Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Mascarenhas, C.; Sousa, A.C.A.; Rato, L. Pharmaceuticals with Obesogen Action Impact Male Fertility. Encyclopedia. Available online: https://encyclopedia.pub/entry/55452 (accessed on 02 March 2026).
Mascarenhas C, Sousa ACA, Rato L. Pharmaceuticals with Obesogen Action Impact Male Fertility. Encyclopedia. Available at: https://encyclopedia.pub/entry/55452. Accessed March 02, 2026.
Mascarenhas, Caio, Ana C. A. Sousa, Luís Rato. "Pharmaceuticals with Obesogen Action Impact Male Fertility" Encyclopedia, https://encyclopedia.pub/entry/55452 (accessed March 02, 2026).
Mascarenhas, C., Sousa, A.C.A., & Rato, L. (2024, February 26). Pharmaceuticals with Obesogen Action Impact Male Fertility. In Encyclopedia. https://encyclopedia.pub/entry/55452
Mascarenhas, Caio, et al. "Pharmaceuticals with Obesogen Action Impact Male Fertility." Encyclopedia. Web. 26 February, 2024.
Copy Citation
Obesogens have been identified as a significant factor associated with increasing obesity rates, particularly in developed countries. Substances with obesogenic traits are prevalent in consumer products, including certain pharmaceuticals. Specific classes of pharmaceuticals have been recognized for their ability to induce weight gain, often accompanied by hormonal alterations that can adversely impact male fertility.
antidiabetics
antihypertensives
endocrine disruptors
male fertility
obesogens
Pharmaceuticals
1. Introduction
The regulation of male fertility is a very complex process and can be interrupted by numerous factors such as life style, drug consumption, and exposure to environmental contaminants that present endocrine-disrupting and obesogenic properties [1]. In order to understand the impact of such factors, several endpoints need to be evaluated. While all animals are monitored by body weight and fertility indices, there are specifically relevant assessment points that should also be considered, including the macroscopic examination and morphology of reproductive organs, observation of development effects, and measurement of spermatozoan effects. Weight and histopathological analyses of the testicles, epididymis, and accessory sex glands, including the prostate and seminal vesicles, should be conducted because these sex glands are dependent on androgens, and these hormones reflect changes in the endocrine state of the animal or testicular function [1][2]. Additionally, as the normal physical development may also be affected by the exposure to obesogens, testicular descent, anogenital distance, and the external genitalia structure need to be evaluated. Finally, the evaluation of the number of spermatozoa, morphology, and motility is of paramount importance as the number of spermatozoa is derived from spermatid head counts in the testicle and epididymis [3][4][5][6]. Furthermore, the comprehension of the impacts of the exposure to different pharmaceutical agents is further conditioned by a latency period, as the side effects of the drugs may be observed even after the discontinuation of treatment, being necessary for 1 to 3 months for the parameters to be restored. Some studies have shown that obesogens can alter endocrine activity in various ways, affecting androgen production. The hypothalamus–pituitary–gonad axis (HPG) is fundamental for male sexual maturity and fertility regulation. The hypothalamus secretes the gonadotrophine-refining hormone (GnRH), which causes an increase in the nocturnal secretion of pulsatile gonadotrophy (luteinizing hormone (LH) and follicle-stimulating hormone (FSH)) by the anterior pituitary [1][7]. In humans, a neonatal testosterone spike during the first 4 months of life leads to testosterone levels that resemble those of a healthy adult man [8]. At 6 months of age, testosterone levels decrease to almost negligible levels and remain low until puberty, at which time sexual characteristics develop. In adult men, the pulsatile secretion of gonadotrophin occurs approximately every 90 min; the frequency with which this occurs is an important factor in the normal gonadal response [9]. When the pulse frequency of gonadotrophin reaches a critical level, secondary sexual characteristics begin to form; this marks the onset of puberty [7]. While FSH is not used until sperm maturation, LH is released during sleep along with pulsatile GnRH, causing gonadal stimulation and the induction of the hyperplasia of Leydig cells, responsible for testosterone production [10]. Any therapy that affects testicular endocrine function has as a direct consequence of the deregulation of spermatogenesis, compromising the viability of germ cells or even the integrity of Sertoli cells. Sertoli cells play a supporting role in the survival and differentiation of germ cells, as they not only provide physical support, but also ensure the “nutrition” of the germ line [11][12]. Another target of the endocrine disruption of the testicles is the production of testosterone by Leydig cells or even the disturbance of the hypothalamus–pituitary axis, which results in deficient testosterone production. Treatments with certain classes of medications (antidiabetic, antihypertensive, antidepressant, antipsychotic, and antiepileptic) can cause endocrine disorders, which end up directly interfering with the male reproductive tract and all molecular mechanisms responsible for the physiological maintenance of male fertility (see Figure 1).
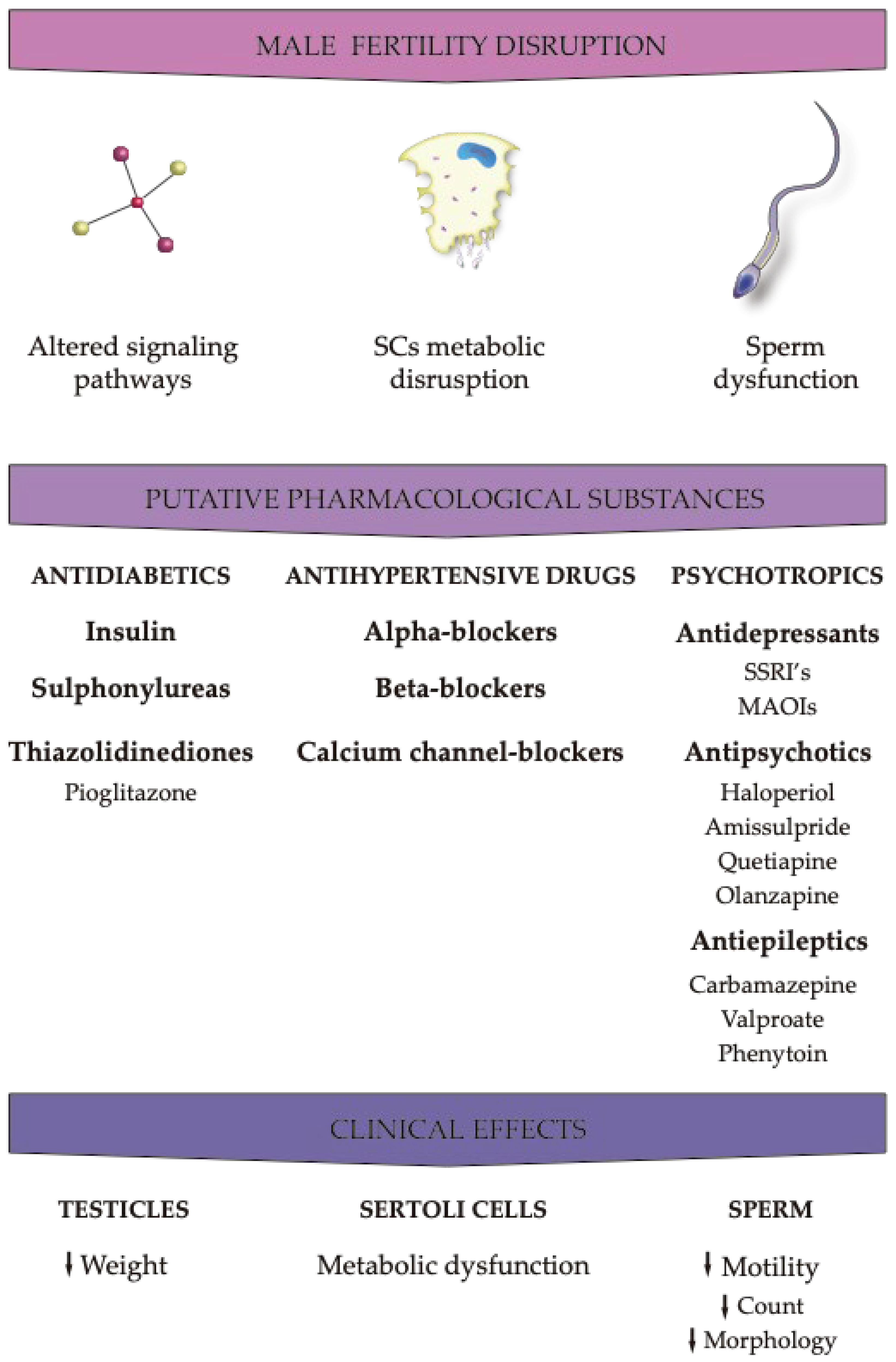
Figure 1. Effects of the different pharmacological agents on male fertility parameters. The effects of pharmaceuticals with obesogenic action are exerted at the peripheral level by disrupting molecular pathways that regulate male reproductive physiology. However, in addition to peripheral effects, local effects, particularly at the cellular level, have implications that can be equally or more severe than the former. Due to their relevance in the formation of germ cells, Sertoli cells are one of the main targets, as they provide physical and nutritional support to germ cells. Any action leading to the dysfunction of these cells compromises the production or the development of sperm in functionally competent cells. Down arrows: decreased.
2. Antidiabetics
Although certain drugs of this class have obesogenic characteristics, such as insulin, SU, and some TZDs, pioglitazone and metformin (biguanide) are the most notorious ones. These drugs are used in the treatment of T2DM, being suitable for young people and men of reproductive age. Pioglitazone is a potent synthetic agonist of PPARg-activated receptors [13]. The activation of these receptors leads to the increased transcription of genes related to glucose metabolism. Pioglitazone is available to make combinations with other antidiabetics such as metformin [14]. It differs (heterodimerizes) from retinoid receptor X and binds to responsive nuclear elements, thus modulating the transcription of genes that play a role in glucose and lipid metabolism [15]. An adverse effect that this class has is fluid retention, which makes TZDs contraindicated in individuals with heart failure, which is one of the leading causes of death in individuals with T2DM [16]. In a recent study, it was observed that pioglitazone at the dose of (10 μM) increases lactate production in in vitro cultures of human Sertoli cells without causing morphological changes or considerable metabolic changes (Table 1). This result is relevant since lactate is a survival factor of some germ cells and, thus, pioglitazone is a positive factor in testicular metabolic reprogramming [17].
3. Antihypertensive Drugs
The mechanisms by which these treatments affect sexual function are yet to be properly clarified, with limited studies providing data on the interactions between this class of drugs and sexual dysfunctions. Therefore, it is still difficult to show the impact they may have on the reproductive tract. Some studies suggest that hypertensive erectile dysfunction may be the result of reduced penile pressure, associated with decreased systemic pressure reduced by the antihypertensives themselves [18][19][20]. Other studies have shown that antihypertensives with central action stimulate α2-adrenergic presynapttic receptors, causing a reduction in the central sympathetic tone. The increase in the sympathetic tone leads to short-blooded tacardia; consequently, centrally activated antihypertensives would be a good choice for the treatment of hypertension. However, they can generate changes in ejaculatory function, as a sign of hormonal changes [18][21].
Other drugs, including alpha blockers and calcium channel blockers, do not cause erectile dysfunction but may generate ejaculatory disorders due to spongy bulb muscle contractions [12]. Angiotensin-converting-enzyme inhibitors and sartans, on the other hand, do not alter erectile function. In fact, angiotensin II is an important mediator of penile tumescence (erectile dysfunction). Regarding the effects of drugs that improve endothelium function in erection, it has been demonstrated that angiotensin II antagonists are very promising [22]. In fact, angiotensin II antagonists are considered a good option for the treatment of hypertension in sexually active individuals, since they improve endothelial function in penile erection [18][23][24][25][26]. Some studies on the implication of antihypertensive drugs in erectile dysfunction showed that sartans were not associated with the development of sexual dysfunction and that they might be a viable therapeutic treatment option to prevent or correct erectile dysfunctions in patients with hypertension [18][19][23][24][27][28][29]. The administration of drugs with antihypertensive action, such as calcium channel blockers, compromise fertility, particularly by reducing the viability and motility of spermatozoa (Table 1). The alteration of these clinical parameters prevents the fertilization process because it prevents the sperm and oocyte from interacting, resulting from the transmembrane movement of the calcium modifier, as described in vitro in [29][30][31][32]. Although these side effects in hypertensive individuals do not constitute a motive for therapy discontinuation, it is important to consider the beneficial effects that antihypertensives have in relation to cardiovascular problems.
4. Psychotropics
4.1. Antidepressants
Selective serotonin reuptake inhibitors (SSRIs) are the first-line treatment for depression, and tricyclic antidepressants play the role of inhibiting the recapture of catecholamines at the central level. Tricyclic antidepressants and SSRIs are responsible for hyperprolactinemia, which will inhibit the hypothalamus. If hypogonadism is observed, these drugs may cause adverse effects on male fertility as described below [28][29][33][34]. SSRIs are responsible for the increase in serotonin neurotransmission, thus causing an inhibition of male sexual behavior. Men who are under this type of therapy have a loss of libido and anorgasmia during prophylaxis. Delayed ejaculation, or even anejaculation, have also been observed in a few weeks after the start of treatment. Treatment with tricyclic antidepressants is associated with delayed ejaculation/anejaculation [21][24][27][28][29][35][36][37]. At the clinical level, SSRIs alter sperm count and motility (Table 1). However, there is some controversy in the literature about the adverse effects on reproductive clinical parameters. Antidepressants can also alter sperm quality through a mechanism that affects its transport, since drugs belonging to this class act at the level of the central nervous system and affect the ejaculation process [34][38][39][40]. Monoamine oxidase inhibitors (MAOIs) are also prescribed for the treatment of depression, but with a lower frequency and priority, and they rarely generate any erectile disorders, as they are less associated with hyperprolactinemia [33]. Depression is characterized as a chronic condition, and in the event of adverse effects such as changing sexual parameters, in the therapy based and MRI or MAOI, discontinuation of treatment is a very viable option. In relation to other antidepressants such as bupropion, mirtazapine, and buspirone, it was found that they do not cause considerable changes in male reproductive health [21][27][28][29][35][37][41][42][43].
4.2. Antipsychotics
Like tricyclic antidepressants and SSIss, “typical” neuroleptics (phenothiazides) are responsible for hyperprolactinemia, the most common abnormality of the hypothalamic-hypothesis axis, caused by exaggerated production and prolactin (PRL) due to the central dopamine secretion block. As a result, one of the most relevant adverse effects are changes in spermatogenesis and the consequent decrease in sperm quality [29][33][44]. The “typical” neuroleptics can also affect sexual activity, e.g., through difficulty in reaching orgasm even with sexual stimulation (anorgasmia), decreased libido, and disorders of the reaction. Dysfunctions that are observed during treatment may also result from an anticholinergic effect induced by the antipsychotics of the β-adrenergic transmission block [12]. As psychotic conditions are often difficult to interpret, it is difficult to tell whether sexual disorders come from chronic disease or its treatment. If any sexual dysfunction appears during treatment with typical neuroleptics such as haloperidol or amissulpride, it may be possible to switch to a treatment with atypical neuroleptics such as quetiapine, olanzapine, or clozapine, as these have an affinity for 5-HT2 receptors and also for dopamine D2 receptors, facilitating sexual behavior by causing fewer side effects [21][27][29][35][45].
4.3. Antiepileptics
Sexual dysfunction in individuals with epileptic conditions is due to several causes and may result from the pathophysiology of the disease and/or treatment with associated anticonvulsants. It is extremely difficult to distinguish the cause of these changes, as epileptic men usually rarely remain without proper treatment, which, therefore, makes it difficult to determine whether the changes are a result of epilepsy or the interaction of the drugs used in the treatment. Studies conducted in animal models have shown that valproate administration is responsible for reducing testicular weight in animals [31][46][47]. Valproate does not increase SHGH levels but increases the level of GABA in the central nervous system, thus modifying the production of GnRH. This drug may also be responsible for increased peripheral levels of androgens, and a possible reduction of LH [47][48][49][50][51]. Inducers of liver enzymes such as carbamazepine and phenytoin increase the synthesis of sex-hormone-binding globulin, the protein involved in testosterone transport, but reduce free levels of androgens [52]. On the clinical level, antiepileptics are believed to have a significant impact on spermatic parameters, and although the underlying molecular pathways are still unclear it is thought that it may be due to the interaction between pharmacological action and the molecular mechanisms underlying pathophysiology. Carbamazepine, valproate, and phenytoin reduce sperm motility by interfering with the sperm membrane, as valproate reduces the L-carnitine/T-carnitine ratio (Table 1). Similarly, carbamazepine is believed to be directly related to germ cells, inducing a greater number of necrotic germ cells in the lumen of seminiferous tubules. Thus, it is suspected that valproate is responsible for the reduction in the testicular weight in animals, indicating that the drug can be harmful not only in the level of spermatogenesis, but also in the degradation of testicular somatic cells, such as Sertoli cells [31][46][47][53][54].
Table 1. The effects of pharmaceuticals with obesogen action in reproductive cells, mainly in Sertoli cells and sperm.
| Types of Pharmaceuticals | Samples/Subjects | Outcomes | References |
|---|---|---|---|
| Antidiabetics | |||
| TZDs | |||
| Pioglitazone | Human Sertoli cells | ↓ lactate production | [17] |
| Antihypertensives | |||
| Alpha Blockers Tamsulosin Alfuzosin |
Human (Clinical trial) | Alterations in semen | [55][56] |
| Calcium Channel Blockers Nifedipine Amlodipine Verapamil Diltiazem |
Human (Clinical trial) | Reduced fertilizing ability of spermatozoa (not under in vivo conditions) | [30][31][32] |
| Amlodipine | Human | ↓ Sperm viability ↓ Sperm motility |
[12][29][30][31][32] [30][31][32] |
| Antidepressants | |||
| Tricyclic (Imipramine) | Human | ↓ Sperm motility | [31][34][40] |
| SSRI | [31][34][40] [31][34][38] [31][46][49] |
||
| Fluoxetine | Human | ↓ Sperm morphology ↓ Sperm count |
|
| Paroxetine | |||
| Sertraline | |||
| Fluvoxamine | |||
| MAOIs | |||
| Bupropion | Human | No effects observed | [21][27][28][35][41][42][43] |
| Mirtazapine | |||
| Buspirone | |||
| Mocoblemide | Human | ↓ Sperm motility under in vitro conditions | [34] |
| Antiephyletics | |||
| Carbamazepine | Human | ↓ Sperm motility ↓ Sperm count ↓ Sperm morphology |
[12] [46][47][50][57] [31][46][49] [46][47][50][57] |
| Phenytoin | |||
| Valproate | |||
| Oxcarbazepine | |||
| Phenobarbital | |||
| Lithium | Human | ↓ Sperm motility | [58] |
| ↓ Sperm count | |||
| ↓ Sperm morphology |
Legend: MAOIs: Monoamine oxidase inhibitors; SSRI: selective serotonin reuptake inhibitors; TZDs: thiazolidinediones. Down arrows: decreased.
References
- Campion, S.; Catlin, N.; Heger, N.; McDonnell, E.V.; Pacheco, S.E.; Saffarini, C.; Sandrof, M.A.; Boekelheide, K. Male reprotoxicity and endocrine disruption. Mol. Clin. Environ. Toxicol. 2012, 315–360.
- Gore, A.C.; Chappell, V.A.; Fenton, S.E.; Flaws, J.A.; Nadal, A.; Prins, G.S.; Toppari, J.; Zoeller, R.T. EDC-2: The Endocrine Society’s second scientific statement on endocrine-disrupting chemicals. Endocr. Rev. 2015, 36, E1–E150.
- Sousa, A.C.A.; Alves, M.G.; Oliveira, P.F.; Silva, B.M.; Rato, L. Male Infertility in the XXI Century: Are Obesogens to Blame? Int. J. Mol. Sci. 2022, 23, 3046.
- Creasy, D.M. Evaluation of testicular toxicity in safety evaluation studies: The appropriate use of spermatogenic staging. Toxicol. Pathol. 1997, 25, 119–131.
- Cardoso, A.M.; Alves, M.G.; Mathur, P.P.; Oliveira, P.F.; Cavaco, J.E.; Rato, L. Obesogens and male fertility. Obes. Rev. 2017, 18, 109–125.
- Rato, L.; Sousa, A.C.A. The Impact of Endocrine-Disrupting Chemicals in Male Fertility: Focus on the Action of Obesogens. J. Xenobiot. 2021, 11, 163–196.
- Traggiai, C.; Stanhope, R. Disorders of pubertal development. Best Pract. Res. Clin. Obst. Gynaecol. 2003, 17, 41–56.
- Wilson, C.; Davies, D. The control of sexual differentiation of the reproductive system and brain. Reproduction 2007, 133, 331–359.
- Rinaldi, S.; Moret, C.; Kaaks, R.; Biessy, C.; Kurzer, M.; Dechaud, H.; Peeters, P.; Van Noord, P. Reproducibility over time of measurements of androgens, estrogens and hydroxy estrogens in urine samples from post-menopausal women. Eur. J. Epidemiol. 2003, 18, 417–424.
- Viswanathan, V.; Eugster, E.A. Etiology and treatment of hypogonadism in adolescents. Pediatr. Clin. 2011, 58, 1181–1200.
- Casey, D.E.; Zorn, S.H. The pharmacology of weight gain with antipsychotics. J. Clin. Psychiatry 2001, 62, 4–10.
- Semet, M.; Paci, M.; Saïas-Magnan, J.; Metzler-Guillemain, C.; Boissier, R.; Lejeune, H.; Perrin, J. The impact of drugs on male fertility: A review. Andrology 2017, 5, 640–663.
- Kung, J.; Henry, R.R. Thiazolidinedione safety. Exp. Opin. Drug Safety 2012, 11, 565–579.
- Alves, M.G.; Martins, A.D.; Vaz, C.V.; Correia, S.; Moreira, P.I.; Oliveira, P.F.; Socorro, S. Metformin and male reproduction: Effects on Sertoli cell metabolism. Br. J. Pharmacol. 2014, 171, 1033–1042.
- Tontonoz, P.; Spiegelman, B.M. Fat and beyond: The diverse biology of PPARγ. Annu. Rev. Biochem. 2008, 77, 289–312.
- Krentz, A.J.; Bailey, C.J. Oral antidiabetic agents: Current role in type 2 diabetes mellitus. Drugs 2005, 65, 385–411.
- Meneses, M.J.; Bernardino, R.L.; Sa, R.; Silva, J.; Barros, A.; Sousa, M.; Silva, B.M.; Oliveira, P.F.; Alves, M.G. Pioglitazone increases the glycolytic efficiency of human Sertoli cells with possible implications for spermatogenesis. Int. J. Biochem. Cell Biol. 2016, 79, 52–60.
- Ferrario, C.M.; Levy, P. Sexual dysfunction in patients with hypertension: Implications for therapy. J. Clin. Hypertens. 2002, 4, 424–432.
- Grimm Jr, R.H.; Grandits, G.A.; Prineas, R.J.; McDonald, R.H.; Lewis, C.E.; Flack, J.M.; Yunis, C.; Svendsen, K.; Liebson, P.R.; Elmer, P.J. Long-term effects on sexual function of five antihypertensive drugs and nutritional hygienic treatment in hypertensive men and women: Treatment of Mild Hypertension Study (TOMHS). Hypertension 1997, 29, 8–14.
- Manolis, A.; Doumas, M. Antihypertensive treatment and sexual dysfunction. Curr. Hypert. Rep. 2012, 14, 285–292.
- Jones, D.; Norman, A.; Horwich, A.; Hendry, W. Ejaculatory dysfunction after retroperitoneal lymphadenectomy. Eur. Urol. 1993, 23, 169–171.
- Shindel, A.; Kishore, S.; Lue, T. Drugs designed to improve endothelial function: Effects on erectile dysfunction. Curr. Pharm. Des. 2008, 14, 3758–3767.
- Becker, A.J.; Ückert, S.; Stief, C.G.; Scheller, F.; Knapp, W.H.; Hartmann, U.; Jonas, U. Plasma levels of angiotensin II during different penile conditions in the cavernous and systemic blood of healthy men and patients with erectile dysfunction. Urology 2001, 58, 805–810.
- Droupy, S. Epidemiology and Physiopathology of Erectile Dysfunction. Ann. Urol. 2005, 39, 71–84.
- Karavitakis, M.; Komninos, C.; Theodorakis, P.N.; Politis, V.; Lefakis, G.; Mitsios, K.; Koritsiadis, S.; Doumanis, G. Evaluation of sexual function in hypertensive men receiving treatment: A review of current guidelines recommendation. J. Sex. Med. 2011, 8, 2405–2414.
- Shindel, A.W.; Althof, S.E.; Carrier, S.; Chou, R.; McMahon, C.G.; Mulhall, J.P.; Paduch, D.A.; Pastuszak, A.W.; Rowland, D.; Tapscott, A.H. Disorders of ejaculation: An AUA/SMSNA guideline. J. Urol. 2022, 207, 504–512.
- Gratzke, C.; Angulo, J.; Chitaley, K.; Dai, Y.-t.; Kim, N.N.; Paick, J.-S.; Simonsen, U.; Ückert, S.; Wespes, E.; Andersson, K.E. Anatomy, physiology, and pathophysiology of erectile dysfunction. J. Sex. Med. 2010, 7 Pt 2, 445–475.
- Nudell, D.M.; Monoski, M.M.; Lipshultz, L.I. Common medications and drugs: How they affect male fertility. Urol. Clin. 2002, 29, 965–973.
- Schlosser, J.; Nakib, I.; Carré-Pigeon, F.; Staerman, F. Infertilité Masculine: Définition et Physiopathologie. Ann. Urol. 2007, 41, 127–133.
- Benoff, S.; Cooper, G.W.; Hurley, I.; Mandel, F.S.; Rosenfeld, D.L.; Scholl, G.M.; Gilbert, B.R.; Hershlag, A. The effect of calcium ion channel blockers on sperm fertilization potential. Fertil. Steril. 1994, 62, 606–617.
- Brezina, P.R.; Yunus, F.N.; Zhao, Y. Effects of pharmaceutical medications on male fertility. J. Reprod. Infertil. 2012, 13, 3.
- Kanwar, U.; Anand, R.; Sanyal, S. The effect of nifedipine, a calcium channel blocker, on human spermatozoal functions. Contraception 1993, 48, 453–470.
- De Rosa, M.; Zarrilli, S.; Di Sarno, A.; Milano, N.; Gaccione, M.; Boggia, B.; Lombardi, G.; Colao, A. Hyperprolactinemia in men: Clinical and biochemical features and response to treatment. Endocrine 2003, 20, 75–82.
- Tanrikut, C.; Schlegel, P.N. Antidepressant-associated changes in semen parameters. Urology 2007, 69, 185.e5–185.e7.
- Baldwin, D.; Mayers, A. Sexual side-effects of antidepressant and antipsychotic drugs. Adv. Psychiatr. Treat. 2003, 9, 202–210.
- Dording, C.M.; Fisher, L.; Papakostas, G.; Farabaugh, A.; Sonawalla, S.; Fava, M.; Mischoulon, D. A double-blind, randomized, pilot dose-finding study of maca root (L. meyenii) for the management of SSRI-induced sexual dysfunction. CNS Neurosci. Ther. 2008, 14, 182–191.
- Montejo, A.L.; Llorca, G.; Izquierdo, J.A.; Rico-Villademoros, F. Incidence of sexual dysfunction associated with antidepressant agents: A prospective multicenter study of 1022 outpatients. J. Clin. Psychiatry 2001, 62, 10–21.
- Erdemir, F.; Atilgan, D.; Firat, F.; Markoc, F.; Parlaktas, B.S.; Sogut, E. The effect of sertraline, paroxetine, fluoxetine and escitalopram on testicular tissue and oxidative stress parameters in rats. Int. Braz. J. Urol. 2014, 40, 100–108.
- Montejo, A.L.; Montejo, L.; Navarro-Cremades, F. Sexual side-effects of antidepressant and antipsychotic drugs. Curr. Opin. Psych. 2015, 28, 418–423.
- Safarinejad, M.R. Sperm DNA damage and semen quality impairment after treatment with selective serotonin reuptake inhibitors detected using semen analysis and sperm chromatin structure assay. J. Urol. 2008, 180, 2124–2128.
- Althof, S.E.; McMahon, C.G.; Waldinger, M.D.; Serefoglu, E.C.; Shindel, A.W.; Adaikan, P.G.; Becher, E.; Dean, J.; Giuliano, F.; Hellstrom, W.J.; et al. An Update of the International Society of Sexual Medicine’s Guidelines for the Diagnosis and Treatment of Premature Ejaculation (PE). J. Sex. Med. 2014, 2, 60–90.
- Taylor, M.J.; Rudkin, L.; Bullemor-Day, P.; Lubin, J.; Chukwujekwu, C.; Hawton, K. Strategies for managing sexual dysfunction induced by antidepressant medication. Cochrane Database Syst. Rev. 2013.
- Rosen, R.C.; Marin, H. Prevalence of antidepressant-associated erectile dysfunction. J. Clin. Psychiatry 2003, 64, 5–10.
- Panidis, D.; Rousso, D.; Skiadopoulos, S.; Panidou, E.; Mamopoulos, M. Evaluation of semen parameters in man with hyperprolactinemia induced by metoclopramide. Arch. Androl. 1997, 39, 237–242.
- Howes, O.D.; Wheeler, M.J.; Pilowsky, L.S.; Landau, S.; Murray, R.M.; Smith, S. Sexual function and gonadal hormones in patients taking antipsychotic treatment for schizophrenia or schizoaffective disorder. J. Clin. Psychiatry 2007, 68, 361–367.
- Chen, S.S.; Shen, M.R.; Chen, T.J.; Lai, S.L. Effects of antiepileptic drugs on sperm motility of normal controls and epileptic patients with long-term therapy. Epilepsia 1992, 33, 149–153.
- Isojärvi, J.; Löfgren, E.; Juntunen, K.; Pakarinen, A.; Päivänsalo, M.; Rautakorpi, I.; Tuomivaara, L. Effect of epilepsy and antiepileptic drugs on male reproductive health. Neurology 2004, 62, 247–253.
- Herzog, A.G. Disorders of reproduction in patients with epilepsy: Primary neurological mechanisms. Seizure 2008, 17, 101–110.
- Lossius, M.I.; Taubøll, E.; Mowinckel, P.; Mørkrid, L.; Gjerstad, L. Reversible Effects of Antiepileptic Drugs on Reproductive Endocrine Function in Men and Women with Epilepsy—A Prospective Randomized Double-Blind Withdrawal Study. Epilepsia 2007, 48, 1875–1882.
- Rättyä, J.; Turkka, J.; Pakarinen, A.J.; Knip, M.; Kotila, M.; Lukkarinen, O.; Myllylä, V.; Isojärvi, J. Reproductive effects of valproate, carbamazepine, and oxcarbazepine in men with epilepsy. Neurology 2001, 56, 31–36.
- Webber, M.P.; Hauser, W.A.; Ottman, R.; Annegesr, J.F. Fertility in persons with epilepsy: 1935–1974. Epilepsia 1986, 27, 746–752.
- Ocek, L.; Tarhan, H.; Uludag, F.I.; Sariteke, A.; Kose, C.; Colak, A.; Zorlu, F.; Zorlu, Y. Evaluation of sex hormones and sperm parameters in male epileptic patients. Acta. Neurol. Scand. 2018, 137, 409–416.
- Isojärvi, J.I.; Taubøll, E.; Herzog, A.G. Effect of antiepileptic drugs on reproductive endocrine function in individuals with epilepsy. CNS Drugs 2005, 19, 207–223.
- Oliva, S.U.; Scarano, W.R.; Okada, F.K.; Miraglia, S.M. Harmful effects of carbamazepine on the postnatal development of the rat ventral prostate. Reprod. Biol. Endocrinol. 2012, 10, 1–15.
- Hellstrom, W.J.; Sikka, S.C. Effects of alfuzosin and tamsulosin on sperm parameters in healthy men: Results of a short-term, randomized, double-blind, placebo-controlled, crossover study. J. Androl. 2009, 30, 469–474.
- Hellstrom, W.J.; Sikka, S.C. Effects of acute treatment with tamsulosin versus alfuzosin on ejaculatory function in normal volunteers. J. Urol. 2006, 176 Pt 1, 1529–1533.
- Røste, L.; Taubøll, E.; Mørkrid, L.; Bjørnenak, T.; Saetre, E.; Mørland, T.; Gjerstad, L. Antiepileptic drugs alter reproductive endocrine hormones in men with epilepsy. Eur. J. Neurol. 2005, 12, 118–124.
- Ghadirian, A.M.; Annable, L.; Belanger, M.C. Lithium, benzodiazepines, and sexual function in bipolar patients. Am. J. Psychiatry 1992, 149, 801–805.
More
Information
Subjects:
Reproductive Biology
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
484
Revisions:
2 times
(View History)
Update Date:
27 Feb 2024
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No





