Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Sol Ferrán | -- | 3107 | 2024-03-12 17:55:54 | | | |
| 2 | Sirius Huang | Meta information modification | 3107 | 2024-03-13 03:00:00 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Ferrán, S.; Garaycochea, O.; Terrasa, D.; Díaz Zufiaurre, N.; Alcalde, J.; Fernández, S. Muscle Tension Dysphonia. Encyclopedia. Available online: https://encyclopedia.pub/entry/56174 (accessed on 07 February 2026).
Ferrán S, Garaycochea O, Terrasa D, Díaz Zufiaurre N, Alcalde J, Fernández S. Muscle Tension Dysphonia. Encyclopedia. Available at: https://encyclopedia.pub/entry/56174. Accessed February 07, 2026.
Ferrán, Sol, Octavio Garaycochea, David Terrasa, Natalia Díaz Zufiaurre, Juan Alcalde, Secundino Fernández. "Muscle Tension Dysphonia" Encyclopedia, https://encyclopedia.pub/entry/56174 (accessed February 07, 2026).
Ferrán, S., Garaycochea, O., Terrasa, D., Díaz Zufiaurre, N., Alcalde, J., & Fernández, S. (2024, March 12). Muscle Tension Dysphonia. In Encyclopedia. https://encyclopedia.pub/entry/56174
Ferrán, Sol, et al. "Muscle Tension Dysphonia." Encyclopedia. Web. 12 March, 2024.
Copy Citation
Muscle Tension Dysphonia (MTD) is a relatively new clinical entity that, despite being one of the most frequent causes of functional dysphonia, is little-known by many otorhinolaryngologists. MTD has been defined as a functional voice disorder characterized by excessive tension in the extrinsic laryngeal musculature during phonation but without organic or neurological alterations.
muscle tension dysphonia
speech therapy
hyperfunction
1. Introduction
The term known as “Muscle Tension Dysphonia” (MTD) is relatively new. It has taken a matter of years to reach the entity that we know today with this name, due to the lack of knowledge of its pathophysiology. A few years ago, all dysphonia devoid of organic lesions in the vocal folds were classified as functional voice disorders, and certain psychological characteristics were assumed in these patients [1].
Over the last decade, MTD has been defined as a functional voice disorder characterized by excessive tension in the extrinsic laryngeal musculature during phonation but without organic or neurological alterations [1]. The increase in muscular tension generates an abnormal laryngeal position during phonation: the larynx is elevated, and there is some degree of glottic and/or supraglottic compression. This affects the position of cartilaginous structures and, therefore, affects the intrinsic musculature of the larynx, the vocal folds, and glottic closure during phonation, resulting in changes in qualities of the voice. A decade ago, it comprised approximately 10–40% of clinical cases in voice centers [2][3].
Based on the mechanism that unleashes this increase in muscular tension, MTD is classified in the “Classification manual for voice disorders-I, 2006” into primary or secondary types. Primary MTD is characterized by an increase in tension that is independent of any external mechanism: it is an alteration of the phonation mechanism itself. In secondary MTD, the mechanism responsible for the increase in muscular tension is a compensatory reaction to a mechanism that alters the function or structure of the glottis [4].
History
The origin and foundations of what is currently known as Muscle Tension Dysphonia (MTD) lie in the early 1980s. In 1982, Koufman and Blalock [5], in an attempt to better define and organize functional disorders of the voice, proposed a way to classify these disorders by dividing them into five big groups: conversion reaction, postviral chronic hoarseness, inappropriate falsetto, postoperative dysphonia, and vocal misuse/abuse syndromes. Half of the patients belonged to the group with vocal misuse or abuse syndromes (VMS). Moreover, most of the patients in the VMS group had altered skeletal laryngeal muscle tension, characterized by chronic intermittent dysphonia and vocal fatigue. On this basis, the authors decided to refer to this disorder as laryngeal tension–fatigue syndrome (TFS). This type of disorder affected, according to the authors, 25% of all functional voice disorders [5]. Moreover, the authors differentiated TFS in the voices professional and non-professional subjects. According to the authors, in the former, the tone of the voice is very low, while, in the non-professionals, the tone of the voice is variable. TFS syndrome in voice professionals was labeled as Bogart–Bacall syndrome [6].
TFS was the predecessor of what is currently known as Muscle Tension Dysphonia (MTD), since TFS is a functional voice disorder characterized by an alteration of tone but with a normal appearance of the larynx by physical examination. The concept of TFS, however, was limited by the fact that it only applied to cases in which the origin of the dysphonia was VMS; it did not cover other possible etiological factors [1].
The term MTD was first used in 1983 by Morrison and Rammage [7]. In their work, these authors described the clinical characteristics of young people who made excessive use of the voice under stress. As in TFS, the authors found an increase in muscle tension in MTD. They assessed this muscle tension by palpation of the extrinsic laryngeal musculature and by means of laryngeal fibroscopy when evaluating the behavior of the larynx during phonation [8]. However, the principal difference between MTD and TFS, and the reason why the new term came to be more-widely used internationally, is that MTD denotes a pathological condition in which the increased laryngeal and/or para-laryngeal muscle tension can be caused by diverse etiological factors. The newer term covers a clinical disorder that can arise from various factors and not just VMS [1].
2. Etiology and Physiopathology
As has already been mentioned, MTD can be primary or secondary. The alteration in muscular activity in primary MTD has been associated with inappropriate use of the voluntary muscles used in phonation related to the personality. Imaging studies of brain function have demonstrated the presence of functional alterations in the limbic–motor system and in the behavioral inhibition system [9][10]. In secondary MTD, the mechanism responsible for the increase in muscular tension is a compensatory reaction to a mechanism that alters the function or structure of the glottis. The principal mechanisms that have been shown to lead to secondary MTD are upper respiratory tract infections [11], glottic insufficiency [1][12][13], laryngopharyngeal reflux [13][14], structural lesions of the VC [15], spasmodic dysphonia [16], and hormonal alterations [17][18].
The phonatory hyperfunction characteristic of MTD can contribute to the development of traumatic lesions such as nodules or polyps on the VC [8]. However, in those cases in which MTD is associated with organic lesions, it remains to be elucidated whether it is the MTD that brings about the organic pathology or whether the MTD is the result of that pathology. Therefore, it is not always easy to distinguish between a primary or a secondary MTD.
3. Diagnosis
The principal symptoms of MTD are dysphonia and vocal fatigue. Patients with MTD usually manifest increased phonatory effort, accompanied by a reduction or worsening in voice quality. Some patients have symptoms such as tension, pain in the cervical region, and sensations of itchiness, dryness, irritation, or even the presence of a foreign body in the larynx area. Although the symptoms are always a subjective parameter in the diagnosis, there are some scales that can be used to assess them, such as the Vocal Tract Discomfort scale [19]. VHI results show worse scores in patients with this pathology [20][21].
Observation of the larynx during phonation is indispensable in the diagnosis. It can rule out an underlying organic pathology or a secondary MTD, and it can determine the type of MTD.
Garaycochea [22] discusses the three most frequent laryngoscopic profiles in these patients. Anteroposterior supraglottic contraction involves the reduction in the visibility of the vocal cords (VC) at both their anterior and posterior borders. The reduction in visibility of the posterior border is related to approximation of the arytenoids due to an increase in their rotation. At the anterior level, the increase in tension and increased elevation of the laryngeal musculature produces bowing of the epiglottic petiole towards the laryngeal lumen, which makes it difficult to see the anterior border of the VC, starting with visual obstruction of the anterior commissure [1][20]. Supraglottic lateral contraction results in reduction in the visibility of the width of the VC. The reduction ranges from visual obstruction of the laryngeal ventricle to complete visual obstruction of the vocal cords by the ventricular bands, (False VC phonation). To date, the muscle structure and innervation of the ventricular bands remain poorly understood and areas of controversy; the same applies to the role of the ventricular bands (VB) in normal phonation and in phonation by people with voice alterations. Posterior glottic gap (PGG) refers to an incomplete closure of the VC at their posterior edge. This originates from an attempted contraction of the lateral and interarytenoid cricoarytenoid muscle accompanied by insufficient relaxation of the posterior cricoarytenoid muscle [7]. The low incidence of PGG relative to that of supraglottic compression in patients with MTD is attributable to the difficulty, in many cases, of observing PGG when there is concomitant supraglottic compression [22].
There have been different proposals of classification systems based on the laryngoscopic profiles during phonation. The first system was written by Morrison in 1986 [8]. While this initial classification did differentiate patients with MTD from patients with psychogenic functional dysphonia, it has been progressively modified by different authors over the last few years. Sama considers psychogenic functional dysphonia profiles as profiles of MTD and excludes those profiles related to organic lesions [23]. Belafsky excludes the presence of “bowing” during phonation because bowing is related to underlying glottic insufficiency and not to hyperfunction [24][25]. A second scoring system was described by Van Lawrence in 1987 [26], and a third was described by Koufman in 1991 [27]. In 2020, Fernández et al. [20] published a new classification (Universidad de Navarra) based on subglottal pressure (SgP) values, which has been demonstrated to be related to the degree of anteroposterior (AP) compression (Figure 1). The higher the SgP value, the higher the degree of AP compression. This classification system uses the endoscopic profiles mentioned above and assumes that AP contraction is present. While the classic classifications only allow choosing between one of the phonatory profiles, excluding the other ones, the latest classification proposed by Fernández et al. is based on a single laryngoscopic profile, but it makes it possible to associate LC or PGG, if present, and provide a more detailed description from the physical examination.
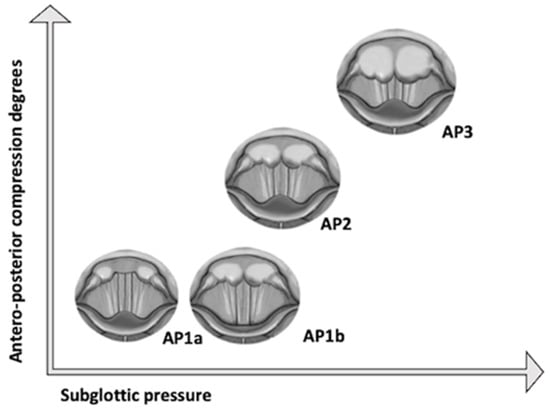
Figure 1. Classification of Universidad de Navarra.
Considering these more frequent profiles in MTD, it should be noted that, in some cases, increased rotation of the arytenoids may compress the VB and create the appearance of a vocal false folds phonation. Therefore, it is important to know how to interpret the role of this phenomenon in patients with dysphonia, including MTD, since there is not enough evidence to justify attributing any clinical value to this characteristic. While it is true that lateral compression (LC) can be present in MTD, according to work carried out by Stager and Behrman, this is not necessarily related to the degree, the seriousness, or the stage of dysphonia; as a clinical and diagnostic indicator, LC has less value than AP compression [27][28]. As it has been found and reported previously, the best way to conduct the physical examination is with a transnasal fiberoptic laryngoscopy, because it is not possible to evaluate compression of the supraglottis well with a fixed lens. Stroboscopy is limited by the supraglottic compression, which can block the vision of the VC [29].
In patients with MTD, the higher the SgP value, the higher the degree of AP compression. AP1a: The anterior commissure is not visible during phonation; AP1b: Vocal processes are not visible during phonation due to the medial approximation of the arytenoids; AP2: only 2/3 of the vocal fold length is visible during phonation.
As for acoustic analysis, although there are few studies that focus exclusively on this technique for the diagnosis of MTD, most of them include it. Although there is no characteristic pattern for this pathology, or a specific parameter with a characteristic alteration in patients with MTD, it is a technique that will always provide useful information on the phonatory function of a patient.
A possible use of acoustic analysis in patients with MTD is to differentiate between MTD and spasmodic dysphonia (SD). Interruptions in an acoustic signal are highly suggestive of SD and can be a determining factor when differentiating between SD and MTD in severe cases [16][30].
There is a parameter that began to be studied in 2010 by Stepp et al. [31], the RFF, from which it seems that biomechanical elements can be inferred. It is defined as the fundamental frequency of the cycles immediately preceding and following the production of a voiceless consonant, normalized by the “steady-state” fundamental frequencies of the voicing preceding and following the consonant (during a vowel–voiceless consonant–vowel (VCV) utterance). After several studies on this parameter, there is evidence that it may be an acoustic indicator of laryngeal tension. The studies that have compared the RFF of healthy subjects with that of patients with vocal hyperfunction have found significantly lower RFF values in the latter, although it is still not clear which values provide more information on laryngeal tension: those prior to the voiceless consonant or those after it. There is also evidence of its usefulness as a clinical follow-up tool to quantify progress before and after therapy [31][32][33]. However, its analysis has not yet been standardized in clinical voice evaluation, partly because it is currently very time-consuming to perform manually, and also because it requires lengthy training to properly identify the last cycles of a vocal transition [34]. More research is needed to prove its clinical utility and to better understand its underlying physiology, but it may be a very interesting parameter in the study of MTD.
Aerodynamic analysis has proven to be a very useful tool in the evaluation of voice alterations. Among the parameters studied, SgP has the lowest variance in subjects without a voice alteration, and, in contrast to GF, SgP is not affected significantly by age or sex [35][36]. In addition, as already mentioned, its relationship with the degree of anteroposterior compression has been demonstrated, so its study is of great value for the diagnosis of MTD. Espinoza et al. [37] studied the aerodynamic pattern in women with vocal hyperfunction, distinguishing between phonotraumatic (PVH) and non-phonotraumatic (NPVH) VH, and found that, in those women with PVH, all measured parameters (subglottal air pressure, peak-to-peak airflow, maximum flow declination rate, and open quotient) had significantly reduced sound pressure level (SPL)-normalized values than the control group, while women with NPVH had lower values for SgP and open quotient. This means that higher than normal levels of these parameters are needed to achieve a given SPL. Other aerodynamic profiles described in patients with MTD in which there is no increase in SgP are the presence of reduced GF or increased LR.
EMG can detect changes in the activity of extrinsic musculature in patients with vocal hyperfunction and MTD. However, these are not constant in all patients, only evaluate extrinsic musculature, are affected to varying degrees by the thickness of subcutaneous and contraction of the platysma, and they cannot reveal whether vocal pathology is due to an increase in tension of extrinsic musculature or due to an increase in tension of intrinsic musculature [38][39].
As previously mentioned, in this pathology there is an abnormal laryngeal position during phonation, with the larynx higher than normal. The use of X-rays provides an objective measure of the height of the larynx during phonation. The main downside to this technique is the radiation that the patient is exposed to [40].
Lastly, the administration of intravenous midazolam has been proposed not only as a treatment, but also as a diagnostic method for MTD by subjective and perceptual improvement of voice quality [11].
In parallel with all the diagnostic techniques studied, it is important to make a thorough differential diagnosis and to rule out neurological, psychiatric, and organic alterations that can explain the dysphonia of a patient.
4. Treatment
Treatment approaches can be classified as indirect (vocal education) or direct interventions. Intervention usually involves a combination of direct and indirect treatment approaches for successful outcomes and begins by addressing vocal hygiene [41].
The patient must understand that his or her voice is a combination of multiple factors, including possible psychological influences. Vocal education includes a series of general measures (environmental, behavioral, and related to vocal use) that seek to modify and avoid possible factors that are related to altered vocal behavior. Some examples would be talking as little as possible in an environment where there is a lot of background noise, avoiding shouting, trying not to whisper, or using good breathing techniques [1].
Direct approaches to voice therapy aim at modifying the physiology of the vocal mechanism through symptomatic vocal therapy or the physiological principles of vocal therapy [41].
Physiological voice therapy programs strive to balance the three subsystems of voice production (respiration, phonation, and resonance) rather than working directly on isolated voice symptoms [42]. They include techniques such as the Accent Method, Conversation Training Therapy (CTT), Expiratory Muscle Strength Training (EMST), Lee Silverman Voice Treatment (LSVT), Manual Circumlaryngeal Techniques, Phonation Resistance Training Exercises (PhoRTE), Resonant Voice Therapy (RVT), Stretch and Flow Phonation, and Vocal Function Exercises (VFEs).
As previously shown, results with many of these techniques have been published for the treatment of MTD. The RVT deserves a special mention for being one of the most widely used. The goal of RVT is to produce the most powerful and “clean” voice possible with the least effort and impact between the vocal folds to minimize the likelihood of injury and maximize the likelihood of vocal health [41]. It attempts to have patients produce an oral voice localized to the anterior alveolar ridge or adjacent facial plates [43], which is derived from the principles of a semi-occluded vocal tract [44]. Semi-occlusion occurs at the ends of the resonant cavities, which reduces unnecessary pressure at the vocal fold level [41]. One of the exercises included in this program is humming, used as a treatment for MTD with improvements in supraglottic compression and EGG parameters [45][46].
Within the manual laryngeal techniques (first described in 1993) [47], there are also many different maneuvers described. MCT was developed by Aronson and Roy and Leeper [48], and it is based on the application of pressure, massage, to different points of the larynx. It starts with a circular compression on the hyoid bone, the thyrohyoid space, and the posterior borders of the thyroid cartilage. Lastly, the whole larynx is moved down and laterally. During the technique, the patient vocalizes sustained vowels or hums so that changes in vocal quality can be tracked [47]. The objective of MCT is to reduce the increased tension and muscular contraction, especially around the hio-laryngeal musculature [47][49][50][51]. The LMT proposed by Mathieson (MLMT) consists of rotational massage, kneading, and stretching of the perilaryngeal muscles (sternocleidomastoid muscles). Although these muscles are not directly related to laryngeal function, patients frequently complain of stiffness and tenderness in them in association with their voice disorders [52]. The cricothyroid visor maneuver (CVM) was proposed by Dehqan et al. [53] based on the findings of Harris and Lieberman [54], who reported that abnormal patterns of muscle activity can develop in the cricothyroid muscle and visor mechanism, which may contribute to voice problems, and manipulation of this muscle and articulation can lead to remarkable improvement in the voice. A lower range of action of the cricothyroid visor has also been identified in patients with MTD, probably associated with a reduced efficiency of cricothyroid muscle activity.
There are also multiple techniques focused on the modification of vocal symptoms or perceptual voice components, which are also used for the treatment of patients with MTD: Amplification, Auditory Masking, Biofeedback, Chant Speech, Confidential Voice, Inhalation Phonation, Posture, Relaxation, Semi-Occluded Vocal Tract (SOVT) Exercises, Twang Therapy, and Yawn–Sigh [55].
In secondary MTD, part of the treatment must be oriented towards treating the cause involved in the genesis of the increase in muscular tension. Surgical treatment is usually complemented with both vocal education and rehabilitation. Medical treatment has been described in MTD in the context of respiratory tract infections, sinusitis, allergy, and laryngopharyngeal reflux [56].
References
- Van Houtte, E.; Van Lierde, K.; Claeys, S. Pathophysiology and Treatment of Muscle Tension Dysphonia: A Review of the Current Knowledge. J. Voice 2011, 25, 202–207.
- Craig, J.; Tomlinson, C.; Stevens, K.; Kotagal, K.; Fornadley, J.; Jacobson, B.; Garrett, C.G.; Francis, D.O. Combining voice therapy and physical therapy: A novel approach to treating muscle tension dysphonia. J. Commun. Disord. 2015, 58, 169–178.
- Bhattacharyya, N. The Prevalence of Voice Problems among Adults in the United States. Laryngoscope 2014, 124, 2359–2362. Available online: https://pubmed.ncbi.nlm.nih.gov/24782443/ (accessed on 20 February 2024).
- Verdolini, A.K.; Rosen, C.A.; Branski, R.C. Classification Manual for Voice Disorders-I; Psychology Press: East Sussex, UK, 2006.
- Sambhu, M.; Goh, T.; Golan, H.; Pisegna, J.; Noordzij, J.P. Evaluating the use of baclofen as adjunct treatment for muscle tension dysphonia. Am. J. Otolaryngol. 2022, 43, 103309.
- Koufman, J.A.; Blalock, P.D. Classification and Approach to Patients with Functional Voice Disorders. Ann. Otol. Rhinol. Laryngol. 1982, 91, 372–377.
- Koufman, J.A.; Blalock, P.D. Vocal fatigue and dysphonia in the professional voice user: Bogart-bacall syndrome. Laryngoscope 1988, 98, 493–498.
- Morrison, M.D.; A Rammage, L.; Belisle, G.M.; Pullan, C.B.; Nichol, H. Muscular tension dysphonia. J. Otolaryngol. 1983, 12, 302–306.
- Kryshtopava, M.; Van Lierde, K.; Meerschman, I.; D’Haeseleer, E.; Vandemaele, P.; Vingerhoets, G.; Claeys, S. Brain Activity During Phonation in Women with Muscle Tension Dysphonia: An fMRI Study. J. Voice 2017, 31, 675–690.
- Roy, N.; Dietrich, M.; Blomgren, M.; Heller, A.; Houtz, D.R.; Lee, J. Exploring the Neural Bases of Primary Muscle Tension Dysphonia: A Case Study Using Functional Magnetic Resonance Imaging. J. Voice 2019, 33, 183–194.
- Bhalla, R.; Wallis, J.; Kaushik, V.; de Carpentier, J. How we do it: Adjunctive intravenous midazolam: Diagnosis and treatment of therapy-resistant muscle tension dysphonia. Clin. Otolaryngol. 2005, 30, 367–369.
- Novakovic, D.; Nguyen, D.D.; Chacon, A.; Madill, C. Injection laryngoplasty as adjunct treatment method for muscle tension dysphonia: Preliminary findings. Laryngoscope 2020, 130, 980–985.
- Angsuwarangsee, T.; Morrison, M. Extrinsic Laryngeal Muscular Tension in Patients with Voice Disorders. J. Voice 2002, 16, 333–343.
- Cohen, S.M.; Garrett, C.G. Hoarseness: Is It Really Laryngopharyngeal Reflux? Laryngoscope 2008, 118, 363–366.
- Altman, K.W.; Atkinson, C.; Lazarus, C. Current and Emerging Concepts in Muscle Tension Dysphonia: A 30-Month Review. J. Voice 2005, 19, 261–267.
- Roy, N. Differential diagnosis of muscle tension dysphonia and spasmodic dysphonia. Curr. Opin. Otolaryngol. Head Neck Surg. 2010, 18, 165–170.
- D’haeseleer, E.; Depypere, H.; Claeys, S.; Van Borsel, J.; Van Lierde, K. The menopause and the female larynx, clinical aspects and therapeutic options: A literature review. Maturitas 2009, 64, 27–32.
- Abitbol, J.; Abitbol, P.; Abitbol, B. Sex hormones and the female voice. J. Voice 1999, 13, 424–446.
- Torabi, H.; Khoddami, S.M.; Ansari, N.N.; Dabirmoghaddam, P. The Vocal Tract Discomfort Scale: Validity and Reliability of the Persian Version in the Assessment of Patients with Muscle Tension Dysphonia. J. Voice 2016, 30, 711–716.
- Fernández, S.; Garaycochea, O.; Martinez-Arellano, A.; Alcalde, J. Does More Compression Mean More Pressure? A New Classification for Muscle Tension Dysphonia. J. Speech Lang. Hear. Res. 2020, 63, 2177–2184.
- Aghadoost, S.; Jalaie, S.; Dabirmoghaddam, P.; Khoddami, S.M. Effect of Muscle Tension Dysphonia on Self-perceived Voice Handicap and Multiparametric Measurement and Their Relation in Female Teachers. J. Voice 2022, 36, 68–75.
- Garaycochea, O.; Navarrete, J.M.A.; del Río, B.; Fernández, S. Muscle Tension Dysphonia: Which Laryngoscopic Features Can We Rely on for Diagnosis? J. Voice 2019, 33, 812.e15–812.e18.
- Sama, A.; Carding, P.N.; Price, S.; Kelly, P.; Wilson, J.A. The Clinical Features of Functional Dysphonia. Laryngoscope 2001, 111, 458–463.
- Belafsky, P.C.; Postma, G.N.; Reulbach, T.R.; Holland, B.W.; Koufman, J.A. Muscle Tension Dysphonia as a Sign of Underlying Glottal Insufficiency. Otolaryngol. Head Neck Surg. 2002, 127, 448–451.
- Vaca, M.; Cobeta, I.; Mora, E.; Reyes, P. Clinical Assessment of Glottal Insufficiency in Age-related Dysphonia. J. Voice 2017, 31, 128.e1–128.e5.
- Van Lawrence, L. Suggested Criteria for Fibre-Optic Diagnosis of Vocal Hyperfunction. In Care of the Professional Voice Symposium; The British Voice Association: London, UK, 1987.
- Stager, S.V.; Bielamowicz, S.; Gupta, A.; Marullo, S.; Regnell, J.R.; Barkmeier, J. Quantification of Static and Dynamic Supraglottic Activity. J. Speech Lang. Hear Res. 2001, 44, 1245–1256.
- Behrman, A.; Dahl, L.D.; Abramson, A.L.; Schutte, H.K. Anterior-Posterior and medial compression of the supraglottis: Signs of nonorganic dysphoniaor normal postures? J. Voice 2003, 17, 403–410.
- Koufman, J.A.; Blalock, P. Functional Voice Disorders. Otolaryngol. Clin. N. Am. 1991, 24, 1059–1073.
- Sapienza, C.M.; Walton, S.; Murry, T. Adductor spasmodic dysphonia and muscular tension dysphonia: Acoustic analysis of sustained phonation and reading. J. Voice 2000, 14, 502–520.
- Stepp, C.E.; Hillman, R.E.; Heaton, J.T. The Impact of Vocal Hyperfunction on Relative Fundamental Frequency During Voicing Offset and Onset. J. Speech Lang. Hear. Res. 2010, 53, 1220–1226.
- Stepp, C.E.; Merchant, G.R.; Heaton, J.T.; Hillman, R.E.; Murray, E.S.H.; Segina, R.K.; Woodnorth, G.H.; Park, Y.; Van Stan, J.H.; Mehta, D.D.; et al. Effects of Voice Therapy on Relative Fundamental Frequency During Voicing Offset and Onset in Patients with Vocal Hyperfunction. J. Speech Lang. Hear Res. 2011, 54, 1260–1266.
- Kagan, L.S.; Heaton, J.T. The Effectiveness of Low-Level Light Therapy in Attenuating Vocal Fatigue. J. Voice 2017, 31, 384.e15–384.e23.
- McKenna, V.S.; Vojtech, J.M.; Previtera, M.; Kendall, C.L.; Carraro, K.E. A Scoping Literature Review of Relative Fundamental Frequency (RFF) in Individuals with and without Voice Disorders. Appl. Sci. 2022, 12, 8121.
- Shembel, A.C.; Lee, J.; Sacher, J.R.; Johnson, A.M. Characterization of Primary Muscle Tension Dysphonia Using Acoustic and Aerodynamic Voice Metrics. J. Voice 2021, 37, 897–906.
- Belsky, M.A.; Rothenberger, S.D.; Gillespie, A.I.; Gartner-Schmidt, J.L. Do Phonatory Aerodynamic and Acoustic Measures in Connected Speech Differ Between Vocally Healthy Adults and Patients Diagnosed with Muscle Tension Dysphonia? J. Voice 2020, 35, 663.e1–663.e7.
- Espinoza, V.M.; Zañartu, M.; Van Stan, J.H.; Mehta, D.D.; Hillman, R.E. Glottal Aerodynamic Measures in Women with Phonotraumatic and Nonphonotraumatic Vocal Hyperfunction. J. Speech Lang. Hear. Res. 2017, 60, 2159–2169.
- Hocevar-Boltezar, I.; Janko, M.; Zargi, M. Role of Surface EMG in Diagnostics and Treatment of Muscle Tension Dysphonia. Acta Oto-Laryngol. 1998, 118, 739–743.
- Van Houtte, E.; Claeys, S.; D’haeseleer, E.; Wuyts, F.; Van Lierde, K. An Examination of Surface EMG for the Assessment of Muscle Tension Dysphonia. J. Voice 2013, 27, 177–186.
- Lowell, S.Y.; Kelley, R.T.; Colton, R.H.; Smith, P.B.; Portnoy, J.E. Position of the hyoid and larynx in people with muscle tension dysphonia. Laryngoscope 2012, 122, 370–377.
- Theis, S.M.; Carlson, A. Voice Therapy. Int. J. Head Neck Surg. 2022, 13, 27–31.
- Stemple, J.C.; Glaze, L.E.; Klaben, B.G. Clinical Voice Pathology: Theory and Management, 4th ed.; Plural Publishing: San Diego, CA, USA, 2010.
- Chen, F.C.; Ma, E.P.-M.; Yiu, E.M.-L. Facial Bone Vibration in Resonant Voice Production. J. Voice 2014, 28, 596–602.
- Titze, I.R. Voice Training and Therapy with a Semi-Occluded Vocal Tract: Rationale and Scientific Underpinnings. J. Speech Lang. Hear Res. 2006, 49, 448–459.
- Ogawa, M.; Hosokawa, K.; Yoshida, M.; Iwahashi, T.; Hashimoto, M.; Inohara, H. Immediate Effects of Humming on Computed Electroglottographic Parameters in Patients with Muscle Tension Dysphonia. J. Voice 2014, 28, 733–741.
- Ogawa, M.; Hosokawa, K.; Yoshida, M.; Yoshii, T.; Shiromoto, O.; Inohara, H. Immediate Effectiveness of Humming on the Supraglottic Compression in Subjects with Muscle Tension Dysphonia. Folia Phoniatr. Logop. 2013, 65, 123–128.
- Roy, N.; Leeper, H.A. Effects of the manual laryngeal musculoskeletal tension reduction technique as a treatment for functional voice disorders: Perceptual and acoustic measures. J. Voice 1993, 7, 242–249.
- Ribeiro, V.V.; Pedrosa, V.; Silverio, K.C.A.; Behlau, M. Laryngeal Manual Therapies for Behavioral Dysphonia: A Systematic Review and Meta-analysis. J. Voice 2018, 32, 553–563.
- Dehqan, A.; Scherer, R.C. Positive Effects of Manual Circumlaryngeal Therapy in the Treatment of Muscle Tension Dysphonia (MTD): Long Term Treatment Outcomes. J. Voice 2019, 33, 866–871.
- Aghadoost, S.; Jalaie, S.; Khatoonabadi, A.R.; Dabirmoghaddam, P.; Khoddami, S.M. A Study of Vocal Facilitating Techniques Compared to Manual Circumlaryngeal Therapy in Teachers with Muscle Tension Dysphonia. J. Voice 2019, 34, 963.e11–963.e21.
- Dromey, C.; Nissen, S.L.; Roy, N.; Merrill, R.M. Articulatory Changes Following Treatment of Muscle Tension Dysphonia: Preliminary Acoustic Evidence. J. Speech Lang. Hear Res. 2008, 51, 196–208.
- Mathieson, L.; Hirani, S.; Epstein, R.; Baken, R.; Wood, G.; Rubin, J. Laryngeal Manual Therapy: A Preliminary Study to Examine its Treatment Effects in the Management of Muscle Tension Dysphonia. J. Voice 2009, 23, 353–366.
- Dehqan, A.; Ballard, K.J. An evaluation of Short-term Treatment Outcomes of Cricothyroid Visor Maneuver: A Proof-of-Concept Pilot Study. J. Voice 2021, 35, 330.e1–330.e7.
- Roy, N. Assessment and treatment of musculoskeletal tension in hyperfunctional voice disorders. Int. J. Speech-Lang. Pathol. 2008, 10, 195–209.
- Boone, D.R.; McFarlane, S.C.; Von Berg, S.L.; Zraick, R.I. The Voice and Voice Therapy; Pearson Education: Upper Saddle River, NJ, USA, 2013.
- Kandogan, T.; Aksoy, G.; Dalgic, A. Effects of Omeprazole Over Voice Quality in Muscle Tension Dysphonia Patients with Laryngopharyngeal Reflux. Iran. Red Crescent Med. J. 2012, 14, 787–791.
More
Information
Subjects:
Otorhinolaryngology
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.3K
Revisions:
2 times
(View History)
Update Date:
13 Mar 2024
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




