1. Introduction
According to Food and Agriculture Organization (FAO) and World Health Organization (WHO), probiotics are live microorganisms that provide health benefits to the host when ingested in adequate amounts
[1][2][3][1,2,3].
Lactobacillus and
Bifidobacterium are the most commonly used probiotic genera and are widely incorporated into functional foods (e.g., fermented dairy products) and dietary supplements
[4]. Some health benefits associated with the consumption of probiotics include stimulation of the immune system, antagonism against gastrointestinal pathogens, cholesterol reduction, and anticancer effects
[5]. Due to the highly documented beneficial effects of probiotics on human health, the food industry has become increasingly interested in these microorganisms.
Regulatory approaches used to approve probiotics in food vary across regions. In Europe, the European Food Safety Authority (EFSA) has developed the Qualified Presumption of Safety (QPS) approach, a safety assessment procedure for microbes found in food and feed chains. QPS includes microorganisms such as probiotics which have been assessed by the EFSA as not raising any safety concerns
[6]. Moreover, Regulation (EC) No. 1924/2006 establishes directives on nutrition and health claims made on foods, covering the communication on the nutritional and health effects of probiotics
[7]. In the US, the use of probiotics is regulated by the Generally Recognized as Safe (GRAS) guidelines developed by the Food and Drug Administration (FDA)
[8].
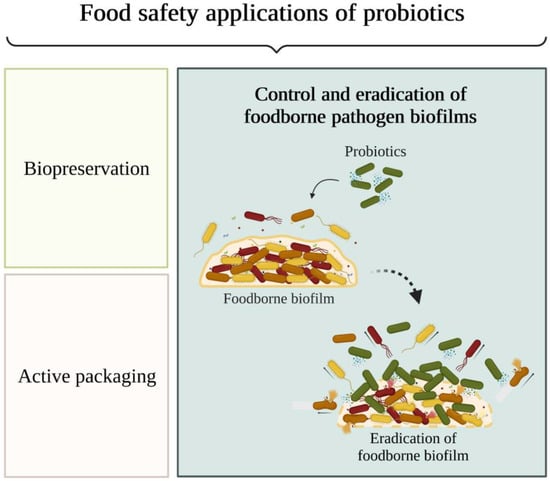
In addition to their use in functional foods and dietary supplements, probiotics have been studied for applications in food safety assurance (
Figure 1) as a promising strategy for food biopreservation, active food packaging, and prevention and control of biofilm formation in the food industry
[5][9][5,9]. Biopreservation is a hurdle approach that is applied to extend the shelf life and prevent food spoilage using specific microorganisms and their antimicrobial products (e.g., organic acids, hydrogen peroxide, and bacteriocins)
[9]. The combination of hurdles, such as probiotics and non-thermal technologies, can ensure that all pathogens are eliminated or rendered harmless in the final food product. Indeed, it has been reported that non-thermal techniques induce the formation of compounds that promote the growth and survival rates of beneficial microbes in food, making food products safer for consumption
[10].
Figure 1.
Food safety applications of probiotics: preservation, packaging, and control and eradication of foodborne pathogen biofilms.
2. The Nature and Extent of Foodborne Diseases
When food safety is compromised, foodborne diseases can develop. They comprise a broad range of diseases caused by microorganisms, chemicals, toxins, radioactivity, or even physical agents present in ingested food or water. Foodborne illnesses constitute a public health problem since they boost morbidity and mortality, causing a significant number of hospitalisations and deaths
[5][11][12][5,12,13]. Worldwide, the consumption of contaminated food or water results in 600 million infections (7.7% of the world’s population) and 420,000 deaths every year. In Europe, an estimated 23 million people suffer from foodborne diseases annually, resulting in approximately 5000 deaths
[11][12]. The annual number of infections in the US is approximately 48 million, with more than 3000 deaths
[13][14]. Additionally, foodborne diseases pose a huge economic burden. The lost productivity and medical costs associated with this type of infection are more than US$ 110 billion per year in low- and middle-income countries
[14][15]. In the US, the total cost in 2018 was US$ 17.6 billion
[15][16].
Salmonella spp. was the pathogenic microorganism causing the highest number of reported foodborne infections in 2020, followed by norovirus and
Listeria monocytogenes [16][17]. Other important bacteria known to cause foodborne diseases include
Staphylococcus spp.,
Clostridium spp., and
Vibrio spp.
[5]. For example,
Salmonella can cause diarrhoea, fever, and abdominal pain;
L. monocytogenes can cause febrile gastroenteritis and other extreme health problems such as meningitis and abortion; and
S. aureus can cause acute gastroenteritis
[17][18]. In 2020, campylobacteriosis and salmonellosis caused the highest number of reported zoonoses, followed by yersiniosis and intoxication by Shiga, a toxin produced by some
Escherichia coli strains
[16][17].
3. The Role of Biofilms in Food Contamination
Food contamination can occur at any stage of the food chain, from production, processing, storage, distribution, or even the preparation and cooking of food by consumers
[18][19]. According to the European Council Regulation (EEC) No. 315/93, a contaminant is any substance not intentionally added to food which is present in such food as a result of the production, manufacture, processing, preparation, treatment, packing, packaging, transport or holding of such food, or as a result of environmental contamination
[19][20]. Food contamination may lead to changes in taste, smell, texture, or appearance, which are considered unacceptable or undesirable
[20][21]. Raw, uncooked, minimally processed food, mostly of animal origin, but also fruits and vegetables, are at high risk of bacterial contamination
[21][22].
Instead of being present in the planktonic state, bacteria tend to adhere to food contact surfaces and form biofilms
[22][23]. The risk of biofilm formation is particularly high in cutters, conveyor belts, drains, walls, and ceilings
[23][24]. Biofilms pose a noticeable hygiene risk by being reservoirs of food pathogens and spoilage microorganisms, which alter the organoleptic properties of food by secreting lipases and proteases
[22][24][23,25]. Additionally, biofilms have the ability to clog and corrode equipment, causing machinery technical failure and, consequently, huge economic losses
[17][25][18,26]. The availability of nutrients from food residues and moisture on these surfaces promotes the development of biofilms, which can form in all types of materials, for instance, stainless steel, plastic, polystyrene, and glass
[25][26]. The relevant biofilm-forming food-associated pathogens include
L. monocytogenes,
Campylobacter spp.,
Salmonella spp.,
Pseudomonas spp., and
E. coli [21][22][22,23].
A biofilm can be defined as a complex aggregate of bacteria established in a three-dimensional structure and embedded in a matrix synthesised by the microbial community
[23][26][24,27]. The generally accepted model of biofilm formation includes five stages: reversible attachment, irreversible attachment, maturation I, maturation II, and dispersion
[27][28]. Initially, planktonic cells adhere to the surface via a single pole through weak and reversible interactions and can readily detach and return to the planktonic phase. Surface conditioning, which consists of organic substances absorbed on the surface, serves as a nutritional cue, thus triggering biofilm formation
[25][26]. The transition from reversible to irreversible attachment occurs when bacterial appendages overcome physical repulsive forces, and consequently, cell surface proteins can permanently bind to the surface
[25][28][26,29]. Cell attachment depends on multiple factors, including environmental conditions, surface characteristics, and microbial cell properties
[22][29][30][23,30,31]. The maturation stage of biofilm formation encompasses the accumulation of cells, forming cell clusters that subsequently mature into microcolonies
[27][28]. At this stage, bacteria increase the production of extracellular polymeric substances
[25][26]. This extracellular matrix surrounds sessile microorganisms, protecting them from the stressful conditions found during food processing (e.g., low temperature, acidity, or oxidative and osmotic stresses) and limiting the effect of antimicrobials, which, in turn, allows biofilm growth and proliferation
[12][30][31][32][13,31,32,33]. In addition, high cellular density facilitates direct horizontal gene transfer between cells, which can confer antibiotic resistance to bacteria within biofilms
[23][33][24,34]. Cell dispersion can occur in mature biofilms; thus, bacteria can return to their planktonic form and colonise new surface locations
[25][32][26,33]. Biofilm dispersion enhances microorganism spread, resulting in food contamination and spoilage
[21][22]. The high cellular density and the concentration gradients of nutrients, oxygen, and waste cause biofilm cells to experience an ever-changing microenvironment. The original five-stage model of biofilm development presented before does not accurately represent these microenvironments or the complexity of biofilm structures and processes in real-world industrial systems. Thus, a recent publication proposed a more encompassing model for biofilm formation, which includes three steps: aggregation, growth, and disaggregation
[34][35]. The suggested model considers different habitats and microenvironments, the possible influx of new cells, and surface-attached and non-surface-attached biofilms.
4. Biofilm Prevention and Control Strategies in the Food Industry
The best approach to eradicate biofilms in the food industry is to prevent their formation and, more importantly, prevent microorganisms from entering food processing facilities. The establishment of an effective hygiene protocol and a correct plant and equipment design are crucial to limit the access of microorganisms to factories and further contact with food
[22][35][23,36]. For example, gaps, crevices, and dead areas should be avoided in order to minimise the locations where microorganisms can find shelter and grow
[22][23]. The choice of surface materials and coatings is also important for inhibiting biofilm formation
[35][36]. In addition, the adoption of a Hazard Analysis and Critical Control Point system (HACCP) is essential to preserve food safety and quality
[23][24]. Its application by companies in the food sector is recommended in EC Regulation No. 852/2004 (Hygiene of Foodstuffs) and EC Regulation No. 853/2004 (Specific Rules Food of Animal Origin) of the European Union.
Once biofilms are formed on food contact surfaces, mechanical and physical cleaning actions are the first approaches to be applied
[35][36], such as super-heated steam injection and high-pressure washing
[25][26]. These measures disrupt the extracellular matrix, destroying the biofilm and moving the sessile cells to the sensitive planktonic state, which is essential for the complete removal of biofilms
[32][35][33,36]. A combination of physical and chemical methods is commonly used in the food industry. For example, Cleaning-In-Place (CIP) combines mechanical actions with the use of chemical cleaning agents. Its efficacy depends on the properties of the surface being cleaned, the type of biofilm, the concentration of the cleaning agents, and CIP time and temperature
[36][37].
Chemical treatment with detergents, sanitisers, and disinfectants seems to be an effective biofilm control method
[22][30][37][23,31,38]. Sodium hypochlorite, hydrogen peroxide, peracetic acid, and sodium hydroxide are chemical agents that have demonstrated competence in reducing biofilms
[21][24][22,25]. However, the doses and application times of these chemical agents are usually adapted to kill planktonic microorganisms, thus they may be inefficient against biofilms
[23][24]. Additionally, biofilms are more tolerant to some biocides, including chlorine-based and quaternary ammonium sanitisers
[24][25]. Several reasons have been suggested to explain this biofilm tolerance: (1) the defective diffusion of antimicrobials within the biofilm due to the extracellular polymeric matrix, (2) biocide enzymatic degradation within the matrix, (3) the slow metabolism of bacteria inside the biofilm, which prevents the effect of many antibiotics/biocides, and (4) the formation of spores, which have a high intrinsic resistance to environmental stresses. Additionally, the resistance of biofilms is enhanced because of acquired or intrinsic genetic modifications, including overexpression of efflux pumps and modification of antimicrobial binding sites
[22][38][23,39].
Biofilm tolerance against synthetic antimicrobials and the negative consumer perception towards these chemicals, in addition to their release into the environment and the high amount of water spent in cleaning, have strengthened the search for different alternatives, namely for environmentally friendly disinfection
[24][31][25,32]. Environment-friendly biofilm control strategies include the use of enzymes, bacteriophages, natural compounds such as essential oils, and bacterial products such as bacteriocins and biosurfactants
[30][37][31,38]. Enzymes (e.g., proteases, lipases, and polysaccharidases) are biodegradable and low-toxicity bioactive macromolecules that have shown the ability to inhibit biofilm formation. Currently, they are widely used in detergents for application in the food industry, despite their production costs and strict time and temperature requirements
[22][24][32][23,25,33]. Bacteriophages are viruses targeting prokaryotic cells and are, therefore, innocuous to humans. Some commercial solutions have bacteriophages in their composition due to their anti-biofilm ability, although they have some limitations in targeting microorganisms inside biofilms due to the extracellular matrix
[24][25]. In turn, essential oils consist of a plant-derived mixture of secondary metabolites (e.g., phenol, thymol, and carvacrol)
[32][33]. Some of their components exhibit important anti-biofilm properties, even though some essential oils may irritate the skin and other human organs
[24][25]. Biosurfactants are amphipathic molecules secreted by microorganisms capable of disrupting the hydrophobic interactions involved in biofilm matrix cross-linking
[32][33]. These metabolic products can also prevent biofilm formation by altering the hydrophobic characteristics of the bacterial surface and decreasing surface tension and, consequently, its adhesion ability
[24][25]. Bacteriocins are ribosomally synthesised proteins or peptides with antibacterial activity
[39][40][40,41]. For example, nisin, derived from
Lactococcus lactis, has been approved for its antimicrobial activity against several foodborne microorganisms by the WHO and the FDA and is widely used as a food preservative
[24][30][25,31]. The main disadvantages of these molecules are their high production cost and narrow-spectrum antibacterial activity
[13][14].
Quorum sensing (QS) inhibition is believed to be another approach to control biofilm formation, although their relationship is not yet fully understood. Contrary to bactericidal strategies, molecules targeting QS cause less selection pressure to develop resistance to antimicrobial agents
[21][24][22,25]. QS inhibition may occur through the following mechanisms: (1) competitive binding of inhibitors to QS signalling molecules (called autoinducers (AI)), (2) degradation of AI signals through quorum-quenching enzymes, (3) post-transcriptional control of QS genes via sRNAs, and (4) inhibition of AI. The disturbance of only one component of the QS pathway often leads to the downregulation of QS genes and the inactivation of the QS mechanism
[24][41][25,42]. Quorum-quenching molecules are produced by microorganisms when they compete with neighbouring cells. However, bacteria can also degrade their own QS molecules to maintain an appropriate signal concentration
[21][22].
Probiotics have arisen as a promising alternative strategy for controlling biofilm formation in the food industry, thereby preventing antimicrobial resistance associated with foodborne microorganisms
[5]. Their antagonistic activity may be due to competition for nutrients and adhesion sites or the release of antimicrobial metabolites, such as bacteriocins, biosurfactants, organic acids, hydrogen peroxide, and inhibitory exopolysaccharides [18][24][30][32]. Bacteriocins can compromise cell integrity by dissipating the proton motive force and disrupting bacterial membranes through pore formation or inhibition of peptidoglycan synthesis. Organic acids, such as lactic acid, lead to a lowering of pH, which can inhibit the growth of microorganisms without affecting probiotics due to their tolerance to low pH. Biosurfactants can affect cell surface compounds (e.g., surface proteins) and remove lipopolysaccharides from Gram-negative bacteria, decreasing the cell surface hydrophobicity and preventing further bacterial adhesion to food contact surfaces. Hydrogen peroxide is an oxygen-containing compound with reactive properties that can damage biomolecules such as DNA. Enzymes can target microorganisms for hydrolysis of extracellular proteins, degradation of exopolysaccharides, eDNA damage by endonucleases, and degradation of QS molecules by quorum-quenching enzymes. In addition to quorum-quenching enzymes, QS inhibition may occur by the repression of genes encoding QS signals or by interference with their receptors.
Probiotics can inhibit the growth of microorganisms and biofilm formation through displacement, exclusion, or competition [42]. Displacement consists of adding probiotics and/or their metabolites to disrupt already formed biofilms; exclusion consists of coating food contact surfaces with probiotic biofilms and/or their metabolites to prevent the adhesion of pathogenic microorganisms; competition involves the direct interaction of probiotics and/or their metabolites with foodborne microorganisms [43].
Regarding the displacement strategy, L. monocytogenes and S. aureus are the most studied biofilm-forming pathogens, while Lactiplantibacillus and Lacticaseibacillus are the most tested probiotic genera. Probiotic cells and cell-free supernatants are the most used agents to displace biofilms from abiotic surfaces. Among the antimicrobial substances tested, whole cells showed the most promising results in biofilm displacement, followed by bacteriocins[5].