Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Thomas Müller | -- | 1942 | 2024-02-27 12:24:17 | | | |
| 2 | Rita Xu | Meta information modification | 1942 | 2024-02-28 03:01:54 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Müller, T.; Braden, B. Percutaneous Biliary Drainage. Encyclopedia. Available online: https://encyclopedia.pub/entry/55541 (accessed on 15 January 2026).
Müller T, Braden B. Percutaneous Biliary Drainage. Encyclopedia. Available at: https://encyclopedia.pub/entry/55541. Accessed January 15, 2026.
Müller, Thomas, Barbara Braden. "Percutaneous Biliary Drainage" Encyclopedia, https://encyclopedia.pub/entry/55541 (accessed January 15, 2026).
Müller, T., & Braden, B. (2024, February 27). Percutaneous Biliary Drainage. In Encyclopedia. https://encyclopedia.pub/entry/55541
Müller, Thomas and Barbara Braden. "Percutaneous Biliary Drainage." Encyclopedia. Web. 27 February, 2024.
Copy Citation
Ultrasound guidance in biliary interventions has become the standard tool to facilitate percutaneous biliary drainage as well as percutaneous gall bladder drainage. Monitoring of the needle tip whilst penetrating the tissue in real time using ultrasound allows precise manoeuvres and exact targeting without radiation exposure.
percutaneous biliary drainage
percutaneous gall bladder drainage
ultrasound guidance
1. Introduction
Interventions in the biliary system might target the bile ducts or the gall bladder. The two most commonly practised procedures are percutaneous transhepatic biliary drainage (PTBD) and percutaneous (transhepatic) gallbladder drainage (PGBD) [1]. Ultrasound (US) guidance of punctures and drainage placements offers some apparent advantages over “blind” punctures and fluoroscopic or computed tomography guidance. US, whether applied percutaneously or endoscopically, is the only modality that allows continuous and real-time monitoring of the needle trajectory and the advancement of the needle tip through the penetrated tissue. The reduction in or even avoidance of ionising radiation is another major benefit for the patient and doctor. Therefore, not using ultrasound might need justification.
2. Biliary Drainage
Endoscopic biliary drainage (EBD) using metal and plastic stents inserted by endoscopic retrograde cholangiography (ERC) is the standard procedure for draining the common bile duct and the intrahepatic biliary system. PTBD is an alternative approach if the major duodenal papilla is not accessible or the endoscopic approach via the papilla has failed. This might be due to postsurgical changes in the anatomy (Roux-en-Y operation and others) or if a stenosis of the biliary system cannot be overcome by the endoscopic approach [2][3][4]. PTBD does not seem to be inferior to EBD [5][6][7]. Endoscopic ultrasound-guided biliary drainage (EUS-BD) is an increasingly used third method of accessing the biliary system when ERC fails to achieve biliary drainage, but so far, this is only available in specialised centres [8][9][10]. Thus, the choice of the appropriate drainage method when EBD fails or is not applicable is “based on the location of the obstruction, the purpose of drainage (as a preoperative procedure or a palliative treatment) and level of experience in biliary drainage at individual treatment centers” [5].
Indications for PTBD include palliative treatment (e.g., bile drainage in unresectable metastases, and biliary, papillary, or pancreatic carcinoma) as well as access to minimally invasive procedures in benign diseases (dilation of benign strictures, percutaneous stone removal, drainage in cholangitis, preparing a channel for direct cholangioscopy, etc.) [2][4][11][12][13][14].
From its beginning in the 1930s and for many decades, PTBD used to be a solely fluoroscopic procedure [15]. With the increasing use of ultrasound as a diagnostic tool in the late 1970s and 1980s, US guidance for the initial puncture of bile ducts was recommended by a few radiologists. It seemed desirable to have a guidance method at hand that provided continuous monitoring of the needle’s tip and tracking through the tissues in real time. From a theoretical point of view, continuous guidance was supposed to reduce the number of needle punctures, fluoroscopy time, total procedure time, and complication rates [16][17][18][19]. Targeting bile ducts with a needle is a challenging procedure and often requires multiple passes before it is successfully achieved. Each pass increases the risk of bleeding. Ultrasound provides excellent spatial and temporal resolution and, therefore, will facilitate access to the biliary system. Over the years, US guidance has become more and more common.
After an initial puncture under ultrasound guidance, the procedure is usually continued under fluoroscopic imaging [3][20][21][22][23]. As long as only external drainage is to be obtained, US guidance alone without fluoroscopy is feasible and sufficient [17][24][25]. Without fluoroscopy, ultrasound-guided PTBD, performed at the bedside in intensive care, can be life-saving to critically ill patients who cannot be transported to a fluoroscopy suite [24].
One case series illustrates the feasibility of also achieving external–internal drainage using contrast-enhanced ultrasound. A diluted ultrasound contrast agent was administered via the percutaneously placed needle for visualising the biliary system. However, fluoroscopy was necessary for depicting the guide wire on its way through the stenosis [26]. Intrabiliary application of a diluted contrast agent may be useful for depicting drainage tips and identifying stenoses [27][28].
Fusion imaging might be used as well for the initial puncture [29], but the clinical relevance of this method, combining US and CT or MRI imaging, cannot currently be assessed.
2.1. Data Background
While since 1980, numerous feasibility studies on US guidance have been published [21][22][23][24][25][30][31], only very few studies compared US-guided vs. fluoroscopically guided initial puncture in PTBD retrospectively [32][33]. Prospective comparative studies have not been published.
An older Russian study (including a total of 89 patients) favours US guidance due to a decrease in radiation time, higher technical success, a lower number of needle passes, and decreased complication rates in the US group [32]. A larger German retrospective analysis (n = 251), on the other hand, showed no differences in the total complication rate, fluoroscopy time, and success rates [33]. A recent systematic review and meta-analysis of bleeding rates in PTBD found no reduction in the US group [34].
Other authors compare their results from US-guided PTBD to data from the literature and suggest lower complication rates [30] or a lower radiation time [23][31].
2.2. How to Perform US-Guided PTBD
US-guided PTBD is performed under sterile conditions, including protective clothing, skin disinfection, sterile covers on keyboards and probes, and sterile drapes [35][36]. Local anaesthesia of the parietal peritoneum and liver capsule is mandatory. Researchers usually do not administer sedative medication in order to maintain a patient’s cooperation (particularly for breath holding).
The biliary system can be punctured in the right or left liver lobe, depending on the level of obstruction or medical needs. In dilated intrahepatic ducts, accessing the bile ducts with a needle and advancing a wire with the subsequent placement of drainage is easier, and adverse events are fewer than in nondilated ducts. It is also possible to access nondilated ducts, but ideally, a duct with a diameter of ≥3 mm should be aimed for. As bile ducts run in parallel to portal veins, nondilated bile ducts can be found by using colour Doppler and heading for a portal vessel visualised thereby—the so-called parallel technique [20][31][37][38][39]. Ideally, the angle between the duct and needle should be less than 90 degrees [40].
PTBD is commonly performed in the so-called “in plane technique” (Figure 1a,b).
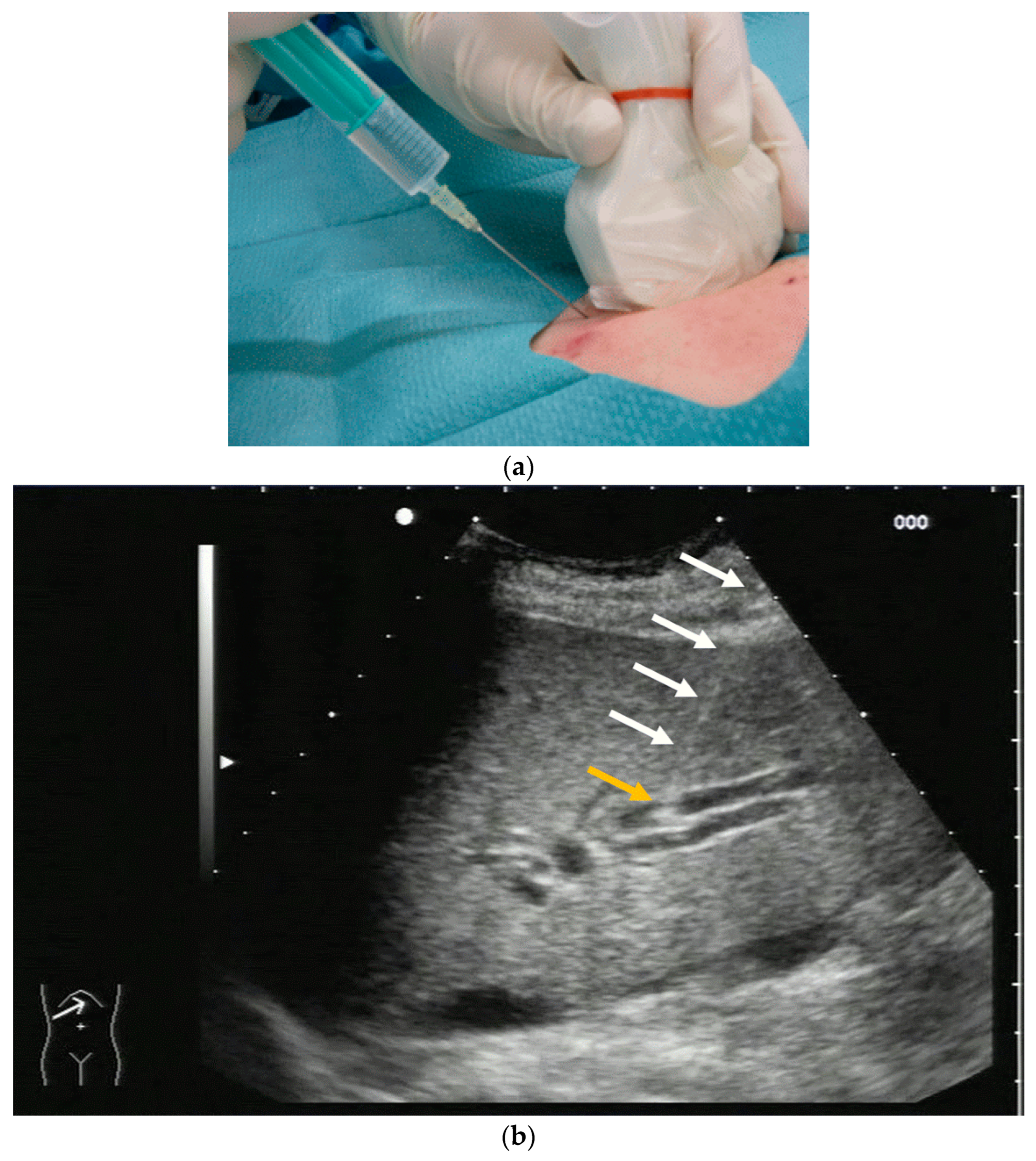
Figure 1. (a) Puncture in plane. The needle is inserted at the centre of the small side of the transducer; (b) Needle tip (yellow arrow), body (white arrows), and target (bile duct) are depicted in one plane. The needle tip is kept in plane by very small movements of the transducer.
The needle is inserted at the narrow side of the transducer and advanced in the US plane. It can thereby be depicted on its whole trajectory. For a successful puncture, the interventionalist has to keep the needle shaft, tip, and target (bile duct) on the image at all times. Losing the tip or the target being out of sight will obviously prohibit a successful puncture. Not having the needle shaft in sight but seeing the tip and target means the further trajectory of the needle will miss the bile duct. Careful tiny corrections, either of the probe orientation or needle direction, must then be undertaken to have all three in sight during the procedure.
A needle-holding attachment (Figure 2) can be used. It will facilitate keeping all elements “in plane”.
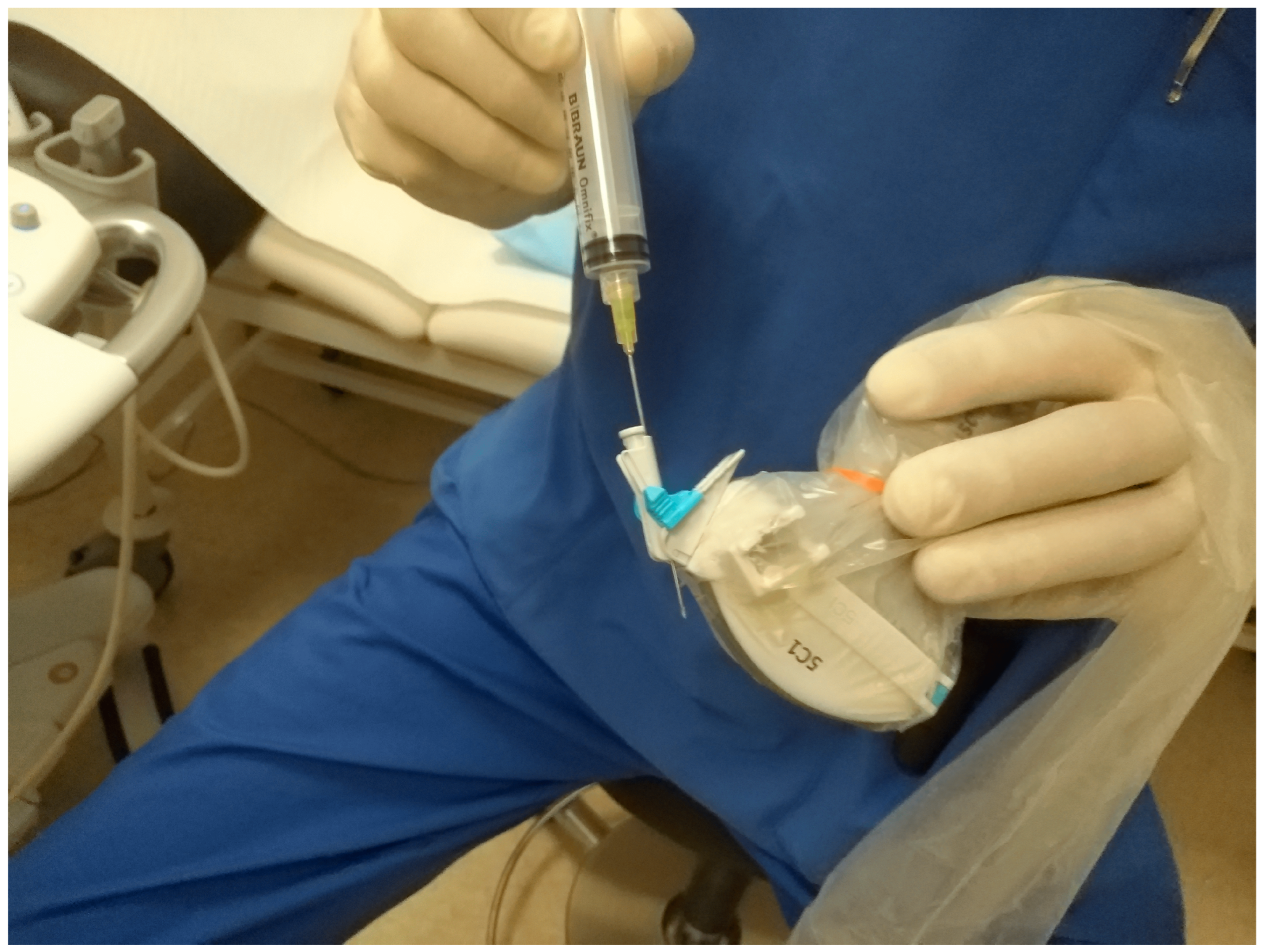
Figure 2. Needle attachment. Up to four given puncture angles can be chosen depending on the US machine manufacturer.
However, the “free hand” technique allows for every puncture angle and is, therefore, preferred by us. The use of colour Doppler will enable the doctor to avoid blood vessels and identify smaller bile ducts (Figure 3a,b).
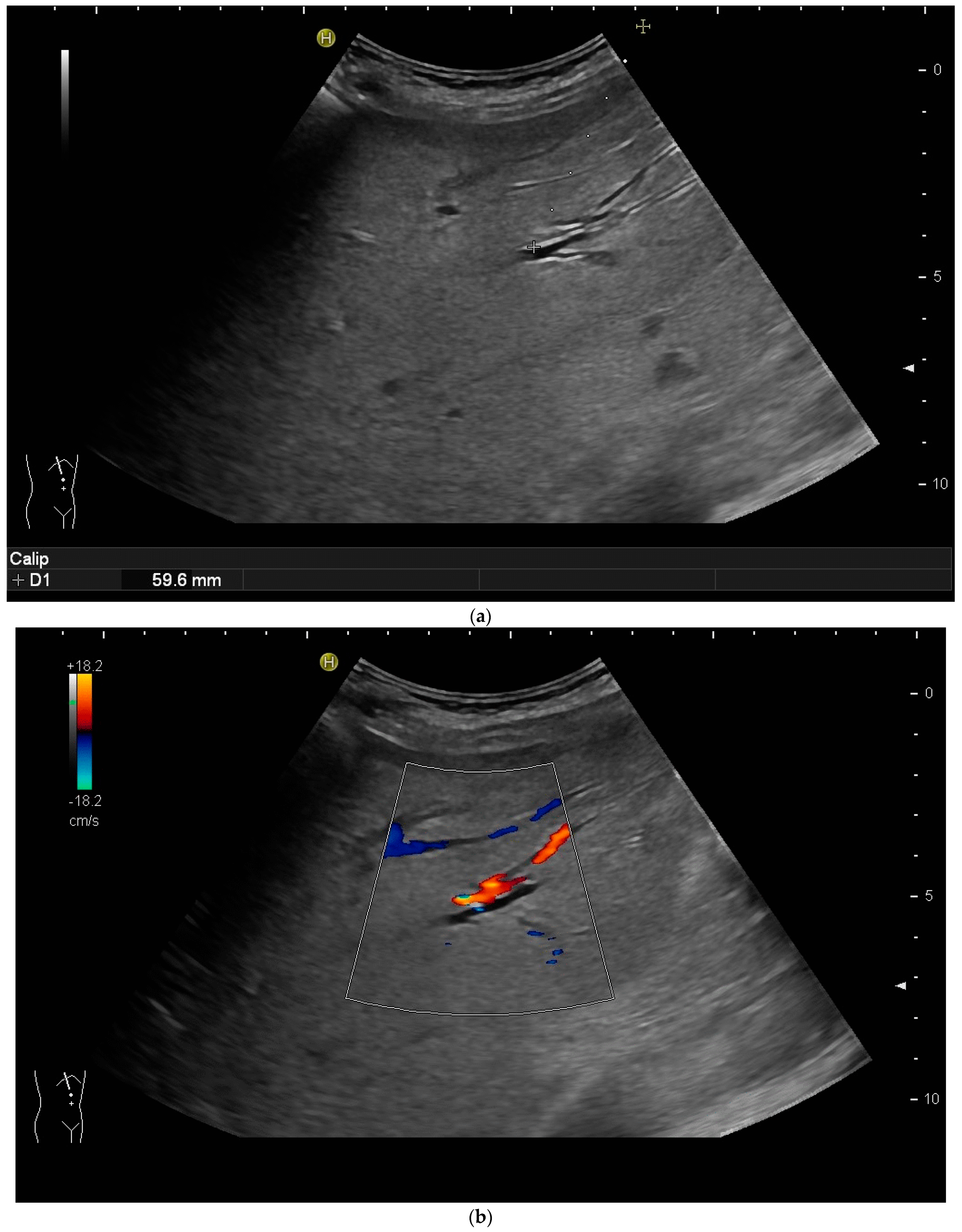
Figure 3. (a) Hypoechoic tubular structures in Segment V are visualised in an intercostal view; (b) Colour Doppler helps to differentiate between bile ducts and blood vessels.
In cases of extrahepatic obstruction, mostly the right liver lobe will be addressed. It is common practice to head for the peripheral branches in Segment V (cf. Figure 3a,b), as from there to the common bile duct, the biliary branches form a harmonic arch, and the forward movement of the guide wire seems unpretentious [3]. However, US guidance allows the puncture of any biliary duct of the right or left liver lobe that can be depicted well (Figure 4a–c).
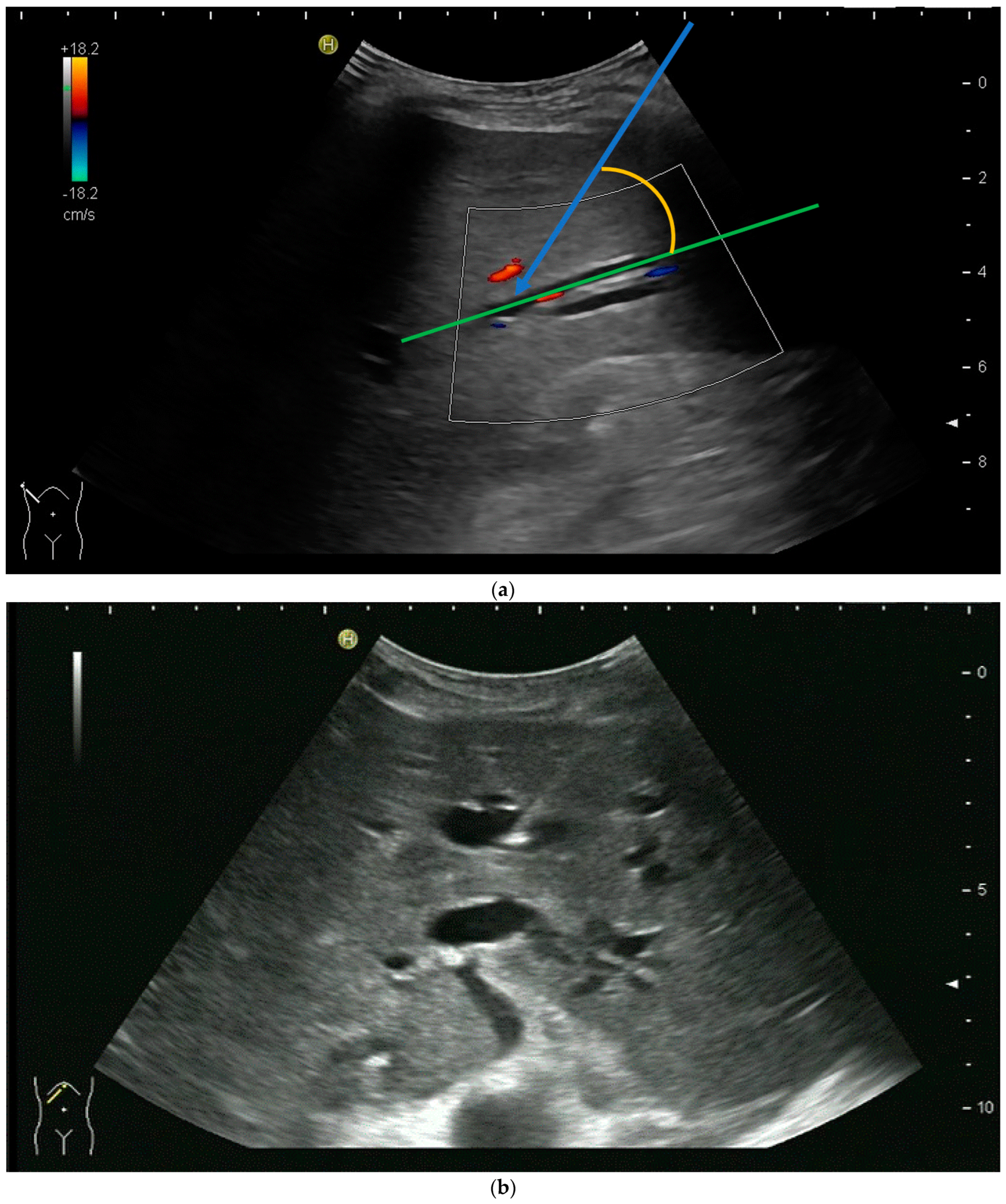
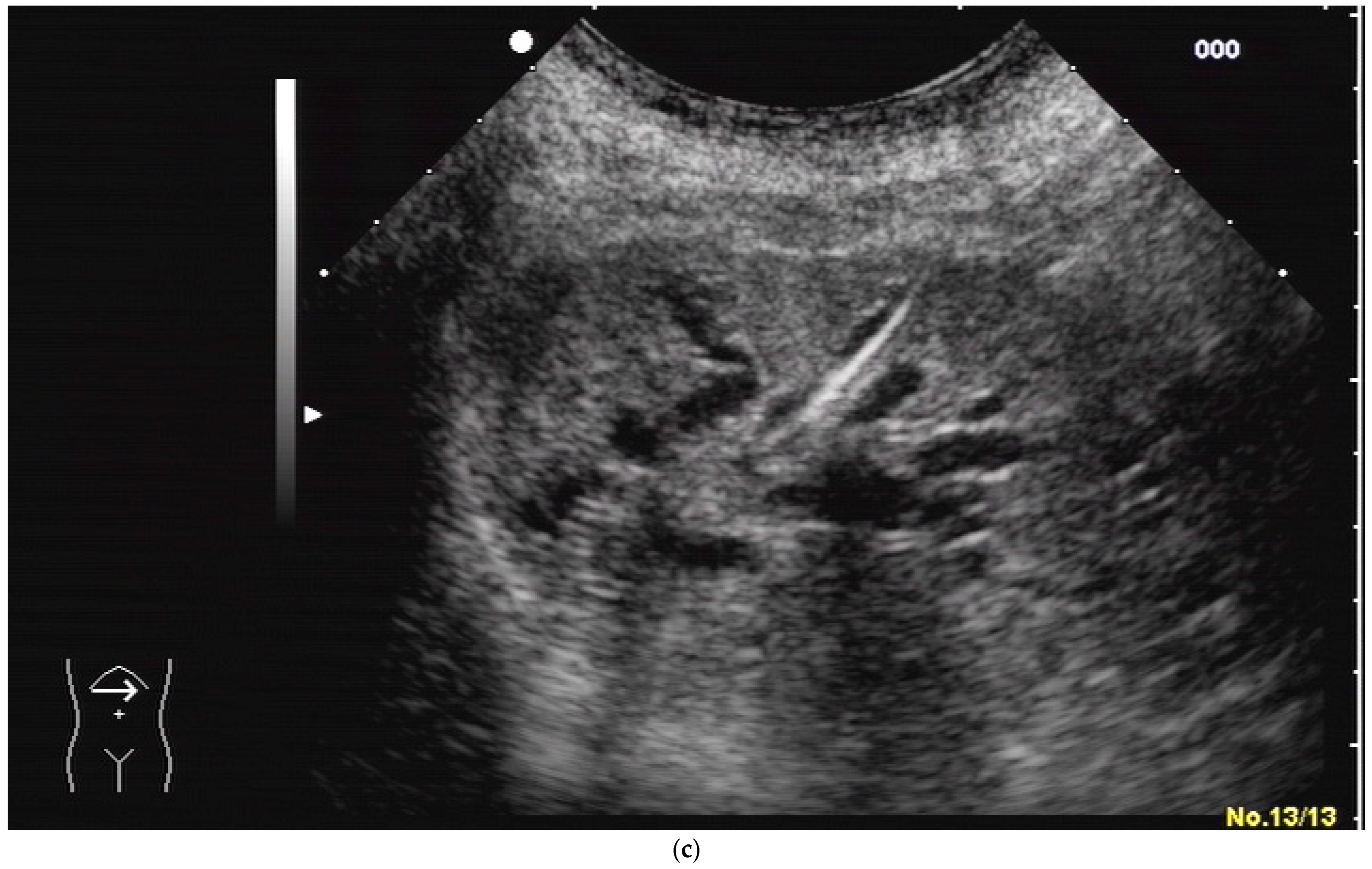
Figure 4. (a) A pointed angle between the needle trajectory and a bile duct of Segment V/VI is given; (b) Puncture of a dilated bile duct in Segment IV at a suitable angle. A guide wire with a bended tip should be used to facilitate the correct advancement; (c) A guide wire is placed in a dilated intrahepatic bile duct in Segment III.
If peripheral bile ducts are not dilated and puncture is difficult, sometimes, targeting the central bile ducts and even the common bile duct close to the hilum are the only options to place drainage. When trying to puncture the common bile duct, it is sensible to enter it as proximal as possible to avoid biliary leakage after drain removal. The needle tract should point towards the distal common bile duct (CBD) to facilitate guide-wire advancement (Figure 5).
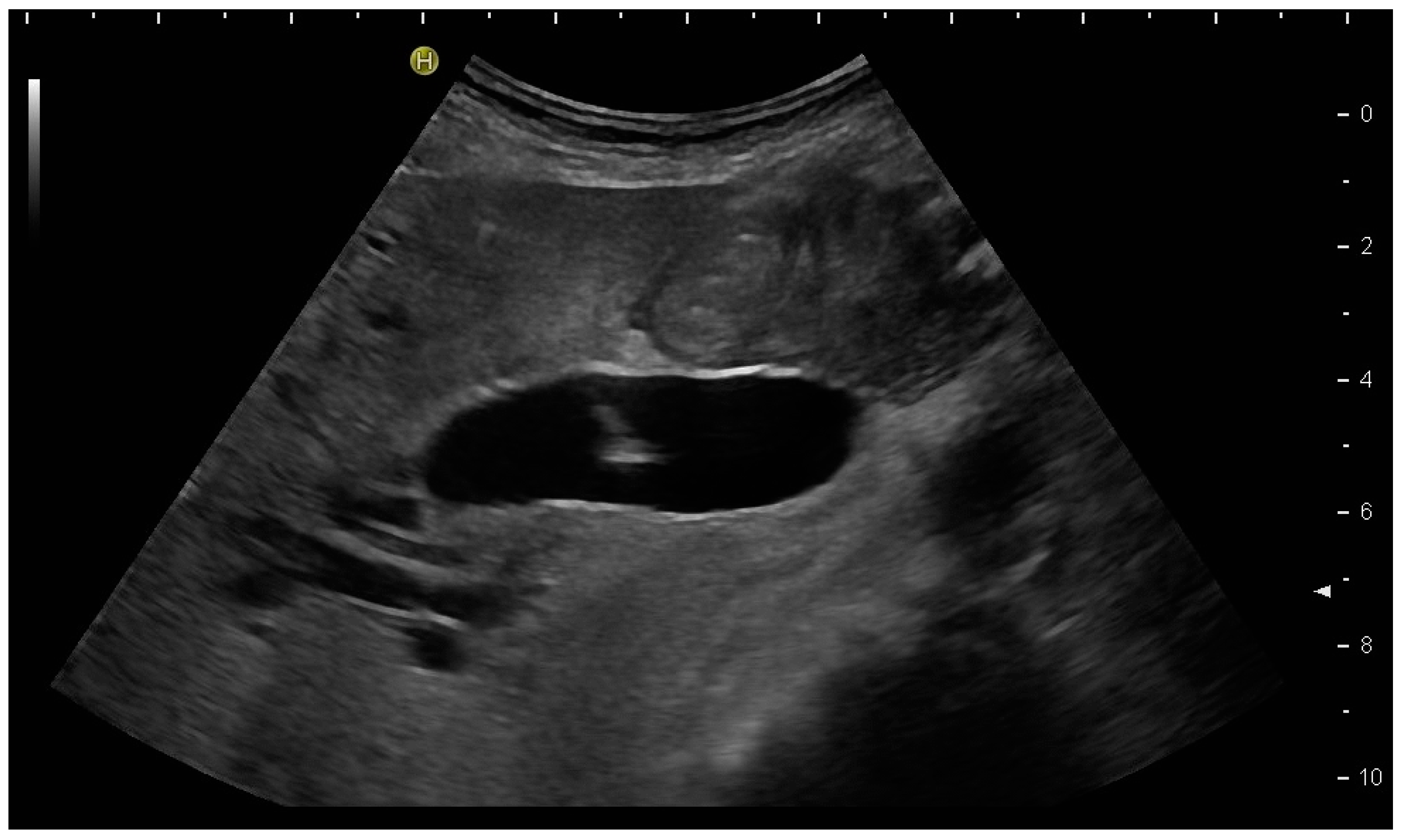
Figure 5. Puncture of the CBD in a patient with pancreatic carcinoma. The tip of the needle is seen in the dilated CBD. Pigtail drainage was placed in the CBD, and ten days later, internal drainage by a self-expanding metal stent was placed using a rendezvous technique (percutaneous transpapillary guide-wire advancement and endoscopic stent placement over the wire).
Usually, a Chiba needle of 21 G is used for the primary puncture. These needles can be depicted quite well in US given that the angle is pointed. Once the targeted bile duct has been accessed, the procedure is continued under fluoroscopic guidance by injecting a small amount of contrast agent to confirm correct needle placement and to visualise the biliary system fluoroscopically (Figure 6).
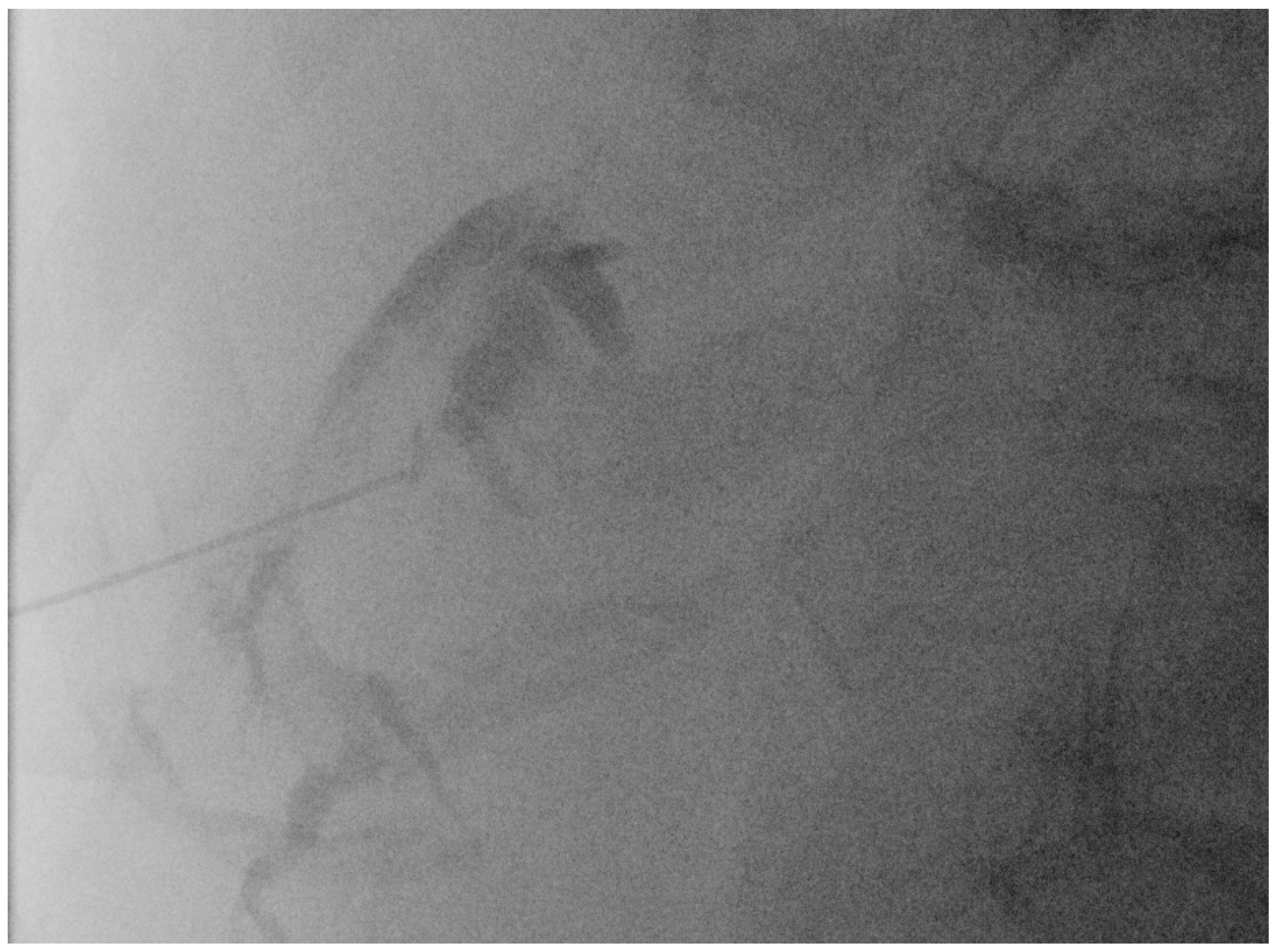
Figure 6. Fluoroscopic confirmation of correct US-guided placement of the 24G needle.
The application of diluted US contrast agents such as SonoVue® can confirm correct needle placement as well (Figure 7) but will worsen guide-wire visibility thereafter.
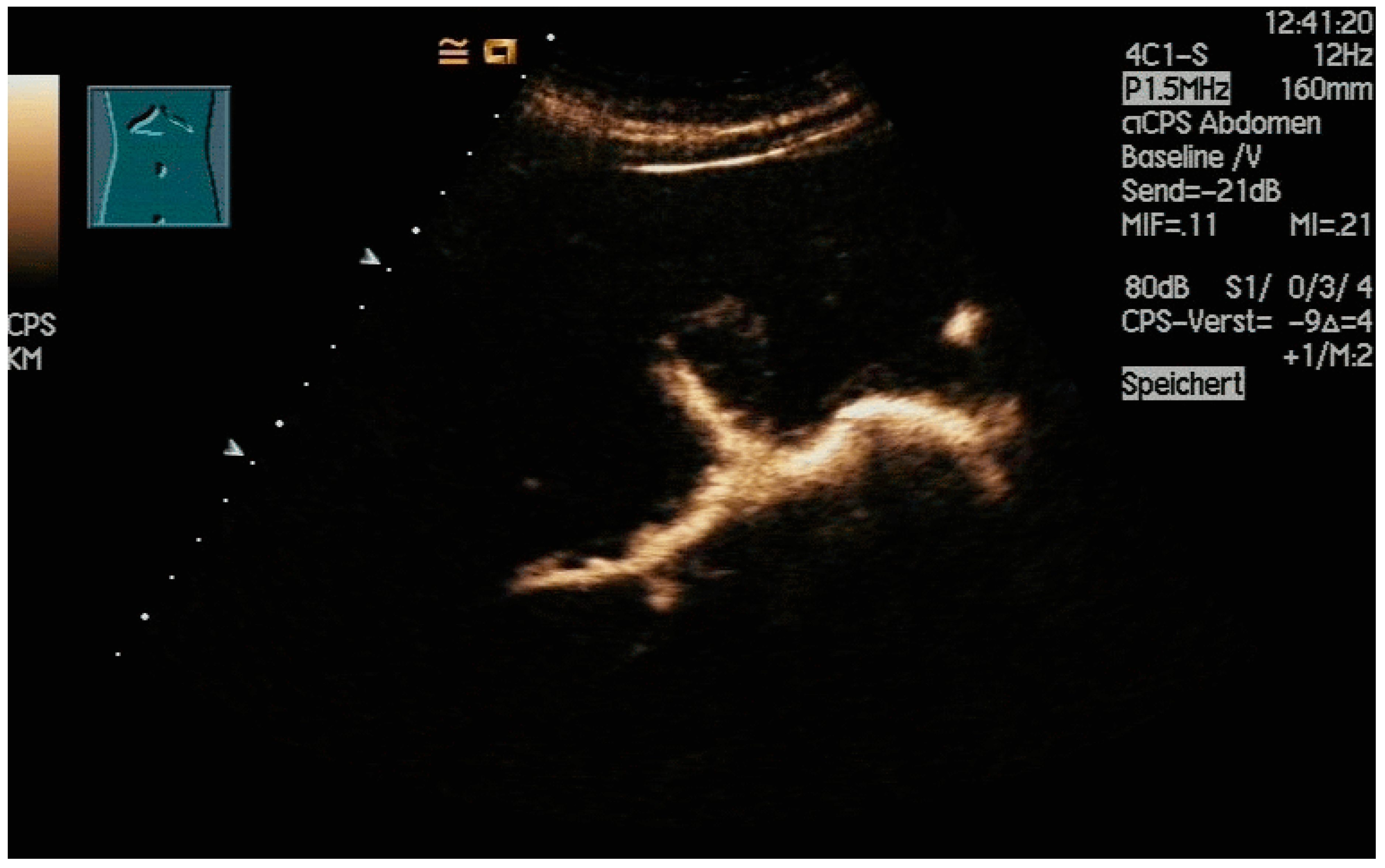
Figure 7. After injection of one drop of SonoVue® diluted in 10 mL sodium chloride 0.9%, the dilated intrahepatic bile ducts are depicted, and correct needle placement is confirmed. However, subsequent monitoring of the guide wires will be hindered.
Then, a thin 0.018” guide wire is placed through the needle into the bile duct. Subsequently, a plastic 5F catheter is inserted over the wire. Thin metal guide wires are clearly visible on the US (Figure 8), but usually, the procedure is continued under fluoroscopic guidance to advance the wire across the stricture into the duodenum.
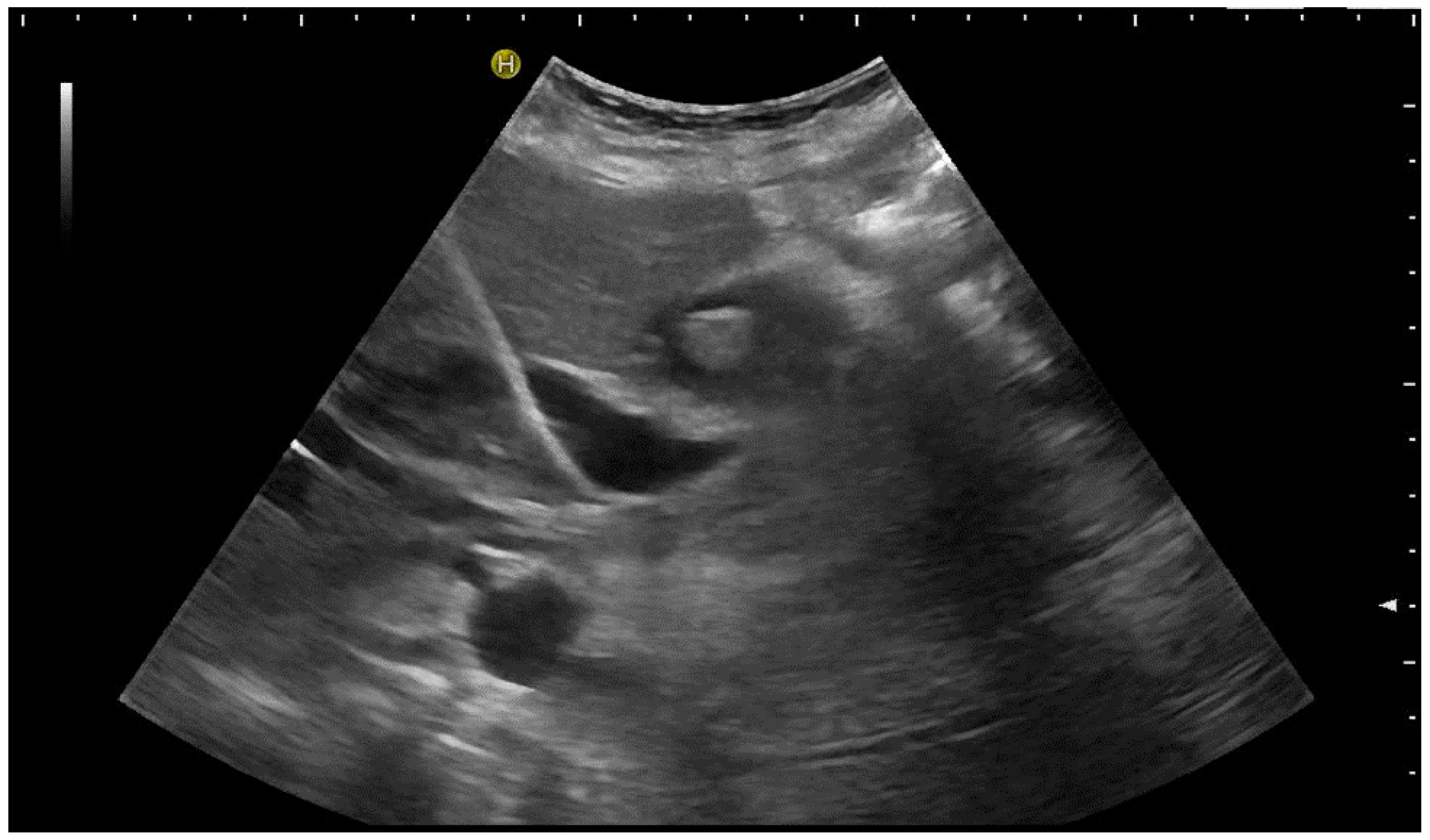
Figure 8. The 0.018” guide wire is very well-depicted by US. The 5F plastic catheter will subsequently be placed; however, there is poor sonographic visibility.
Subsequently, exchanging to larger and more stable 0.035” guide wires allows stepwise bouginage of the tract and the placement of drainage [3][14][41][42]. Ideally, drainage should be placed with side holes above and below the stenosis and the tip in the duodenum for combined extern–intern drainage. If the placement across the stricture into the duodenum fails, external drainage can be placed.
If external drainage is initially planned, it can be placed under US guidance alone; fluoroscopy and cholangiography are not necessary. External drainage has a higher risk of dislocation; therefore, a pigtail catheter should be chosen to reduce this risk. A thread lock that prevents the uncoiling of the pigtail may be helpful, too.
If the bile has been drained for 1–2 days via the external catheter, and the intrahepatic ducts have been decompressed, it is often easier to advance the wire successfully into the duodenum to internalise the drainage.
Special consideration should be given to the distance between the skin and the first side hole of drainage to avoid leakage into the peritoneum and to ensure that the first side hole is above the stricture.
References
- Devane, A.M.; Annam, A.; Brody, L.; Gunn, A.J.; Himes, E.A.; Patel, S.; Tam, A.L.; Dariushnia, S.R. Society of Interventional Radiology Quality Improvement Standards for Percutaneous Cholecystostomy and Percutaneous Transhepatic Biliary Interventions. J. Vasc. Interv. Radiol. 2020, 31, 1849–1856.
- Moll, C.F.; Moura, D.T.H.D.; Ribeiro, I.B.; Proença, I.M.; Monte Junior, E.S.D.; Sánchez-Luna, S.A.; Merchán, M.F.S.; Intriago, J.M.V.; Bernardo, W.M.; Moura, E.G.H.D. Endoscopic Biliary Darinage (EBD) versus Percutaneous Transhepatic Biliary Drainage (PTBD) for biliary drainage in patients with Perihilar Cholangiocarcinoma (PCCA): A systematic review and meta-analysis. Clinics 2023, 78, 100163.
- Cazejust, J.; Pommier, R.; Tavolaro, S. Comment je fais un drainage biliaire percutané? J. D’imagerie Diagn. Interv. 2019, 2, 88–93.
- Nagino, M.; Takada, T.; Kawarada, Y.; Nimura, Y.; Yamashita, Y.; Tsuyuguchi, T.; Wada, K.; Mayumi, T.; Yoshida, M.; Miura, F.; et al. Methods and timing of biliary drainage for acute cholangitis: Tokyo Guidelines. J. Hepato-Biliary-Pancreat. Surg. 2007, 14, 68–77.
- Duan, F.; Cui, L.; Bai, Y.; Li, X.; Yan, J.; Liu, X. Comparison of efficacy and complications of endoscopic and percutaneous biliary drainage in malignant obstructive jaundice: A systematic review and meta-analysis. Cancer Imaging 2017, 17, 27.
- Liu, J.-G.; Wu, J.; Wang, J.; Shu, G.-M.; Wang, Y.-J.; Lou, C.; Zhang, J.; Du, Z. Endoscopic Biliary Drainage Versus Percutaneous Transhepatic Biliary Drainage in Patients with Resectable Hilar Cholangiocarcinoma: A Systematic Review and Meta-Analysis. J. Laparoendosc. Adv. Surg. Tech. 2018, 28, 1053–1060.
- Dumonceau, J.M.; Tringali, A.; Papanikolaou, I.S.; Blero, D.; Mangiavillano, B.; Schmidt, A.; Vanbiervliet, G.; Costamagna, G.; Devière, J.; García-Cano, J.; et al. Endoscopic biliary stenting: Indications, choice of stents, and results: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline—Updated October 2017. Endoscopy 2018, 50, 910–930.
- Adler, D.; Dhindsa, B.; Mashiana, H.; Dhaliwal, A.; Mohan, B.; Jayaraj, M.; Sayles, H.; Singh, S.; Ohning, G.; Bhat, I. EUS-guided biliary drainage: A systematic review and meta-analysis. Endosc. Ultrasound 2020, 9, 101–109.
- Sharaiha, R.Z.; Khan, M.A.; Kamal, F.; Tyberg, A.; Tombazzi, C.R.; Ali, B.; Kahaleh, M. Efficacy and safety of EUS-guided biliary drainage in comparison with percutaneous biliary drainage when ERCP fails: A systematic review and meta-analysis. Gastrointest. Endosc. 2017, 85, 904–914.
- Elmunzer, B.J.; Maranki, J.L.; Gómez, V.; Tavakkoli, A.; Sauer, B.G.; Limketkai, B.N.; Brennan, E.A.; Attridge, E.M.; Brigham, T.J.; Wang, A.Y. ACG Clinical Guideline: Diagnosis and Management of Biliary Strictures. Am. J. Gastroenterol. 2023, 118, 405–426.
- Yee, A.C.; Ho, C.S. Percutaneous transhepatic biliary drainage: A review. Crit. Rev. Diagn. Imaging 1990, 30, 247–279.
- Weber, A.; Rosca, B.; Neu, B.; Rösch, T.; Frimberger, E.; Born, P.; Schmid, R.; Prinz, C. Long-term follow-up of percutaneous transhepatic biliary drainage (PTBD) in patients with benign bilioenterostomy stricture. Endoscopy 2009, 41, 323–328.
- Fairchild, A.H.; Hohenwalter, E.J.; Gipson, M.G.; Al-Refaie, W.B.; Braun, A.R.; Cash, B.D.; Kim, C.Y.; Pinchot, J.W.; Scheidt, M.J.; Schramm, K.; et al. ACR Appropriateness Criteria® Radiologic Management of Biliary Obstruction. J. Am. Coll. Radiol. 2019, 16, S196–S213.
- Hafezi-Nejad, N.; Liddell, R.P. Percutaneous Biliary Interventions: Clinical Indications, Comparative Effectiveness, Technical Considerations, Complications, and Outcomes. Gastrointest. Endosc. Clin. 2022, 32, 493–505.
- Morettin, L.B.; Dodd, G.D. Percutaneous transhepatic cholangiography. Am. J. Dig. Dis. 1972, 17, 831–845.
- Wimmer, B.; Hauenstein, K.H.; Kauffmann, G.; Friedburg, H. Sonographische perkutane Gallengangsdrainage. RoFo 1981, 135, 466–470.
- Makuuchi, M.; Bandai, Y.; Ito, T.; Watanabe, G.; Wada, T.; Abe, H.; Muroi, T. Ultrasonically guided percutaneous transhepatic bile drainage: A single-step procedure without cholangiography. Radiology 1980, 136, 165–169.
- Makuuchi, M.; Yamazaki, S.; Hasegawa, H.; Bandai, Y.; Ito, T.; Watanabe, G. Ultrasonically guided cholangiography and bile drainage. Ultrasound Med. Biol. 1984, 10, 617–623.
- Das, K.; Kochhar, R.; Mehta, S.K.; Suri, S. A modified technique of ultrasonically guided percutaneous transhepatic biliary drainage. Surg. Endosc. 1989, 3, 191–194.
- Lee, W.; Kim, G.C.; Kim, J.Y.; Baik, S.K.; Lee, H.J.; Kim, H.J.; Ryeom, H.K. Ultrasound and fluoroscopy guided percutaneous transhepatic biliary drainage in patients with nondilated bile ducts. Abdom. Imaging 2008, 33, 555–559.
- Ilikan, G.; AKMANGİT, İ. Percutaneous Transhepatic Cholangiography, Percutaneous Biliary Drainage and Metallic Endoprotesis Applications in Malign Biliary Obstructions. J. Contemp. Med. 2020, 11, 97–103.
- Schmitz, D.; Grosse, A.; Hallscheidt, P.; Roseneck, A.; Niemeyer, J.; Rudi, J. Color Doppler ultrasound-guided PTBD with and without metal stent implantation by endoscopic control: Prospective success and early adverse event rates. Z. Gastroenterol. 2015, 53, 1255–1260.
- Giurazza, F.; Italian College of Interventional Radiology (ICIR) Rising Stars Group; Corvino, F.; Contegiacomo, A.; Marra, P.; Lucarelli, N.M.; Calandri, M.; Silvestre, M.; Corvino, A.; Lucatelli, P.; et al. Safety and effectiveness of ultrasound-guided percutaneous transhepatic biliary drainage: A multicenter experience. J. Ultrasound 2019, 22, 437–445.
- Prasad, U.; Kumar, D.; Kumar, A.; Singh, R.K.; Suman, S.K.; Kumari, P. Ultrasound-Guided Percutaneous Transhepatic Biliary Drainage Outcome at Tertiary Care Centre of North India. Int. J. Sci. Study 2021, 9, 93–99.
- Chandel, K.; Singh, J.; Tripathy, T.P.; Patel, R. Is Ultrasound-guided Bedside Percutaneous Transhepatic Biliary Drainage Safe and Feasible in Critically Ill Patients with Severe Cholangitis? A Preliminary Single-center Experience. Indian J. Crit. Care Med. 2023, 27, 16–21.
- Ignee, A.; Cui, X.; Schuessler, G.; Dietrich, C.F. Percutaneous transhepatic cholangiography and drainage using extravascular contrast enhanced ultrasound. Z. Gastroenterol. 2015, 53, 385–390.
- Müller, T.; Blank, W.; Leitlein, J.; Kubicka, S.; Heinzmann, A. Endocavitary contrast-enhanced ultrasound: A technique whose time has come? J. Clin. Ultrasound 2015, 43, 71–80.
- Xu, E.-J.; Zheng, R.-Q.; Su, Z.-Z.; Li, K.; Ren, J.; Guo, H.-Y. Intra-biliary contrast-enhanced ultrasound for evaluating biliary obstruction during percutaneous transhepatic biliary drainage: A preliminary study. Eur. J. Radiol. 2012, 81, 3846–3850.
- Miyazaki, M.; Shibuya, K.; Tokue, H.; Tsushima, Y. Percutaneous transhepatic biliary drainage assisted by real-time virtual sonography: A retrospective study. BMC Gastroenterol. 2013, 13, 127.
- Wagner, A.; Mayr, C.; Kiesslich, T.; Berr, F.; Friesenbichler, P.; Wolkersdörfer, G.W. Reduced complication rates of percutaneous transhepatic biliary drainage with ultrasound guidance. J. Clin. Ultrasound 2017, 45, 400–407.
- Park, S.E.; Nam, I.C.; Baek, H.J.; Ryu, K.H.; Lim, S.G.; Won, J.H.; Kim, D.R. Effectiveness of ultrasound-guided percutaneous transhepatic biliary drainage to reduce radiation exposure: A single-center experience. PLoS ONE 2023, 17, e0277272.
- Kozlov, A.V.; A Polikarpov, A.; Oleshchuk, N.V.; Tarazov, P.G. Comparative assessment of percutaneous transhepatic cholangiodrainage under roentgenoscopy and ultrasound guidance. Vestn. Rentgenol. Radiol. 2002, 4, 30–33.
- Nennstiel, S.; Treiber, M.; Faber, A.; Haller, B.; von Delius, S.; Schmid, R.M.; Neu, B. Comparison of Ultrasound and Fluoroscopically Guided Percutaneous Transhepatic Biliary Drainage. Dig. Dis. 2018, 37, 77–86.
- Lee, Y.-T.; Yen, K.-C.; Liang, P.-C.; Wu, C.-H. Procedure-related risk factors for bleeding after percutaneous transhepatic biliary drainage: A systematic review and meta-analysis. J. Formos. Med. Assoc. 2022, 121, 1680–1688.
- Müller, T.; Martiny, H.; Merz, E.; Döffert, J.; Wüstner, M.; Lessel, W.; Heynemann, H.; Enzmann, T.; Dudwiesus, H.; Nuernberg, D.; et al. DEGUM Recommendations on Infection Prevention in Ultrasound and Endoscopic Ultrasound. Ultraschall Med. 2018, 39, 284–303.
- Nyhsen, C.M.; Humphreys, H.; Koerner, R.J.; Grenier, N.; Brady, A.; Sidhu, P.; Nicolau, C.; Mostbeck, G.; D’onofrio, M.; Gangi, A.; et al. Infection prevention and control in ultrasound—Best practice recommendations from the European Society of Radiology Ultrasound Working Group. Insights Imaging 2017, 8, 523–535.
- Hayashi, N.; Sakai, T.; Kitagawa, M.; Kimoto, T.; Inagaki, R.; Ishii, Y. US-guided left-sided biliary drainage: Nine-year experience. Radiology 1997, 204, 119–122.
- Gupta, P.; Maralakunte, M.; Rathee, S.; Samanta, J.; Sharma, V.; Mandavdhare, H.; Sinha, S.K.; Dutta, U.; Kochhar, R. Percutaneous transhepatic biliary drainage in patients at higher risk for adverse events: Experience from a tertiary care referral center. Abdom. Imaging 2020, 45, 2547–2553.
- Kim, Y.H.; Cha, S.J. US-guided Percutaneous Transhepatic Biliary Drainage: Comparative Study of Right-sided and Left-sided Approach. J. Korean Radiol. Soc. 2002, 46, 115–118.
- Filipović, A.N.; Mašulović, D.; Zakošek, M.; Filipović, T.; Galun, D. Total Fluoroscopy Time Reduction During Ultrasound- and Fluoroscopy-Guided Percutaneous Transhepatic Biliary Drainage Procedure: Importance of Adjusting the Puncture Angle. J. Pharmacol. Exp. Ther. 2021, 27, e933889-1–e933889-7.
- Zorger, N.; Feuerbach, S. Technik der perkutanen transhepatischen Cholangio-Drainage (PTCD). J. Gastroenterol. Hepatol. Erkrank. 2010, 8, 21–26.
- Covey, A.M.; Brown, K.T. Percutaneous Transhepatic Biliary Drainage. Tech. Vasc. Interv. Radiol. 2008, 11, 14–20.
More
Information
Subjects:
Emergency Medicine
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
889
Revisions:
2 times
(View History)
Update Date:
28 Feb 2024
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




