Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Gyun-Ho Jeon | -- | 2417 | 2024-03-18 08:02:55 | | | |
| 2 | Lindsay Dong | Meta information modification | 2417 | 2024-03-19 02:38:58 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Jeon, G. Management of Insomnia in Menopausal Women. Encyclopedia. Available online: https://encyclopedia.pub/entry/56368 (accessed on 08 February 2026).
Jeon G. Management of Insomnia in Menopausal Women. Encyclopedia. Available at: https://encyclopedia.pub/entry/56368. Accessed February 08, 2026.
Jeon, Gyun-Ho. "Management of Insomnia in Menopausal Women" Encyclopedia, https://encyclopedia.pub/entry/56368 (accessed February 08, 2026).
Jeon, G. (2024, March 18). Management of Insomnia in Menopausal Women. In Encyclopedia. https://encyclopedia.pub/entry/56368
Jeon, Gyun-Ho. "Management of Insomnia in Menopausal Women." Encyclopedia. Web. 18 March, 2024.
Copy Citation
Insomnia is one of the major complaints of menopausal women with advancing age and may be complexly related to a variety of causes.
hot flushes
insomnia
menopause
sleep disorder
menopausal hormonal therapy
1. Introduction
With the decline of reproductive hormones in the menopausal transition period, a substantial number of women experience physiological and psychological changes. Sleep disturbance is one of the major complaints of menopausal women with advancing age. Menopausal women also frequently experience other typical menopausal symptoms, including hot flashes (HFs), night sweats, palpitations, mood changes, anxiety, and depression, which also increase the risk of developing sleep problems [1]. Indeed, various sleep problems, such as decreased sleep duration, poor sleep quality, and early morning awakenings, commonly begin in the menopausal period [2]. It is reported that women in menopausal transition or menopause suffer from sleep disturbance or insomnia, ranging from 35% to 60%, and a significant number of women experience severe symptoms that impair daytime functioning [3]. Sleep disturbance can cause fatigue, somnolence, mood disorders, memory impairment, lack of attention, and even accidents, which can lead to behavioral, occupational, and social problems [4]. Recent studies revealed that insomnia is also associated with significant medical problems, such as cardiovascular disease, diabetes, and an increased risk of mortality [5]. In addition to menopause, it has been reported that women have specific periods related to vulnerability to sleep disorders, such as the menstrual cycle and pregnancy, suggesting a link between sleep disorders and female hormones [6][7]. As such, insomnia is closely related to hormonal changes and, although it is a major menopausal symptom, there are currently no universal guidelines for treating insomnia in menopausal women.
2.Definition of Insomnia and Sleep Disorders
Insomnia is defined as difficulties falling asleep or maintaining sleep, which result in daytime impairment, despite adequate opportunity and circumstances to sleep. Chronic insomnia disorder is defined when it occurs at least three times per week for three months, according to the International Classification of Sleep Disorders, Third Edition (ICSD-3). Insomnia was traditionally approached as a primary or secondary (comorbid) disorder, provoked by physical problems or psychosocial factors, etc. (as will be discussed later in the Insomnia Etiology Section), but there were issues of uncertainty with the nature of the associations and the direction of causality in comorbid insomnia cases; thus, all insomnia diagnoses were consolidated under chronic insomnia disorder [8].
3. Sleep Disturbance across Menopause: Epidemiology
Middle-aged women have increasing complaints of sleep disorders as they enter menopausal transition and the menopausal period. The incidence rates of sleep problems show 39–47% in peri-menopausal and 35–60% in postmenopausal women, compared to 16–42% in premenopausal women [3]. Although sleep deteriorates with age and is affected by many physical problems (lower back pain, musculoskeletal disorders, urinary symptoms, hot flushes (HFs), etc.), mood disorders and psychosocial factors, socioeconomic, and racial/ethnic factors [9][10], an independent relationship between menopausal stages and sleep disturbance, controlled for the effects of aging and other confounders, was shown in a meta-analysis of 24 cross-sectional studies [11].
Meanwhile, women who had undergone surgical menopause and were not taking hormone therapy had the highest prevalence of sleep disturbance compared with natural menopausal transitional women, independent of age or years since surgery. The most common sleep complaint in these women was reported as frequent awakenings during sleep in the longitudinal analysis of the Study of Women’s Health Across the Nation (SWAN) [3].
4. Pathogenesis and Etiology of Insomnia and Menopause
Sleep disturbance in postmenopausal women is pathophysiologically multifactorial (Table 1). Physiologically, it may be strongly associated with menopause symptoms, such as HFs and night sweats that can be experienced along with female hormonal changes [12], and psychiatrically, with mood disorders, anxiety, and depression [9]. In addition, family/economic/social stress, obesity, ill health, and drug and alcohol intake are common causes of sleep problems in middle-aged women, and commonly encountered comorbid diseases with sleep disorders include OSA, RLS, and periodic leg movement syndrome. After menopause, the prevalence of OSA increases due to weight gain and changes in fat distribution from increased testosterone production and decreased female hormones, and the incidence of RLS increases [13][14].
Table 1. Etiology of sleep disorders in menopause.
| Physiologic/Physical |
|---|
| Age Circadian rhythm modifications Decreased melatonin secretion Female sexual hormone changes Decreased estrogen and progesterone, increased FSH Menopausal symptoms Hot flushes, night sweats Others Bladder problems, Ill health, chronic pain—musculoskeletal disorders, osteoarthritis, fibromyalgia, cancer, etc. Poor sleep hygiene/circumstances Medication, coffee, smoking |
| Psychiatric/Psycho-social |
| Mood disorder—depression Anxiety Illegal drugs, alcohol intake Others—familial/economic/social problem: stress, bereavement, divorce, unemployment, finances, etc. |
| Comorbid diseases with sleep disorders |
| Obstructive sleep apnea Restless legs syndrome Periodic limb movement syndrome |
| Others |
| Circadian rhythm sleep–wake disorder Narcolepsy, idiopathic hypersomnia Parasomnias |
FSH: follicle-stimulating hormone.
5. Assessment of Insomnia in Menopausal Women
The diagnosis of insomnia is mainly performed clinically based on the subjective complaints of the patient, and in menopausal women, insomnia commonly occurs as a secondary disorder to physical and psychiatric problems, underlying other sleep disorders, such as OSA or RLS [9][15]. Therefore, careful assessment by proper history taking is important to exclude the comorbid factors. A detailed history from patients and family members using sleep questionnaires and diaries, including the onset of insomnia, pattern and frequency (number of nights/week) of insomnia symptoms, sleep/awake schedule, frequency and bother from menopausal symptoms (HFs and night sweats), and contributing factors or diseases, should be performed. The impact of the sleep complaint on the patient’s life, daytime sleepiness, sleep hygiene, and physical symptoms—snoring, any apneic episodes, dryness of mouth, sweating, restless legs sensation, and periodic limb movements—suggesting other sleep disorders, such as OSA, RLS, etc., should be assessed.
6. Management of Insomnia in Menopausal Women
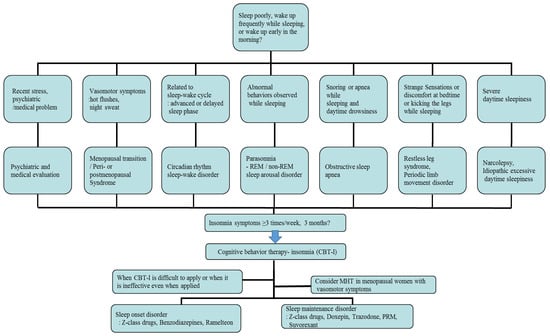
First of all, individual treatment for the identified underlying disease or condition of insomnia is generally necessary, but insomnia after the menopausal transition may be associated with multiple overlapping factors, so management can be complicated and requires individualized treatment. In cases related with multiple sleep disorder factors, such as moderate to severe HFs, depression, and OSA, combined treatments can be considered. The main treatment options for menopausal women with insomnia include non-pharmacological treatment and pharmacological treatment, which are represented by cognitive behavioral therapy for insomnia (CBT-I) and MHT/non-hormonal pharmacological treatment, respectively [16][17]. According to the clinical practice guidelines of the American Academy of Sleep Medicine (AASM) and the European Sleep Research Society (ESRS) for the treatment of insomnia, CBT-I is the first-line intervention for all patients with chronic insomnia, and similar considerations should be given to menopausal women with insomnia. A pharmacological treatment can be offered if CBT-I is not effective or unavailable [17][18]. In patients with OSA, non-pharmacological therapy—continuous positive airway pressure or an oral appliance—should be applied according to the severity of disorder. In addition, in the cases of RLS, triggering factors such as coffee, nicotine, alcohol, antidepressants, and antihypertensive drugs should firstly be avoided, and dopaminergic agonists are the first-line treatment for moderate to severe disease [9]. An example of a flowchart for diagnosing and treating insomnia in postmenopausal women, reflecting medical history and related symptoms, is provided in Figure 1.
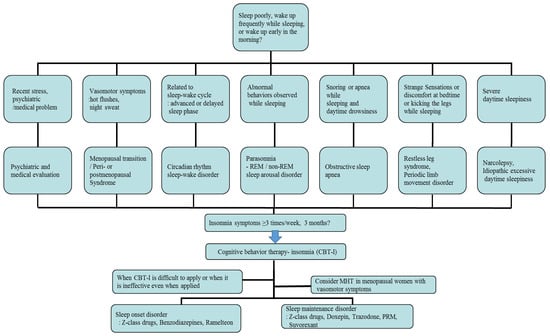
Figure 1. An example of a flowchart for diagnosing and treating insomnia, reflecting patient history and related symptoms, in postmenopausal women. REM: rapid eye movement; MHT: menopausal hormone therapy; PRM: prolonged-release melatonin.
6.1. Non-Pharmacological Treatment
CBT-I is a treatment that includes cognitive therapy to change patients’ beliefs and attitudes about sleep and behavioral techniques to improve their insomnia, which typically includes sleep hygiene education to provide better sleep conditions, sleep restriction therapy to increase sleep efficiency, stimulus control therapy to adjust the relationship between sleep and sleep stimulation conditions, relaxation training to promote a good sleep, and cognitive therapy to correct dysfunctional thinking about sleep [19][20].
6.1.1. Sleep Hygiene Education
Sleep hygiene education teaches patients about behavioral and environmental factors to improve sleep, as follows: ensuring the sleep environment is quiet and at a temperature suitable for sleeping, establishing a regular bedtime, adequate exercise and exposure to sunlight, avoiding caffeine in the afternoon and excessive fluids, alcohol, and nicotine at bedtime, limiting naps to 30 min, limiting bedtime screen use, etc.
6.1.2. Sleep Restriction Therapy and Stimulus Control Therapy
These behavioral treatments of insomnia are for breaking the maladaptive connection between going to sleep and the hyperarousal state. Sleep restriction therapy considers the patient’s actual sleep time and limits the time spent in bed to increase the sleep desire. Monitoring the sleep and wake times every day and trying to stay in bed only during sleep can improve sleep efficiency. Stimulus control therapy involves breaking the relationship between being in the bedroom and negative aspects of sleep, such as lying in bed only when tired and using the bed only for sleeping.
6.1.3. Relaxation Training
Relaxation training is used to control thought patterns and somatic tension that interferes with sleep. This relaxation-based intervention, alternating contraction of muscles with relaxation, is achieved through progressive muscle relaxation, abdominal breathing, etc.
6.1.4. Cognitive Therapy
Cognitive therapy examines negative beliefs or dysfunctional thoughts about sleep, such as the belief that insomnia will persist, excessive worry or obsession with sleep, trying to lie down and sleep beforehand, etc., and replaces them with rational thoughts or facts by setting a realistic amount or quality of sleep.
6.2. Menopausal Hormone Therapy
Based on the identified roles of reproductive hormones in sleep and the theory that vasomotor symptoms (VMS), such as HFs, in menopause cause insomnia, as discussed above, MHT can be an important treatment for insomnia in menopausal women with hot flashes. Indeed, a meta-analysis including 15,468 women from 42 trials published in 2017 showed that MHT improved sleep quality in menopausal women with VMS, along with improvement in concomitant VMS. There was no significant difference when women without VMS were analyzed separately or combined in the study [21]. However, several previous studies exploring the effects of estrogen and progesterone on sleep efficiency have shown mixed results. While some studies suggested that hormone therapy, such as low-dose estrogen with micronized progesterone or drospirenone, 17β-estradiol-progesterone, and low-dose oral estradiol and venlafaxine, reduced insomnia symptoms compared with a placebo [22][23][24][25][26], some contrary results were also reported, which failed to identify any superiority of MHT over the placebo [27][28].
6.3. Non-Hormonal Pharmacological Treatment
6.3.1. Benzodiazepines and Z-Class Drugs
Benzodiazepines (triazolam, temazepam, and estazolam) and Z-class drugs (zolpidem, zopiclone, and zaleplon) act as agonists of the benzodiazepine receptor component of the GABAA receptor complex and are commonly used for treating insomnia. Z-class drugs are known to have relatively fewer side effects compared to benzodiazepines, as they are made to mainly bind selectively to type 1 GABA-A receptors and produce only a sleeping effect [29].
In menopausal women with insomnia, several RCTs for Z-class drugs have also reported that zolpidem increased the total sleep time and decreased the wake time after sleep onset and number of awakenings [30], and eszopiclone was effective in the treatment of insomnia, as well as VMS [31]. However, these agents are suggested for short-term use for ≤4 weeks at the lowest dose in adults with insomnia due to their unproven long-term efficacy, the risk of tolerance, and the potential for dependence and abuse, according to the AASM and ESRS practice guidelines [17][18]. Common side effects of benzodiazepines and Z-class drugs include headache, dizziness, and daytime sleepiness and drowsiness, and in particular, the elderly are at increased risk of side effects such as cognitive function impairment, delirium, and falls and fractures due to the muscle relaxation effect, although Z-class drugs have relatively fewer side effects compared to benzodiazepines [32].
6.3.2. Antidepressants
Given that insomnia is highly implicated in depression, antidepressants can be considered for treating insomnia in menopausal women with comorbid depression. Moreover, antidepressants, such as serotonin and norepinephrine reuptake inhibitors (SSRIs and SNRIs), are valid treatments for VMS in menopausal women with contraindication to MHT [33][34]. Ensrud et al. reported that escitalopram was effective for insomnia in a RCT of 205 peri- and post-menopausal women with HFs [35]. Mirtazapine is also known to be useful in cases of not only insomnia but also depression, which has a sleep-inducing effect and increased slow-wave sleep effect, along with side effects such as appetite, weight gain, and dry mouth [36]. However, there are limited studies on the direct effects of these antidepressants on insomnia; therefore, using antidepressants to treat sleep disruption for women without depression should not be recommended [37].
6.3.3. Melatonin
Melatonin basically advances the sleep cycle and has a sleep-favoring effect. Supplementation with melatonin has been reported to improve insomnia symptoms and mood disorders in postmenopausal women without serious side effects [38][39]. A prolonged-release melatonin (PRM) agent (2 mg) was approved for patients with primary insomnia over 55 years old for short-term use in some European countries [40]. Unlike existing melatonin preparations, which did not have sufficient effects due to their short half-life of 35 to 50 min, the prolonged-release formulation can improve the sleep structure by maintaining the concentration over 8 to 10 h, similar to the pattern of melatonin secretion in the body [41]. However, clinical trials among the elderly, including menopausal women, had inconsistent results, not only in the quality of sleep, but also in menopausal symptoms [39][41][42][43].
6.3.4. Orexin Antagonist and Gabapentin
Orexin is a neuropeptide that plays an important role in promoting wakefulness and impairing thermoregulation and plasma level of orexin increases after menopause. Suvorexant, an orexin OX1 and OX2 receptor antagonist, was approved by the U.S. FDA as a treatment for insomnia in 2014, and the AASM suggested that suvorexant could be used for sleep maintenance disorder.
7. Conclusions
Diagnosis of insomnia in menopausal women is largely performed based on the subjective complaints of patients and may be complexly related to a variety of causes, including changes in female hormones, aging, weight gain, psychosocial problems, and alcohol and drug use. Careful history taking and multidisciplinary physical and psychosocial evaluation are necessary and, in particular, comorbidities related to sleep disorders, such as OSA, must be taken into consideration. Additionally, a unique aspect of insomnia in postmenopausal women is that menopausal symptoms (HFs, mood disorders, musculoskeletal symptoms, and pain) due to hormonal decline can be closely related to sleep disturbances. Therefore, menopausal hormone therapy (MHT) should be considered as the treatment of choice among pharmacological treatments, following cognitive behavioral therapy, which is suggested as the first-line treatment in the general population insomnia treatment guidelines. Additionally, melatonin and 5HT-based drugs, which have fewer side effects, along with MHT should be preferentially recommended in menopausal women. However, there is still a lack of standards on the general approach and treatment for insomnia in menopausal women, and more large-scale prospective studies are needed for further insight on the roles of various treatments for insomnia in menopausal women. Thus, until then, menopausal women with insomnia also need an individualized approach and treatment (MHT, prolonged-release melatonin, 5HT-based drugs, etc.) under the premise that CBT should be used as the first-line treatment, following the treatment guidelines of insomnia for the general population.
References
- Pengo, M.F.; Won, C.H.; Bourjeily, G. Sleep in Women Across the Life Span. Chest 2018, 154, 196–206.
- Jehan, S.; Masters-Isarilov, A.; Salifu, I.; Zizi, F.; Jean-Louis, G.; Pandi-Perumal, S.R.; Gupta, R.; Brzezinski, A.; McFarlane, S.I. Sleep disorders in postmenopausal women. J. Sleep Disord. Ther. 2015, 4, 212.
- Kravitz, H.M.; Zhao, X.; Bromberger, J.T.; Gold, E.B.; Hall, M.H.; Matthews, K.A.; Sowers, M.R. Sleep disturbance during the menopausal transition in a multi-ethnic community sample of women. Sleep 2008, 31, 979–990.
- Edinger, J.D.; Bonnet, M.H.; Bootzin, R.R.; Doghramji, K.; Dorsey, C.M.; Espie, C.A.; Jamieson, A.O.; McCall, W.V.; Morin, C.M.; Stepanski, E.J. Derivation of research diagnostic criteria for insomnia: Report of an American Academy of Sleep Medicine Work Group. Sleep 2004, 27, 1567–1596.
- Khan, M.S.; Aouad, R. The Effects of Insomnia and Sleep Loss on Cardiovascular Disease. Sleep Med. Clin. 2017, 12, 167–177.
- Lee, K.A.; Baker, F.C. Sleep and Women’s Health Across the Lifespan. Sleep Med. Clin. 2018, 13, xv–xvi.
- Zhang, B.; Wing, Y.K. Sex differences in insomnia: A meta-analysis. Sleep 2006, 29, 85–93.
- Sateia, M.J. International classification of sleep disorders. Chest 2014, 146, 1387–1394.
- Bruyneel, M. Sleep disturbances in menopausal women: Aetiology and practical aspects. Maturitas 2015, 81, 406–409.
- Gold, E.B.; Sternfeld, B.; Kelsey, J.L.; Brown, C.; Mouton, C.; Reame, N.; Salamone, L.; Stellato, R. Relation of demographic and lifestyle factors to symptoms in a multi-racial/ethnic population of women 40-55 years of age. Am. J. Epidemiol. 2000, 152, 463–473.
- Xu, Q.; Lang, C.P. Examining the relationship between subjective sleep disturbance and menopause: A systematic review and meta-analysis. Menopause 2014, 21, 1301–1318.
- Ohayon, M.M. Severe hot flashes are associated with chronic insomnia. Arch. Intern. Med. 2006, 166, 1262–1268.
- Lampio, L.; Saaresranta, T.; Engblom, J.; Polo, O.; Polo-Kantola, P. Predictors of sleep disturbance in menopausal transition. Maturitas 2016, 94, 137–142.
- Woods, N.F.; Mitchell, E.S. Sleep symptoms during the menopausal transition and early postmenopause: Observations from the Seattle Midlife Women’s Health Study. Sleep 2010, 33, 539–549.
- Tandon, V.R.; Sharma, S.; Mahajan, A.; Mahajan, A.; Tandon, A. Menopause and Sleep Disorders. J. Midlife Health 2022, 13, 26–33.
- Baker, F.C.; de Zambotti, M.; Colrain, I.M.; Bei, B. Sleep problems during the menopausal transition: Prevalence, impact, and management challenges. Nat. Sci. Sleep 2018, 10, 73–95.
- Sateia, M.J.; Buysse, D.J.; Krystal, A.D.; Neubauer, D.N.; Heald, J.L. Clinical Practice Guideline for the Pharmacologic Treatment of Chronic Insomnia in Adults: An American Academy of Sleep Medicine Clinical Practice Guideline. J. Clin. Sleep Med. 2017, 13, 307–349.
- Riemann, D.; Baglioni, C.; Bassetti, C.; Bjorvatn, B.; Dolenc Groselj, L.; Ellis, J.G.; Espie, C.A.; Garcia-Borreguero, D.; Gjerstad, M.; Gonçalves, M.; et al. European guideline for the diagnosis and treatment of insomnia. J. Sleep Res. 2017, 26, 675–700.
- Haynes, J.; Talbert, M.; Fox, S.; Close, E. Cognitive Behavioral Therapy in the Treatment of Insomnia. South. Med. J. 2018, 111, 75–80.
- Dopheide, J.A. Insomnia overview: Epidemiology, pathophysiology, diagnosis and monitoring, and nonpharmacologic therapy. Am. J. Manag. Care 2020, 26, S76–S84.
- Cintron, D.; Lipford, M.; Larrea-Mantilla, L.; Spencer-Bonilla, G.; Lloyd, R.; Gionfriddo, M.R.; Gunjal, S.; Farrell, A.M.; Miller, V.M.; Murad, M.H. Efficacy of menopausal hormone therapy on sleep quality: Systematic review and meta-analysis. Endocrine 2017, 55, 702–711.
- Welton, A.J.; Vickers, M.R.; Kim, J.; Ford, D.; Lawton, B.A.; MacLennan, A.H.; Meredith, S.K.; Martin, J.; Meade, T.W. Health related quality of life after combined hormone replacement therapy: Randomised controlled trial. BMJ 2008, 337, a1190.
- Gambacciani, M.; Ciaponi, M.; Cappagli, B.; Monteleone, P.; Benussi, C.; Bevilacqua, G.; Vacca, F.; Genazzani, A.R. Effects of low-dose, continuous combined hormone replacement therapy on sleep in symptomatic postmenopausal women. Maturitas 2005, 50, 91–97.
- Gambacciani, M.; Rosano, G.; Cappagli, B.; Pepe, A.; Vitale, C.; Genazzani, A.R. Clinical and metabolic effects of drospirenone-estradiol in menopausal women: A prospective study. Climacteric 2011, 14, 18–24.
- Kagan, R.; Constantine, G.; Kaunitz, A.M.; Bernick, B.; Mirkin, S. Improvement in sleep outcomes with a 17β-estradiol-progesterone oral capsule (TX-001HR) for postmenopausal women. Menopause 2018, 26, 622–628.
- Ensrud, K.E.; Guthrie, K.A.; Hohensee, C.; Caan, B.; Carpenter, J.S.; Freeman, E.W.; LaCroix, A.Z.; Landis, C.A.; Manson, J.; Newton, K.M.; et al. Effects of estradiol and venlafaxine on insomnia symptoms and sleep quality in women with hot flashes. Sleep 2015, 38, 97–108.
- Lindberg, E.; Bonsignore, M.R.; Polo-Kantola, P. Role of menopause and hormone replacement therapy in sleep-disordered breathing. Sleep Med. Rev. 2020, 49, 101225.
- Mirer, A.G.; Peppard, P.E.; Palta, M.; Benca, R.M.; Rasmuson, A.; Young, T. Menopausal hormone therapy and sleep-disordered breathing: Evidence for a healthy user bias. Ann. Epidemiol. 2015, 25, 779–784.e771.
- Griffin, C.E., 3rd; Kaye, A.M.; Bueno, F.R.; Kaye, A.D. Benzodiazepine pharmacology and central nervous system-mediated effects. Ochsner J. 2013, 13, 214–223.
- Dorsey, C.M.; Lee, K.A.; Scharf, M.B. Effect of zolpidem on sleep in women with perimenopausal and postmenopausal insomnia: A 4-week, randomized, multicenter, double-blind, placebo-controlled study. Clin. Ther. 2004, 26, 1578–1586.
- Joffe, H.; Petrillo, L.; Viguera, A.; Koukopoulos, A.; Silver-Heilman, K.; Farrell, A.; Yu, G.; Silver, M.; Cohen, L.S. Eszopiclone improves insomnia and depressive and anxious symptoms in perimenopausal and postmenopausal women with hot flashes: A randomized, double-blinded, placebo-controlled crossover trial. Am. J. Obs. Gynecol. 2010, 202, 171.e1–171.e11.
- French, D.D.; Spehar, A.M.; Campbell, R.R.; Palacios, P.; Coakley, R.W.; Coblio, N.; Means, H.; Werner, D.C.; Angaran, D.M. Advances in Patient Safety Outpatient Benzodiazepine Prescribing, Adverse Events, and Costs. In Advances in Patient Safety: From Research to Implementation (Volume 1: Research Findings); Henriksen, K., Battles, J.B., Marks, E.S., Lewin, D.I., Eds.; Agency for Healthcare Research and Quality (US): Rockville, MD, USA, 2005.
- Loprinzi, C.L.; Sloan, J.; Stearns, V.; Slack, R.; Iyengar, M.; Diekmann, B.; Kimmick, G.; Lovato, J.; Gordon, P.; Pandya, K.; et al. Newer antidepressants and gabapentin for hot flashes: An individual patient pooled analysis. J. Clin. Oncol. 2009, 27, 2831–2837.
- Biglia, N.; Bounous, V.E.; De Seta, F.; Lello, S.; Nappi, R.E.; Paoletti, A.M. Non-hormonal strategies for managing menopausal symptoms in cancer survivors: An update. Ecancermedicalscience 2019, 13, 909.
- Ensrud, K.E.; Joffe, H.; Guthrie, K.A.; Larson, J.C.; Reed, S.D.; Newton, K.M.; Sternfeld, B.; Lacroix, A.Z.; Landis, C.A.; Woods, N.F.; et al. Effect of escitalopram on insomnia symptoms and subjective sleep quality in healthy perimenopausal and postmenopausal women with hot flashes: A randomized controlled trial. Menopause 2012, 19, 848–855.
- Huang, H.; Wang, F.; Chen, Y.; Kong, S.; Huang, Q.; Lyu, D.; Yang, W.; Wei, Z.; Qian, N.; Zhang, M.; et al. Difference in the regulation of biological rhythm symptoms of Major depressive disorder between escitalopram and mirtazapine. J. Affect. Disord. 2022, 296, 258–264.
- Schutte-Rodin, S.; Broch, L.; Buysse, D.; Dorsey, C.; Sateia, M. Clinical guideline for the evaluation and management of chronic insomnia in adults. J. Clin. Sleep Med. 2008, 4, 487–504.
- Claustrat, B.; Leston, J. Melatonin: Physiological effects in humans. Neurochirurgie 2015, 61, 77–84.
- Bellipanni, G.; Di Marzo, F.; Blasi, F.; Di Marzo, A. Effects of melatonin in perimenopausal and menopausal women: Our personal experience. Ann. N. Y. Acad. Sci. 2005, 1057, 393–402.
- Wilson, S.J.; Nutt, D.J.; Alford, C.; Argyropoulos, S.V.; Baldwin, D.S.; Bateson, A.N.; Britton, T.C.; Crowe, C.; Dijk, D.J.; Espie, C.A.; et al. British Association for Psychopharmacology consensus statement on evidence-based treatment of insomnia, parasomnias and circadian rhythm disorders. J. Psychopharmacol. 2010, 24, 1577–1601.
- Wade, A.G.; Ford, I.; Crawford, G.; McMahon, A.D.; Nir, T.; Laudon, M.; Zisapel, N. Efficacy of prolonged release melatonin in insomnia patients aged 55-80 years: Quality of sleep and next-day alertness outcomes. Curr. Med. Res. Opin. 2007, 23, 2597–2605.
- Yi, M.; Wang, S.; Wu, T.; Zhang, X.; Jiang, L.; Fang, X. Effects of exogenous melatonin on sleep quality and menopausal symptoms in menopausal women: A systematic review and meta-analysis of randomized controlled trials. Menopause 2021, 28, 717–725.
- Chung, S.; Youn, S.; Park, B.; Lee, S.; Kim, C. The Effectiveness of Prolonged-Release Melatonin in Primary Insomnia Patients with a Regular Sleep-Wake Cycle. Sleep Med. Res. 2016, 7, 16–20.
More
Information
Subjects:
Obstetrics & Gynaecology
Contributor
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
533
Revisions:
2 times
(View History)
Update Date:
19 Mar 2024
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




