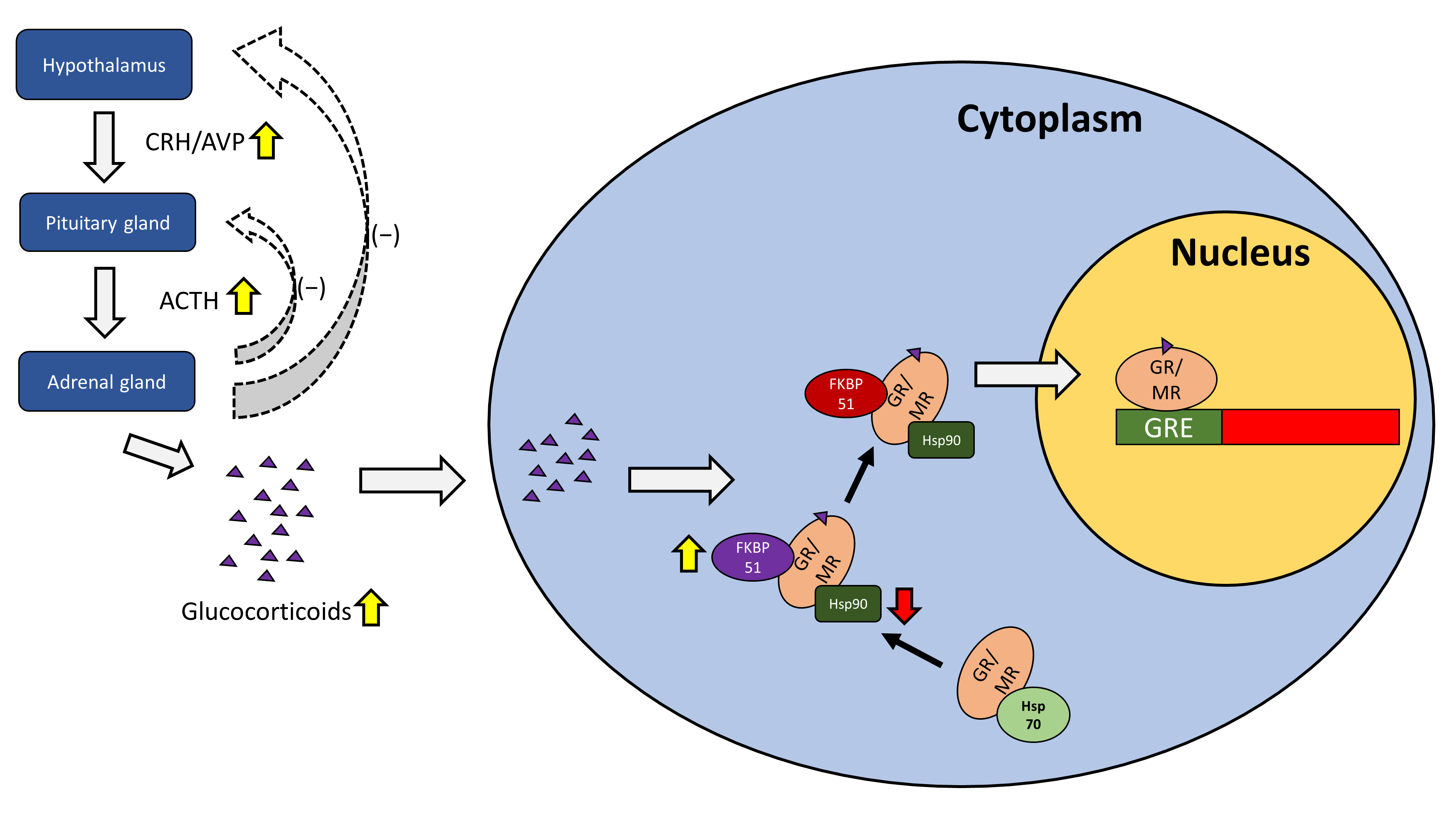
3. Gender Differences in Glucocorticoid and Mineralocorticoid Receptors in Mental Health
3.1. Gene Expression of Glucocorticoid Receptor- and Mineralocorticoid Receptor-Related Genes
3.2. Gender Differences in Animal Studies of Glucocorticoid and Mineralocorticoid Receptor Expression
The presence of gender differences in GR/MR expression in early-life-stress-induced depression appears to be supported by an early life stress animal model. Reactivity of the HPA axis was reduced in female mice exposed to early life stress and further exacerbated by decreased MR expression [73][30]. Male mice showed an increase in HPA reactivity as well as elevated upregulation of MR [73][30]. Gender differences in GR and MR expression are also seen in avian species. Social stress via mate pair separation of zebra finches revealed that female finches displayed an increase in hippocampal MR but not GR, while males showed a decrease in both hippocampal MR and GR [74][31]. A study performed on socially isolated female rats observed an increase in depressive-like behavior that subsides during estrus along with a reduction in GR expression in the hippocampus [75][32]. Another experiment performed on juvenile male rats showed GR expression increased and MR expression decreased during social isolation [76][33]. Furthermore, stress increased GR expression in group-housed rats with time, while it did not affect GR expression in isolated rats [76][33]. These studies indicate the influence of social isolation on altering GR expression. Furthermore, the finding that ovarian hormones may reduce GR expression [75][32] suggests a gender difference present in how GR activity is affected by social isolation.References
- Adam, E.K.; Quinn, M.E.; Tavernier, R.; McQuillan, M.T.; Dahlke, K.A.; Gilbert, K.E. Diurnal cortisol slopes and mental and physical health outcomes: A systematic review and meta-analysis. Psychoneuroendocrinology 2017, 83, 25–41.
- Hidalgo, V.; Pulopulos, M.M.; Puig-Perez, S.; Montoliu, T.; Salvador, A. Diurnal cortisol secretion and health-related quality of life in healthy older people. Int. J. Psychophysiol. 2021, 166, 127–133.
- Biliaminu, S.A.; Saka, M.J.; Sanni, E.O.; Imran, J.; Oluwatosin, I.O.; Dane, S. Gender-related Differences in Correlations among BMI, Salivary Testosterone and Cortisol and Depression and Alexithymia Scores in University Students. J. Res. Med. Dent. Sci. 2020, 8, 152–157.
- Altemus, M. Sex differences in depression and anxiety disorders: Potential biological determinants. Horm. Behav. 2006, 50, 534–538.
- McEwen, B.S. Glucocorticoids, depression, and mood disorders: Structural remodeling in the brain. Metabolism 2005, 54, 20–23.
- Kumar, R.; Thompson, E.B. Gene regulation by the glucocorticoid receptor: Structure:function relationship. J. Steroid Biochem. Mol. Biol. 2005, 94, 383–394.
- Trapp, T.; Holsboer, F. Heterodimerization between mineralocorticoid and glucocorticoid receptors increases the functional diversity of corticosteroid action. Trends Pharmacol. Sci. 1996, 17, 145–149.
- Oldehinkel, A.J.; Bouma, E.M.C. Sensitivity to the depressogenic effect of stress and HPA-axis reactivity in adolescence: A review of gender differences. Neurosci. Biobehav. Rev. 2011, 35, 1757–1770.
- Medina, A.; Seasholtz, A.F.; Sharma, V.; Burke, S.; Bunney, W., Jr.; Myers, R.M.; Schatzberg, A.; Akil, H.; Watson, S.J. Glucocorticoid and mineralocorticoid receptor expression in the human hippocampus in major depressive disorder. J. Psychiatr. Res. 2013, 47, 307–314.
- Gehring, U. The structure of glucocorticoid receptors. J. Steroid Biochem. Mol. Biol. 1993, 45, 183–190.
- Duma, D.; Jewell, C.M.; Cidlowski, J.A. Multiple glucocorticoid receptor isoforms and mechanisms of post-translational modification. J. Steroid Biochem. Mol. Biol. 2006, 102, 11–21.
- Oakley, R.H.; Cidlowski, J.A. The biology of the glucocorticoid receptor: New signaling mechanisms in health and disease. J. Allergy Clin. Immunol. 2013, 132, 1033–1044.
- Cao-Lei, L.; Suwansirikul, S.; Jutavijittum, P.; Mériaux, S.B.; Turner, J.D.; Muller, C.P. Glucocorticoid receptor gene expression and promoter CpG modifications throughout the human brain. J. Psychiatr. Res. 2013, 47, 1597–1607.
- Wang, Q.; Van Heerikhuize, J.; Aronica, E.; Kawata, M.; Seress, L.; Joels, M.; Swaab, D.F.; Lucassen, P.J. Glucocorticoid receptor protein expression in human hippocampus; stability with age. Neurobiol. Aging 2013, 34, 1662–1673.
- Wang, Q.; Verweij, E.; Krugers, H.; Joels, M.; Swaab, D.F.; Lucassen, P. Distribution of the glucocorticoid receptor in the human amygdala; changes in mood disorder patients. Brain Struct. Funct. 2014, 219, 1615–1626.
- Koning, A.-S.C.A.M.; Buurstede, J.C.; van Weert, L.T.C.M.; Meijer, O.C. Glucocorticoid and Mineralocorticoid Receptors in the Brain: A Transcriptional Perspective. J. Endocr. Soc. 2019, 3, 1917–1930.
- Rogerson, F.M.; Brennan, F.E.; Fuller, P.J. Mineralocorticoid receptor binding, structure and function. Mol. Cell. Endocrinol. 2004, 217, 203–212.
- Reul, J.M.H.M.; Gesing, A.; Droste, S.; Stec, I.S.M.; Weber, A.; Bachmann, C.; Bilang-Bleuel, A.; Holsboer, F.; Linthorst, A.C.E. The brain mineralocorticoid receptor: Greedy for ligand, mysterious in function. Eur. J. Pharmacol. 2000, 405, 235–249.
- Roy, B.; Dunbar, M.; Shelton, R.C.; Dwivedi, Y. Identification of microRNA-124-3p as a putative epigenetic signature of major depressive disorder. Neuropsychopharmacology 2017, 42, 864–875.
- Wang, S.-S.; Mu, R.-H.; Li, C.-F.; Dong, S.-Q.; Geng, D.; Liu, Q.; Yi, L.-T. microRNA-124 targets glucocorticoid receptor and is involved in depression-like behaviors. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2017, 79, 417–425.
- Farrell, C.; Doolin, K.; O’Leary, N.; Jairaj, C.; Roddy, D.; Tozzi, L.; Morris, D.; Harkin, A.; Frodl, T.; Nemoda, Z. DNA methylation differences at the glucocorticoid receptor gene in depression are related to functional alterations in hypothalamic–pituitary–adrenal axis activity and to early life emotional abuse. Psychiatry Res. 2018, 265, 341–348.
- Plieger, T.; Felten, A.; Splittgerber, H.; Duke, É.; Reuter, M. The role of genetic variation in the glucocorticoid receptor (NR3C1) and mineralocorticoid receptor (NR3C2) in the association between cortisol response and cognition under acute stress. Psychoneuroendocrinology 2018, 87, 173–180.
- Rao, S.; Yao, Y.; Ryan, J.; Li, T.; Wang, D.; Zheng, C.; Xu, Y.; Xu, Q. Common variants in FKBP5 gene and major depressive disorder (MDD) susceptibility: A comprehensive meta-analysis. Sci. Rep. 2016, 6, 32687.
- Wang, H.; Ba, Y.; Han, W.; Zhang, H.; Zhu, L.; Jiang, P. Association of heat shock protein polymorphisms with patient susceptibility to coronary artery disease comorbid depression and anxiety in a Chinese population. PeerJ 2021, 9, e11636.
- Tatro, E.T.; Everall, I.P.; Masliah, E.; Hult, B.J.; Lucero, G.; Chana, G.; Soontornniyomkij, V.; Achim, C.L. Differential expression of immunophilins FKBP51 and FKBP52 in the frontal cortex of HIV-infected patients with major depressive disorder. J. Neuroimmune Pharmacol. 2009, 4, 218–226.
- Sarubin, N.; Hilbert, S.; Naumann, F.; Zill, P.; Wimmer, A.-M.; Nothdurfter, C.; Rupprecht, R.; Baghai, T.C.; Bühner, M.; Schüle, C. The sex-dependent role of the glucocorticoid receptor in depression: Variations in the NR3C1 gene are associated with major depressive disorder in women but not in men. Eur. Arch. Psychiatry Clin. Neurosci. 2017, 267, 123–133.
- Klok, M.D.; Giltay, E.J.; Van der Does, A.J.W.; Geleijnse, J.M.; Antypa, N.; Penninx, B.W.J.H.; de Geus, E.J.C.; Willemsen, G.; Boomsma, D.I.; van Leeuwen, N.; et al. A common and functional mineralocorticoid receptor haplotype enhances optimism and protects against depression in females. Transl. Psychiatry 2011, 1, e62.
- Vinkers, C.H.; Joëls, M.; Milaneschi, Y.; Gerritsen, L.; Kahn, R.S.; Penninx, B.W.J.H.; Boks, M.P.M. Mineralocorticoid receptor haplotypes sex-dependently moderate depression susceptibility following childhood maltreatment. Psychoneuroendocrinology 2015, 54, 90–102.
- Webster, M.J.; Knable, M.B.; O’Grady, J.; Orthmann, J.; Weickert, C.S. Regional specificity of brain glucocorticoid receptor mRNA alterations in subjects with schizophrenia and mood disorders. Mol. Psychiatry 2002, 7, 985–994.
- Bonapersona, V.; Damsteegt, R.; Adams, M.L.; van Weert, L.T.; Meijer, O.C.; Joëls, M.; Sarabdjitsingh, R.A. Sex-Dependent modulation of acute stress reactivity after early life stress in mice: Relevance of mineralocorticoid receptor expression. Front. Behav. Neurosci. 2019, 13, 181.
- Madison, F.N.; Kesner, A.J.; Alward, B.A.; Ball, G.F. Sex differences in hippocampal mineralocorticoid and glucocorticoid receptor mRNA expression in response to acute mate pair separation in zebra finches (Taeniopygia guttata). Hippocampus 2018, 28, 698–706.
- Ramos-Ortolaza, D.L.; Doreste-Mendez, R.J.; Alvarado-Torres, J.K.; Torres-Reveron, A. Ovarian hormones modify anxiety behavior and glucocorticoid receptors after chronic social isolation stress. Behav. Brain Res. 2017, 328, 115–122.
- Boero, G.; Pisu, M.G.; Biggio, F.; Muredda, L.; Carta, G.; Banni, S.; Paci, E.; Follesa, P.; Concas, A.; Porcu, P. Impaired glucocorticoid-mediated HPA axis negative feedback induced by juvenile social isolation in male rats. Neuropharmacology 2018, 133, 242–253.
