Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Samih Badarny | -- | 1039 | 2024-01-19 15:59:23 | | | |
| 2 | Jason Zhu | Meta information modification | 1039 | 2024-01-22 02:47:19 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Basheer, M.; Waked, H.; Jeries, H.; Azrilin, O.; Paz, D.; Assy, N.; Naffaa, M.E.; Badarny, S. Cases of Neurosarcoidosis. Encyclopedia. Available online: https://encyclopedia.pub/entry/54128 (accessed on 07 February 2026).
Basheer M, Waked H, Jeries H, Azrilin O, Paz D, Assy N, et al. Cases of Neurosarcoidosis. Encyclopedia. Available at: https://encyclopedia.pub/entry/54128. Accessed February 07, 2026.
Basheer, Maamoun, Hamd Waked, Helana Jeries, Olga Azrilin, Dan Paz, Nimer Assy, Mohammad E. Naffaa, Samih Badarny. "Cases of Neurosarcoidosis" Encyclopedia, https://encyclopedia.pub/entry/54128 (accessed February 07, 2026).
Basheer, M., Waked, H., Jeries, H., Azrilin, O., Paz, D., Assy, N., Naffaa, M.E., & Badarny, S. (2024, January 19). Cases of Neurosarcoidosis. In Encyclopedia. https://encyclopedia.pub/entry/54128
Basheer, Maamoun, et al. "Cases of Neurosarcoidosis." Encyclopedia. Web. 19 January, 2024.
Copy Citation
Sarcoidosis is a chronic granulomatous disease of unknown cause characterized by the presence of non-caseating granulomas. The disease can affect any organ including the nervous system. Neurosarcoidosis occurs in about 5% patients with sarcoidosis. The clinical presentation of neurosarcoidosis is varied, and it can involve the brain, spinal cord and peripheral nervous system, separately or in different combinations. The diagnosis of neurosarcoidosis is challenging, as biopsies from the nervous system are not readily available. Anti-TNFα agents are becoming one of the cornerstone treatments for neurosarcoidosis.
neurosarcoidosis
anti-TNFα agents
infliximab
1. Introduction
Sarcoidosis is a multisystemic inflammatory disease characterized by the formation of non-caseating granulomas in various organ systems, mainly in the lungs and lymphatic system [1][2]. Although the pathogenesis of sarcoidosis is not yet fully understood, environmental and genetic factors may contribute to its pathogenesis and lead to an exaggerated granulomatous response [1][2]. Sarcoidosis occurs worldwide and affects all races and age groups [1]. The clinical manifestation, natural course and prognosis of sarcoidosis vary widely [1][2][3][4].
Any tissue can be affected, although the lungs, skin, eyes and liver are the most commonly affected [1][2][3]. The lymphatic system is almost always affected. At the onset of the disease, the lungs are affected in 95% of cases, and multisystem disease is present in about half of cases [1][2][3][4][5]. Neurological symptoms represent the first defining manifestation of sarcoidosis in almost 50% of cases [6][7]. Neurosarcoidosis occurs in 5–10% of patients with sarcoidosis, and these rates are not influenced by race or gender [3][4][5]. The clinical manifestations of neurosarcoidosis are also heterogeneous, as granulomas can affect any part of the brain. Cranial neuropathy is the most common manifestation, with the facial nerves being the most commonly affected [6][7].

2. Case 1
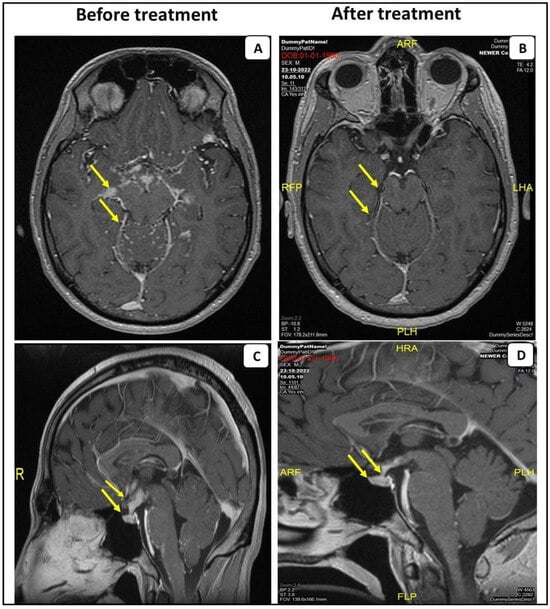
A 34-year-old healthy male, admitted to the emergency room (ER) due to a confusional state. A month prior to his admission, he complained about headaches, decreased sexual function and weight loss. Brain computed tomography (CT) without contrast demonstrated a hypodense process in the pituitary gland and above it on the right side, producing pressure in the same area. Consequently, brain magnetic resonance imaging (MRI) was performed showing a hypothalamic lesion involving the pituitary stalk, accompanied by secondary leptomeningeal spread mainly to the brain and the basal cisterns (Figure 1A,C). The differential diagnosis of the radiologic findings included neurosarcoidosis, tuberculosis or metastasis. The patient underwent the following workup: An electroencephalogram (EEG) on alertness was slightly disturbed, due to slowing over the frontal area. A Lumbar puncture (LP) showed 98 white blood cells, the majority of which were lymphocytes, a protein level of 330 mg/dL and a glucose level of 30 mg/dL. A BIOFIRE test, a detector panel of a wide range of viruses and bacteria in the cerebrospinal fluid (CSF), was negative. Syphilis serology was negative. Cytology tests showed small lymphocytes and a few histiocytes. Polymerase chain reaction (PCR) for tuberculosis was negative as well. Vitamin B12 and thyroid stimulating hormone (TSH) were normal. Human immunodeficiency virus (HIV) was negative. Synacthen test was also normal. The patient’s visual fields test was normal.
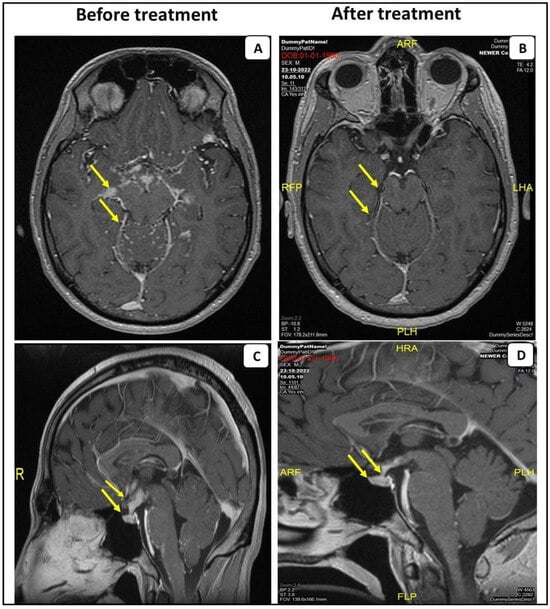
Figure 1. MRI scans with contrast of the first patient before and after the anti-TNF-α treatment. Post-gadolinium T1 MRI from the patient with probable NS, demonstrating leptomeningeal enhancement predominantly affecting the basal cistern of the brain and leptomeningeal spread within the folia of the cerebellum (A). Sagittal post-gadolinium T1 MRI demonstrates abnormal contrast enhancement and swelling of the pituitary gland (arrowhead) (C). Anti-TNF-α treatment resolved these findings (B,D).
Chest and abdominal CTs were negative for malignancy. Mediastinal lymphadenopathy was demonstrated. Endobronchial ultrasound (EBUS) examination and sampling of the lymph node was performed. The biopsy showed columnar epithelial cells, lymphocytes and multinucleated cells on the surfaces. No malignant cells were observed. Detached tiny fragments of lymphoid tissue with a focus on non-necrotizing granuloma were evident.
The patient was treated with high-dose methylprednisilone (1000 mg per day for three sequential days). Clinical improvement was observed. He was discharged with a scheduled prednisone tapering along with weekly oral 20 mg/w of methotrexate. Due to residual disease on the following brain MRI, intravenous infliximab was added to treatment, 5 mg/kg (0, 2 and 6 weeks of a loading dose and every 8 weeks for maintenance), with subsequent clinical and imaging improvement (Figure 1B,D).
3. Case 2
A 49-year-old male, diagnosed with sarcoidosis one year prior to his current admission. The diagnosis of sarcoidosis was based on chronic dyspnea and a cough, and a mediastinal lymph node biopsy showing non-caseating granuloma. Methotrexate (MTX) was initiated, but was later stopped due to severe side effects and replaced by azathioprine. In the current admission, the patient presented to the ER with left leg weakness, walking difficulty and recurrent falls and confusion for several days. Brain CT without contrast was normal. A lumbar puncture revealed 213 white blood cells, 988 mg/dL protein and 35 mg/dL glucose. Due to the patient’s immunocompromised status, treatment with acyclovir, ceftriaxone and vancomycin was initiated. The CSF fluid was negative for micro-organisms and CSF cultures were negative. West Nile virus, HIV, VDRL and PCR for herpes and varicella zoster virus (VZV), tuberculosis (TB), non-tubercles mycobacteria, Nocardia and JC virus were all negative. Anti-viral and anti-bacterial therapy were withheld. MRI of the brain was ambiguous and EEG was normal. Due to proximal weakness in the left leg, an electromyogram (EMG) was performed showing left-sided L4-5 radiculopathy. A lumbar spine CT showed a bulging disc at L2-3 on the right (which did not explain the patient’s complaints).
Spinal MRI demonstrated a significant enhancement of the lumbar nerve roots accompanied by an enhancement of the intra-dural CSF space surrounding the spinal cord at the level of the conus medullaris (Figure 2). Angiotensin converting enzyme (ACE) levels in the CSF were very high (159,000 U/L), which may confirm the diagnosis of neurosarcoidosis. Methylprednisolone pulse therapy was initiated with subsequent clinical improvement. Later, the patient was transferred to the rehabilitation department with a plan for prednisone tapering down. Because of the previous failure on methotrexate (due to elevated liver enzymes) and azathioprine (lack of efficacy), treatment with infliximab was initiated intravenously with the successful tapering down of prednisone along with clinical improvement.

Figure 2. MRI scans with contrast of the second patient before the anti-TNF-α treatment. Spinal MRI of the second patient. Sagittal post-gadolinium T1 MRI of the lumbar spine demonstrating nodular leptomeningeal enhancement about the cauda equina (arrowhead).
References
- Valeyre, D.; Prasse, A.; Nunes, H.; Uzunhan, Y.; Brillet, P.-Y.; Müller-Quernheim, J. Sarcoidosis. Lancet 2014, 383, 1155–1167.
- Drent, M.; Strookappe, B.; Hoitsma, E.; De Vries, J. Consequences of sarcoidosis. Clin. Chest Med. 2015, 36, 727–737.
- Baughman, R.P.; Teirstein, A.S.; Judson, M.A.; Rossman, M.D.; Yeager, H., Jr.; Bresnitz, E.A.; De Palo, L.; Hunninghake, G.; Iannuzzi, M.C.; Johns, C.J.; et al. Clinical characteristics of patients in a case control study of sarcoidosis. Am. J. Respir. Crit. Care Med. 2001, 164, 1885–1889.
- Gosselin, J.; Roy-Hewitson, C.; Bullis, S.S.; DeWitt, J.C.; Soares, B.P.; Dasari, S.; Nevares, A. Neurosarcoidosis: Phenotypes, Approach to Diagnosis and Treatment. Curr. Rheumatol. Rep. 2022, 24, 371–382.
- Pietinalho, A.; Ohmichi, M.; Hiraga, Y.; Löfroos, A.B.; Selroos, O. The mode of presentation of sarcoidosis in Finland and Hokkaido, Japan. A comparative analysis of 571 Finnish and 686 Japanese patients. Sarcoidosis Vasc. Diffuse Lung Dis. 1996, 13, 159–166.
- Fritz, D.; Voortman, M.; van de Beek, D.; Drent, M.; Brouwer, M.C. Many faces of neurosarcoidosis: From chronic meningitis to myelopathy. Curr. Opin. Pulm. Med. 2017, 23, 439–446.
- Stern, B.J.; Royal, W., III; Gelfand, J.M.; Clifford, D.B.; Tavee, J.; Pawate, S.; Berger, J.R.; Aksamit, A.J.; Krumholz, A.; Pardo, C.A.; et al. Definition and Consensus Diagnostic Criteria for NeurosarcoidosisFrom the Neurosarcoidosis Consortium Consensus Group. JAMA Neurol. 2018, 75, 1546–1553.
More
Information
Subjects:
Clinical Neurology
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
573
Revisions:
2 times
(View History)
Update Date:
22 Jan 2024
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




