The roles of the epidermis are multiple; above all, the protection of the organism from external influences throughout its entire life cycle and, in the case of injury, the role of healing as quickly and efficiently as possible and restoring the continuous barrier. The epidermis is maintained with an incredibly complex and perfectly coordinated keratinization process.
The process of full regeneration of the skin includes keratinocyte proliferation, early differentiation, terminal differentiation, and desquamation, which is important for maintaining healthy skin. This process is maintained by stem cells that self-renew and generate the interfollicular epidermis, hair follicles, and sebaceous glands
[1]. The role of the epidermis is to provide an impenetrable barrier, and at the same time it changes every two weeks through a highly regulated proliferation/differentiation process. When normal skin proliferation and differentiation are impaired, skin disease can occur. Skin diseases can be divided into (a) those that have abnormal and premature keratinization occurring within cells or cell groups below the stratum granulosum (e.g., Darier’s disease); (b) those where the keratinization process is both accelerated and incomplete, resulting in the retention of residual nuclei within the stratum corneum (e.g., psoriasis); and (c) those with excessive accumulation of keratin and thickening of the cornified layer or disorders related to the proper detachment of the stratum corneum (e.g., palmoplantar keratodermas, ichthyoses)
[2][3]. According to one prominent book in the literature, the group “Disorders of Keratinization” comprises the spectrum of diseases characterized by incorrect epidermal differentiation, such as ichthyosis, palmoplantar keratoderma, erythrokeratodermia, follicular hyperkeratoses, acantholytic dyskeratoses, porokeratoses, and others
[4]. Also mentioned in this group are scaly skin diseases such as lichen planus, lichen sclerosus, ichthyosis, pityriasis rubra pilaris, Darier disease, and keratosis pilaris, as well as other skin diseases.
2. Basic Features of the Keratinization Process
Keratinization (cornification) is a process by which keratinocytes differentiate, moving from the basal layer to the distinct outer layer called the stratum corneum, where they become specialized cells known as corneocytes. These cells are devoid of a nucleus and contain keratin filaments bound by a filament-aggregating protein filaggrin that contributes to the resilience and durability of the stratum corneum. It is a keratin filament-aggregating protein that serves as a major structural component of the stratum corneum that allows the skin to withstand different mechanical and chemical insults
[5][6][7]. This arrangement contributes to the resilience and durability of the stratum corneum and allows the skin to withstand different mechanical and chemical insults.
Associated with the keratinization process is the physiological process of skin desquamation, which is crucial for maintaining healthy skin. The epidermis consists of layers progressing towards the surface: stratum basale, spinosum, granulosum, lucidum (only in the palmoplantar epidermis), and corneum. The process of desquamation essentially involves the differentiation of basal progenitor cells in the epidermis into enucleated corneocytes, which desquamate through programmed cell death, though differently from the process of apoptosis
[7]. Although apoptosis and keratinization share similarities, such as the loss of the nucleus and other cell organelles, the residual product of epidermal keratinocytes, known as corneocytes, is not removed by phagocytosis but instead maintains barrier function until desquamation
[8]. Therefore, the entire epidermis from the stratum basale to the stratum corneum changes within 14 days
[9].
Keratinocyte proliferation and desquamation are critical processes in developing and maintaining healthy skin
[10]. In the skin’s normal cycle, keratinocytes are gradually produced in the epidermal basal layer, then migrate through several layers, and eventually shed off at the surface. Any dysregulation of these processes can give rise to various skin conditions. Aberrations in keratinocyte growth and turnover, for example, can lead to proliferative and retention hyperkeratosis and related disorders. Keratinocyte proliferation disorders are skin disorders characterized by excessive and rapid, novel cell production.
Over the course of a lifetime, the epidermis must continually provide an impenetrable barrier while at the same time changing rapidly, every two weeks, and retaining the ability to heal wounds. The highly regulated proliferation/differentiation program of the epidermis fulfills these different roles. The ability of the epidermis to constantly renew itself and heal wounds lies in the fact that it contains stem cells, which are progenitor cells that can self-renew and create differentiated progeny over a long period of time. The tissue microenvironment in which stem cells normally exist is called their niche.
The progeny of epidermal stem cells undergo terminal differentiation to generate the interfollicular epidermis, hair follicles, and sebaceous glands
[1]. It appears that distinct populations of stem cells exist within these structures, and the differentiation pathway chosen by their progeny is largely determined by local signals from the microenvironment
[11].
Mitotic activity of basal progenitor cells is of the most importance for normal epidermal turnover and wound healing. Basal progenitor cells are labeled by the expression of keratins 5 and 14
[12]. Basal keratinocytes create spinous cells during epidermal homeostasis. Cell production in the suprabasal cell layers is driven by mitotic spindle reorientation and asymmetric cell divisions during embryonic development
[3][13]. Differentiation from basal to spinous cells is a highly regulated transition. Spinous cells switch from a mitotic keratin 5/14 expression to a postmitotic keratin 1/10 expression.
The identifying feature of granular cells are keratohyaline granules. These granules consist of keratin, profilaggrin, and loricrin. After secretion, keratins, loricrins, as well as other proteins such as prolines, become highly cross-linked by transglutaminase to the plasma membrane and form cornified envelopes. Profilaggrin is eventually metabolized into amino acids to provide hydration and serve a UV protective function. The role of granular cells is to prevent fluid loss, using tight junctions, which are intercellular adhesions that limit the flow of fluids and ions and act as a barrier to membrane diffusion.
Stratum corneum consists of cornified envelopes, which are products of terminal differentiation in the epidermis. Cornified envelopes are acellular and anuclear structures. Their core consists of keratins surrounded by a highly crosslinked network of proteins
[14]. Structural changes accompanying differentiation are highly regulated by a cascade of pathways, including signaling pathways, epigenetic factors, transcriptional control, and posttranscriptional regulation. Notch signaling is a factor responsible for the transition of basal cells to spinous cells
[1].
3. Structure of the Epidermis and Keratinocyte Features Important for Normal Epidermal Structure
The stratum basale in the interfollicular epidermis contains cylindrical keratinocytes along with clusters of stem/progenitor cells capable of asymmetric division. Progenitor cells divide and produce both an identical transit-amplifying stem cell and a cell that begins differentiating into keratinocytes after several divisions, thus maintaining the continuous ability to divide. Keratinocytes that move into terminal differentiation separate from the basement membrane and move suprabasally due to the inactivation of integrins and extracellular matrix receptors that bind them to the basement membrane. These differentiating keratinocytes undergo a keratinization process (through the stratum spinosum, granulosum, and corneum) in the projection of the column distal to the initial stem cell. Above the layer of basal cells there are polyhedral cells of the stratum spinosum whose protein synthesis activity increases, indicating the beginning of a biochemical change in keratinization
[10].
The cells of the next layer, the stratum granulosum are flatter and broader and contain basophilic granules of keratohyaline and lamellar bodies (Odlanda)
[10]. The stratum granulosum consists of at least three layers of flattened granular cells (listed from the stratum corneum to the stratum spinosum termed SG1, SG2, and SG3)
[15][16][17][18].
Lamellar bodies are produced within the Golgi complex and stored as intracellular vesicles within the cytoplasm of SG3 cells. The contents of lamellar bodies (polar lipids, glycosphingolipids, free sterols, and phospholipids) are essentially exocytosed from the apical surface of SG2 layer cells; they move towards the space above the narrow junction line and form a lipid layer that coats corneocytes. After the formation of the lamellar body in the Golgi complex, the uptake of polar lipids into the lamellar body is regulated by ATP-binding cassette transporter 12 channels (ABCA12) located at the boundary membrane of the body. Through exocytosis of lamellar body contents, polar lipids are enzymatically converted into nonpolar ones (glycosphingolipids are hydrolyzed into ceramides, and phospholipids are converted into free fatty acids).
The protein content of keratohyaline granules includes loricrin and profilaggrin
[14]. These proteins are secreted under the signal of increased intracellular Ca
2+ in keratinocytes of the granular layer. Simultaneously, envoplakin, periplakin, and involucrin, located within the cell, covalently bind to the inner surface of the plasma membrane, and the binding process is carried out by transglutaminase 1 (also dependent on calcium concentration). At a later stage of cornification, the protein coat formed by involucrin, envoplakin, and periplakin on the keratinocyte surface is further reinforced through a covalent cross-link with loricrin. Loricrin is a hydrophobic protein that plays a role in waterproofing the cornea, ultimately becoming its main component at the end of the keratinization process.
In the stratum corneum, corneocytes are formed, which have lost all their nuclei and other organelles such as ribosomes, mitochondria, and granules
[10]. The corneocyte becomes compact and covers a larger area than the basal cell from which it developed and eventually desquamates. The intercellular space of the stratum corneum is filled with a hydrophobic layer of lipids, while below the stratum corneum, keratinocytes are immersed in the hydrophilic intercellular space. Corneocytes adhere to each other through adhesion complexes called corneodesmosomes. These complexes are formed by exocytosis of corneodesmosin, which integrates into the keratinized envelope of corneocytes within desmosomes, thus forming corneodesmosomes.
4. The Role of Keratin Expression in the Keratinization Process
Keratins are a multigenic family of proteins—as many as 54 genes encode keratin—that comprise a large proportion of keratinocytes in the epidermis
[19]. Keratins can be divided into an acidic group (group I—keratins 9–20) and alkaline group (group II—keratins 1–8)
[20]. So, α-keratin is a protein chain made up mostly of the amino acids alanine, leucine, arginine, and cysteine, which form the right-sided α-helix. In the formation of a complex structure, two of these polypeptide chains are further linked by disulfide bonds, using cysteine, to form a left-handed helical structure that is approximately 45 nm long. When formed, these dimers are then aligned with other identical dimers, following the principle of binding the terminal end of one dimer to the terminal of another through disulfide bonds, creating a protofilament.
Cytokeratins 1, 5, 10, 11, 14, and 15 are the primary keratins found in normal epidermal cells, and their distribution in the epidermis varies depending on the stage of differentiation. Hence, cytokeratin 5 is specific to normal basal cells, while cytokeratins 1 and 10 are specific to normal suprabasal cells.
Keratins in the skin fundamentally affect the structure and mitotic activity of epithelial cells, thereby maintaining mechanical stress, preserving their structural integrity, ensuring mechanical elasticity, protecting against changes in hydrostatic pressure, and establishing cell polarity
[20][21]. They also participate in cell signaling, transport, and differentiation; have the ability to modulate protein synthesis; and participate in wound healing
[10][22]. Keratins are markers for keratinocyte differentiation, and research suggests that intermediate filaments directly communicate and regulate several signaling pathways
[12][19].
Keratins in the epidermis are expressed as a keratin pair of alkaline and acidic keratin. Mitotically active keratinocytes in the basal epidermal layer primarily express the keratin pair keratin 5 and 14, with less abundant expression of keratin 15 (in the absence of keratin 14, keratin 15 can be paired with keratin 5). As keratinocytes move suprabasally toward the stratum spinosum, they withdraw from the cell cycle, reducing the expression of keratin 5 and keratin 14 and inducing differentially specific keratins 1 and 10. Further maturation of keratinocytes into the stratum granulosum results in keratin 2 expression
[19].
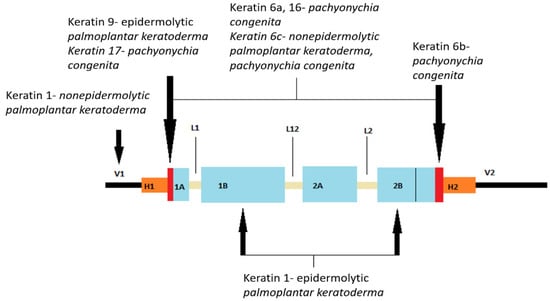
Mutations in the keratin gene cause many types of inherited palmoplantar keratodermas (PPKs), which are described in more detail later. Figure 1 shows the location of mutations in the keratin gene.
Figure 1. Representation of the secondary structure of keratin with marked mutation sites for some of the palmoplantar keratodermas (PPKs). The human genome encodes 54 functional genes for keratin, which are located in two groups on chromosomes 12 and 17. Keratin 1, being a fibrous protein, consists of a secondary protein structure divided into three domains: the N-terminal main domain, the central α-helical rod domain, and the C-terminal tail domain). The main domain further consists of three subdomains: end subdomains, variable subdomains (V1), and homologous subdomains (H1). The central rod domain consists of four α-helical subdomains (1A, 1B, 2A, 2B) connected by β-rotation regions (L). The N-terminal part of subdomain 1A is called the helix initiation motif initiating motives and the C-terminal part of subdomain 2B the protein coil termination motif. (V1 and V2, variable domains of protein head and tail; H1 and H2, homologous subdomains present only in type II keratins; parts marked red, initial and terminal motifs of the coil protein; 1A, 1B, 2A, 2B, α-helix coil domains; L1, L12, L2, connecting non-helical segments). (Modified according to: Arin MJ, Roop DR, Koch PJ, Koster MI. Biology of Keratinocytes. Bologna Dermatology. Pages: 876–887)
[19]. “Reprinted/adapted with permission from Ref.
[19]. Copyright year/2023, copyright owner’s name”/Bologna Dermatology Elsevier.
5. The Role of Ca2+ Gradient and pH in the Keratinization Process
It is important to mention the role of the Ca
2+ gradient and pH in the keratinization process. Across the epidermal layers, there is a gradient of increasing intracellular Ca
2+ concentration, with the peak concentration reached in the stratum granulosum. Intracellular Ca
2+ is stored within the ER and Golgi apparatus
[23]. It is worth noting that the extracellular space in the epidermis is much narrower than previously thought, resulting in the localization of most Ca
2+ in intracellular stores
[23]. The high concentration of calcium ions in these compartments is maintained by calcium pumps or channels, including SERCA2 (sarcoplasmic/endoplasmic reticulum Ca
2+-ATPase). Therefore, mutated SERCA2 proteins can affect the concentration of calcium ions in the endoplasmic reticulum (ER) and the dynamics of Ca
2+ in cells, which may eventually result in aberrant keratinization/epidermopoesis
[24].
Calcium regulates the transcription of all genes encoding proteins specific for keratinocyte differentiation. Additionally, calcium is essential in the posttranslational processing of profilaggrin to filaggrin. During terminal differentiation, several precursor proteins, including involucrin, loricrin, small proline-rich proteins, filaggrin, and keratin, are covalently cross-linked into the keratinized envelope by transglutaminase 1 in a calcium-dependent manner. Protein kinase C (PKC), which is activated by intracellular calcium concentration increase, induces markers of differentiation in granulated keratinocytes, including loricrin, filaggrin, and transglutaminase.
Epidermal calcium gradient is necessary for proper epidermal differentiation and barrier formation. Calcium plays a key role in controlling the transcription of genes responsible for keratinocyte differentiation by regulating the transcription of all genes encoding proteins specific for keratinocyte differentiation. The transcription factors of activator protein-1 (AP-1) are found within numerous genes specific to keratinocytes, such as transglutaminase, loricrin, involucrin, profilaggrin, and other keratins.
6. The Role and Expression of Intercellular Junctions and Channels in Epidermal Structures and Functions
The impact of desmosome components on the properties of keratinocytes and epidermal structure has recently been intensively investigated. Desmosomes are key intercellular compounds in the follicular and interfollicular epidermis. The specific composition of desmosomes is thought to influence their adhesive properties, and, in addition to having the ability to stabilize tissues, they also serve as signal transporters. Desmosomes contain two types of proteins—transmembrane proteins (desmogleins and desmocolins) and binding plaque proteins (plakophilins and plakoglobins), which are connected by keratin intermediate cytoskeletal filaments via desmoplakin
[10]. The components of the desmosome in humans are encoded by multiple genes; there are four genes for desmoglein, three for desmocholine, and three for plakophilin.
Adherent intercellular compounds consist of classical cadherins (E- and P-cadherins) and cytoplasmic protein complexes (α-catenin, β-catenin, plakoglobin) that bind transmembrane proteins to the actin microfilament of the cytoskeleton. It is important to note that plakoglobin can bind to both desmosomal and classical cadherins. As previously mentioned, β-catenin has a similar ability to plakoglobin and can transmit signals to the nucleus as a downstream effector of the classical Wnt pathway
[19].
Tight junctions (“zonule occludentes”) are considered to “seal” the intercellular space, thus preventing the free diffusion of macromolecules, making them crucial for maintaining the barrier of the two compartments in the stratum granulosum
[19].
Gap junctions are specialized intercellular connections that allow various molecules, ions (especially important for Ca
2+ traffic), and electrical impulses to pass directly from cell to cell. One channel consists of two connectors (or chemicals), which connect in the intercellular space. Oligomerization of six connexins results in a chemical channel connexon
[19].
The dysregulated differentiation process of keratinocytes during continuous epidermal renewal may cause various skin conditions or disorders. In this context, in skin physiology and skin diseases, aquaporins (AQs), which are a family of membrane proteins that form channels enabling the passage of water and small neutral solutes, are very important
[25]. Some AQs can, additionally, transport small solutes such as glycerol or urea (e.g., AQ3, 7, 9, and 10), while others are selectively permeable to water (e.g., AQ1, 2, 4, 5, and 8)
[26]. The water content in the skin is extremely high in the basal layers of the epidermis (∼75% water) and decreases sharply in the stratum corneum, which contains only 10–15% water
[27]. Corneocytes, as “dead” cells, are thought to have less need for intracellular water supplies compared to basal layer cells, for which a high water content in the cytoplasm is crucial for differentiation and physiological function.
7. Genetic Basis of the Keratinization Process
The genetic code for the keratinization process is located on chromosome 1. So, genes required for the formation of terminally differentiated epidermis are located on chromosome 1q21 in the epidermal differentiation complex. The transcriptional regulation of this complex is under strict control and is one of the main targets of the differentiation cascade. Therefore, the structural changes that occur in the keratinization process are regulated by signaling pathways, transcriptional and epigenetic factors, and post-transcriptional regulation
[14].
The p63 protein, encoded by the gene of the same name, has at least six different isoforms that activate or suppress transcription
[19]. One of the transcription factors encoded by this gene, Zinc Finger Protein 750 (ZNF750), is crucial for the expression of the second transcription factor, Krüppel-like factor 4 (Klf4), which plays a major role in gene expression for granular layer bodies
[28]. In addition, P63 also induces the expression of epidermal keratins 5 and 14
[19]. Another key function of p63 is to suppress the expression of cell cycle inhibitors and mediate exit from the cell cycle, which promotes basal layer keratinocyte proliferation. P63 also synergizes with Notch signaling to induce keratin expression 1.
“Grainyhead-like” transcription factors are also promoters of keratinocyte differentiation and are required for efficient keratinous envelope formation, in part by regulating transglutaminase-1 activity
[29].
Furthermore, protein-1 (AP-1) transcription factors are present in many keratinocyte-specific genes, including transglutaminase, loricrin, involucrin, profilaggrin, and keratin 5, 6, and 14 genes, and regulate the transcription of various differentiation markers that may be associated with its increased expression in the nucleus of keratinocytes in the stratum granulosum
[30].
8. Skin Conditions/Disorders and Related Histological Findings Associated with the Altered Process of Keratinization
Disorders and disruptions of the keratinization process and subsequent desquamation are responsible for various dermatological conditions, thus comprehending the process of keratinization is extremely important in understanding the pathogenesis of these conditions. Keratinization disorders may impact both the skin and the mucous membranes, and their clinical pictures vary significantly depending on the etiology and the extent of keratin distribution
[5][14]. The histological features associated with keratinization disorders are predominantly dyskeratosis, parakeratosis, and hyperkeratosis (
Table 1)
[31].
Table 1. The typical histological features associated with keratinization disorders.
| |
Features |
Common Skin Diseases Characterized by This Histological Feature |
| Dyskeratosis |
Abnormal, premature keratinization occurring within cells or cell groups bellow the stratum granulosum |
Keratosis follicularis (Darier’s disease), Transient acantholytic dermatosis (Grover’s disease), Pemphigus foliaceus, Subcorneal pustular dermatosis (Sneddon—Wilkinson disease), Familial benign chronic pemphigus (Hailey-Hailey disease) |
| Parakeratosis |
Keratinization process is both accelerated and incomplete, resulting in the retention of residual nuclei within the stratum corneum |
Clear cell acanthoma, Inflammatory linear verrucous epidermal nevus (ILVEN), Actinic keratosis, Lichenoid drug eruption, Porokeratosis, Psoriasis, Lichen simplex chronicus |
| Hyperkeratosis |
Excessive accumulation of keratin and thickening of the cornified layer or disorders related to the proper detachment of the stratum corneum |
Palmoplantar keratodermas, Ichthyoses, Psoriasis, Atopic dermatitis, Calluses and corns, Seborrheic keratosis, Nonmelanoma skin cancers, Blashkoid epidermolytic hyperkeratosis, Nevus sebaceus of Jadassohn (organoid nevus), Spitz nevus, Lupus erythermatosus, Lichen planopilaris, Tinea versicolor, Angiokeratoma |
In some cases, genetic defects in proteins like filaggrin, keratin, and keratohyalin, as well as enzymes responsible for cell cohesion in stratum corneum, along with molecules with roles in the signaling pathway in stratum spinosum, may underlie this pathological condition [31]. Improper desquamation and epidermopoiesis/keratinization, whether stemming from genetic mutations of factors involved in the process or arising from immune-related pathological processes, can lead to retention hyperkeratosis with regular epidermal proliferation. This differs from conditions like psoriasis, where hyperkeratosis results from increased basal layer proliferation driven by an underlying immune-related pathology [14].