Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Hendrik Terheyden | -- | 2765 | 2024-01-18 17:12:17 | | | |
| 2 | Lindsay Dong | Meta information modification | 2765 | 2024-01-19 04:25:45 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Terheyden, H.; Raghoebar, G.M.; Sjöström, M.; Starch-Jensen, T.; Cawood, J. Preprosthetic Surgery. Encyclopedia. Available online: https://encyclopedia.pub/entry/54061 (accessed on 07 February 2026).
Terheyden H, Raghoebar GM, Sjöström M, Starch-Jensen T, Cawood J. Preprosthetic Surgery. Encyclopedia. Available at: https://encyclopedia.pub/entry/54061. Accessed February 07, 2026.
Terheyden, Hendrik, Gerry M. Raghoebar, Mats Sjöström, Thomas Starch-Jensen, John Cawood. "Preprosthetic Surgery" Encyclopedia, https://encyclopedia.pub/entry/54061 (accessed February 07, 2026).
Terheyden, H., Raghoebar, G.M., Sjöström, M., Starch-Jensen, T., & Cawood, J. (2024, January 18). Preprosthetic Surgery. In Encyclopedia. https://encyclopedia.pub/entry/54061
Terheyden, Hendrik, et al. "Preprosthetic Surgery." Encyclopedia. Web. 18 January, 2024.
Copy Citation
The atrophic edentulous jaw can cause severe functional impairment for patients, leading to inadequate denture retention, reduced quality of life, and significant health problems. The aim of preprosthetic surgery is to restore function and form due to tooth loss arising from congenital deformity, trauma, or ablative surgery. Alveolar bone loss is due to disuse atrophy following tooth loss. The advent of dental implants and their ability to preserve bone heralded the modern version of preprosthetic surgery. Their ability to mimic natural teeth has overcome the age-old problem of edentulism and consequent jaw atrophy.
alveolar bone atrophy
alveolar bone loss
bone grafting
dental implants
edentulous jaw
preprosthetic oral surgery procedures
1. Introduction
The term preprosthetic surgery was coined in the 1960s by Professor Hugo Obwegeser. Subsequently, in the 1980s, the International Research Group for Preprosthetic Surgery (IRGPS, now renamed the International Academy for Oral and Facial Rehabilitation “www.iaofr.org (accessed on 21 November 2023)”) was founded by John Cawood, Franz Härle, Eric Hjorting-Hansen, Hans de Koomen, Soren Hillerup, Hermann Sailer, Paul Stoelinga, Bill Terry, et al. [1], laid the foundation for contemporary preprosthetic surgery involving relative heightening of the edentulous ridge by soft tissue surgery (vestibuloplasty to increase the area of fixed mucosa) and absolute heightening of the edentulous ridge by bone grafting [2][3] including osteotomies (sandwich and visor in the mandible and Le Fort 1 in the maxilla) to increase denture retention. Unfortunately, until the advent of dental implants, these methods only provided temporary success as further resorption occurred due to denture-induced pressure [4].
Alveolar bone develops with tooth formation during facial growth. Consequently, following tooth loss, the alveolar bone resorbs due to disuse atrophy. Thus far, no pharmacological or surgical means, including socket preservation [5], has been found to prevent this physiological process other than the occlusal forces delivered by natural teeth. However, the realization that endosseous implants replacing natural teeth also prevent resorption by their ability to transmit functional loading internally forms the basis for predictable contemporary preprosthetic surgery. Grafted bone remains stable when subjected to functional loading by endosteal implants [6].
Jawbone regeneration in combination with dental implants is more than just enabling a dental prosthesis; it offers functional and aesthetic maxillofacial rehabilitation and has superseded tissue replacement by a plastic prosthesis, at least in younger patients. Nowadays, survival of natural teeth is the norm, rendering edentulism rare unless congenital absence, disease, trauma, or ablation intervenes, in which case oral rehabilitation is indicated. Not all patients can benefit from state-of-the-art preprosthetic surgery for health or economic reasons or due to the burden of surgery. Even so, other less invasive treatments involving more bulky prosthetic replacement aided by dental implants can suffice. The best results for rehabilitation are achieved by the team approach of surgeons, maxillofacial prosthodontists/general dentists, and, importantly, informing patients about the available preprosthetic surgical options.
2. Soft versus Hard Tissue Augmentation in the Anterior Region
Implant treatment in the aesthetic zone is a highly reliable option for the rehabilitation of failing or missing teeth [7]. With the demand for the most satisfying aesthetic outcome, the focus has shifted from just implant survival to enhancement and preservation of the hard and soft peri-implant tissues.
The alveolar ridge is subject to continual change, both horizontally and vertically, following tooth extraction [8], especially in the pre-maxilla. Therefore, placing dental implants in the aesthetic zone can be challenging as there is often a pre-existing deficiency of the alveolar ridge, which tends to compromise an aesthetic result. Augmenting the bone and soft tissue before or during implant placement can improve peri-implant conditions, but the timing and nature of any intervention to restore bone and soft tissue volume remains a matter of debate.
Bone augmentation is clearly indicated when an implant is incompletely covered by bone. It may be necessary to apply bone grafts and/or guided bone regeneration (GBR) to create enough bone volume. Guided bone regeneration is a well-documented technique and is effective in reducing bone defects that remain after implant placement. The aim of GBR is the establishment of a facial bone wall of sufficient thickness and height to support the soft tissues. Long-term GBR studies, in combination with implant placement, have demonstrated that thick and stable buccal bone walls can be achieved after lateral bone augmentation [9][10]. However, GBR can be invasive, involving at least one vertical releasing incision as well as a release of the periosteum and muscle insertion, increasing morbidity and mucosal scarring along the releasing incision(s) [11].
Even if there is no bone defect and no need for a bone graft, there may be a need for soft tissue grafting to improve the thickness and contour of the facial mucosa. Grafting of the peri-implant soft tissues can be performed before, simultaneously with implant placement, during osseointegration of the implant, or after prosthetic reconstruction [12]. Inadequate soft tissue dimensions can result in aesthetic and functional complications, oral hygiene maintenance, phonetic impediments, and susceptibility to mucosal recession.
Soft tissue augmentation has also been proposed to re-establish buccal convexity. This approach can be considered when there is sufficient bone for complete embedment of the implant shoulder as well as when minor buccal bone defects causing soft tissue concavities are present [12][13][14]. The outcome of soft tissue augmentation is clinically relevant because thicker tissues enhance peri-implant health [13] and result in higher patient satisfaction and superior aesthetics [15]. Soft tissue augmentation in the aesthetic zone has been shown to result in less recession and a thicker mid-buccal mucosa following immediate implant placement and in less recession in the mid-buccal mucosa following delayed implant placement compared to no graft (Figure 1A–D) [12].
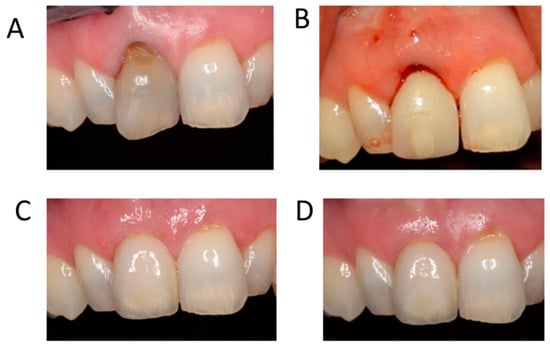
Figure 1. Immediate implant placement with immediate provisionalization and soft tissue grafting. (A) Clinical situation preoperative with failing 11 and thin mucosa. (B) Clinical situation after implant placement in the grafted socket without flap elevation, soft tissue grafting on the labial side, and placement of the screw-retained provisional crown. The tooth was removed in the same session. (C) Clinical situation after 1 year. (D) Clinical situation after 5 years. Nice contour and healthy aspect of the mucosa comparable to the neighboring teeth.
The materials used for soft tissue grafting can be classified into three categories: (1) subepithelial connective tissue grafts harvested from the patients’ palates or tuberosities, (2) allografts, and (3) xenografts. Soft tissue substitutes (a volume-stable collagen matrix) resulted in similar stable peri-implant tissues, favorable aesthetics, and clinically negligible contour changes at 5 years post-loading than after using a subepithelial connective tissue graft [16]. However, in another study, the sites treated with a volume-stable collagen matrix demonstrated more shrinkage and significantly more marginal bone loss than those treated with a subepithelial connective tissue graft after 1 year [17]. Patient-reported outcome measures following soft tissue augmentation with soft tissue substitutes indicate a reduction in pain, less need for painkillers, and shorter surgery time while achieving similar patient satisfaction levels compared with autogenous grafts without impairing the clinical outcomes [18].
In summary, bone augmentation is needed to reconstruct a deficient ridge to a form that will ensure that an aesthetic implant-supported restoration with a good aesthetic outcome can be fabricated. Soft tissue augmentation is needed to improve the functional and aesthetic outcomes if there is any compromise in soft tissue thickness or quantity.
3. Bone Reconstruction of the Anterior Maxilla
Tissue defects in the aesthetic area can be compensated by prosthetic means like artificial gingiva. However, knowledge of surgical procedures, bone remodeling, and osseointegration helps us to find a regenerative solution. When analyzing long-term prognosis and aesthetical results, the use of autogenous bone grafting and alveolar ridge reconstruction is the first choice, provided that the patient is fit for surgery. The aim is that the alveolar bone is adequate in height and width as well as providing support for a natural gingiva covering.
Replacement of the dentition in the anterior maxilla is demanding aesthetically, biologically, and biomechanically due to limited alveolar bone volume [19][20]. Trauma of the anterior maxilla is the major cause of the loss of a central incisor [21], whereas congenital absence is responsible for the majority of missing lateral incisors [22].
The buccal bone thickness in the anterior maxilla seldom exceeds one millimeter [23], and coupled with a further loss of about 50% during the healing process [24], compensation for ridge reduction is required. Avila-Ortiz et al. [25] evaluated techniques for alveolar ridge preservation and reported nine different ridge preservation treatment methods to reduce ridge resorption after tooth extraction. Although alveolar ridge preservation is positive, no superior method was found.
If the preoperative clinical and radiographic examination indicates insufficient alveolar bone volume, usually, two treatment options can be offered: prosthetic replacement with artificial gingiva (pink porcelain) or with a removable denture. In contrast, pre-implant bone reconstruction provides support for endosteal implants and support for the upper lip and a natural gingival appearance [26][27][28][29][30][31]. Each of these approaches reports good predictable results, but outcomes of bone reconstruction are technique-sensitive. The autogenous bone graft placed prior to implant surgery is widely reported [27][28][32]. One important factor for a predictable result after bone reconstruction is the degree of postoperative graft volume change that takes place during initial healing and remodeling.
In severe vertical discrepancies, distraction osteogenesis can be used for reconstruction in the anterior maxilla, but the result compared to onlay bone grafting in terms of bone gain and bone resorption is questionable [33]. Zhao et al. [34] performed a systematic review of vertical distraction osteogenesis and concluded that vertical alveolar defects could be repaired successfully with distraction osteogenesis, and the implant placed in the distraction sites showed a high cumulative survival rate. However, the high complication rate necessitates caution. In situations with malignancies in the anterior maxilla, irradiation may be required. Irradiation impairs blood supply to the alveolar bone [35], which further compounds treatment. If implant treatment is decided, a minimally invasive surgical technique is mandatory [36].
Marginal soft tissue is also important in the reconstruction of the anterior maxilla. Bienz et al. [37] concluded that increased soft tissue thickness at implant sites was associated with more favorable aesthetic outcomes. Hosseini et al. [38] compared connective tissue grafts harvested from the palate with a control group after both groups had received an implant in the anterior maxilla. The authors concluded that augmentation using a connective tissue graft may result in better mucosal color match and more facial dimensional gain compared to implant sites without soft tissue grafting.
4. Sinus Floor Augmentation and Standard-Length Implants versus Short Implants
Prosthetic rehabilitation of the moderately atrophic posterior maxilla with an implant-supported restoration is traditionally solved by grafting of the sinus floor for accommodation of standard-length dental implants.
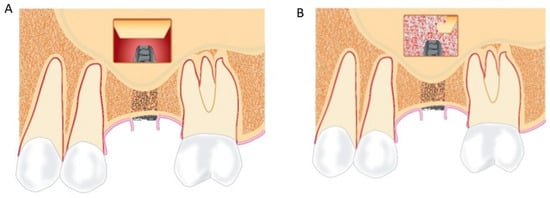
Maxillary sinus floor augmentation applying the lateral window technique and placement of a grafting material underneath the elevated Schneiderian membrane is frequently used to increase the alveolar ridge height of the atrophic posterior maxilla (Figure 2A,B). High survival rates of superstructures and implants, bone regeneration, limited peri-implant marginal bone loss, and low frequency of complications have been reported in systematic reviews and meta-analyses [39][40][41][42]. Autogenous bone graft generates the highest amount of new bone formation compared with other grafting materials in conjunction with sinus floor augmentation [43][44]. However, the use of autologous bone grafts is associated with supplementary surgery, risk of donor site morbidity, and an unpredictable resorption of the augmented volume [45][46][47][48].
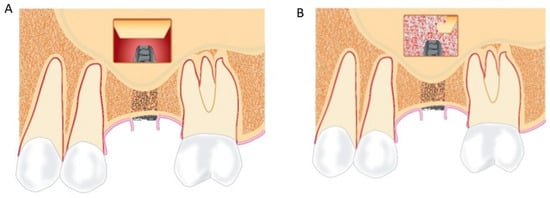
Figure 2. (A) The lateral bony window and the Schneiderian membrane are elevated from the original maxillary sinus floor, and a standard-length implant is inserted. The inserted implant is partially visible in the created compartment. (B) A grafting material is packed around the implant in the created compartment.
Prosthetic rehabilitation in the atrophic posterior maxilla with a short implant has been proposed to preclude alveolar ridge augmentation (Figure 3). The definition of a short implant is inconsistent, and implant lengths between 6 mm and 10 mm have been defined as a short implant. Placement of short implants is associated with a reduced bone-to-implant contact and increased crown-to-implant ratio compared with placement of standard-length implants, which could lead to an increased risk of implant failure or loss.
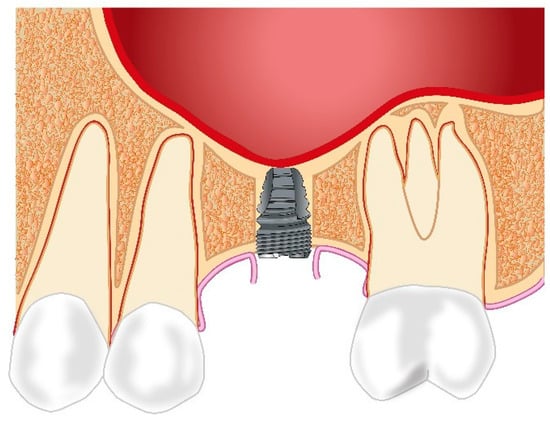
Figure 3. A short implant is inserted in the posterior maxilla avoiding maxillary sinus floor augmentation and the use of a grafting material.
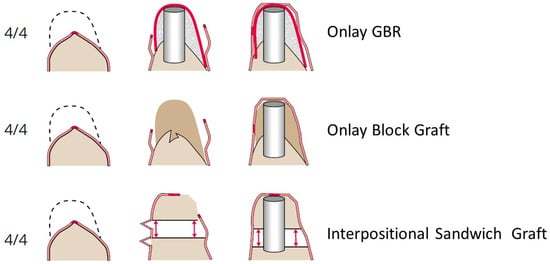
5. Vertical Ridge Augmentation—Sandwich versus Onlay Grafting
In the past, it has often been questioned whether a substantial vertical ridge augmentation with long-term stability is possible because a continuing jaw atrophy, especially in the absence of dental implants, was observed [4].
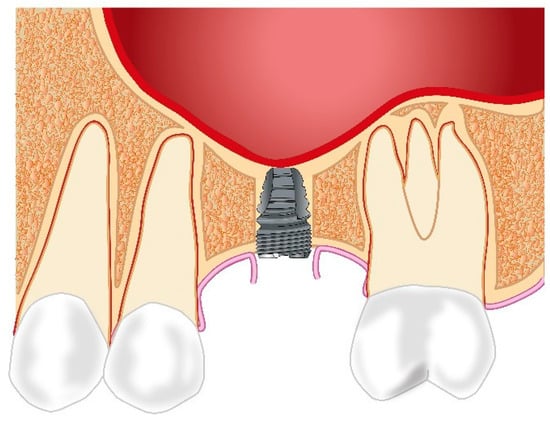
To be functional, a non-vascularized bone graft must first become integrated and then remodeled by the process of neoangiogenesis within the bone graft. The new blood vessels grow into the graft from the base of the bone defect. Traditionally, onlay bone grafts were mainly used prior to implant placement. According to the quarter classification of bone deficits in the site of a dental implant (Terheyden [49]), the required amount of blood vessel growth increases with the defect class (Figure 4).
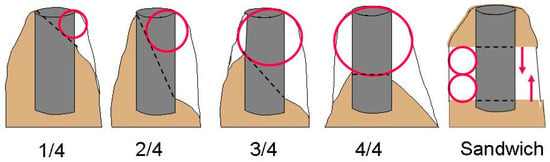
Figure 4. The quarter classification (Terheyden [49]) describes the bone deficit in an implant site in relation to the planned dental implant, starting with buccal bone loss of < 50% of the implant length (1/4), then buccal bone loss > 50% (2/4), then lingual/palatal bone loss < 50% (3/4) and finally loss of the alveolar crest buccal and palatal > 50% (4/4). The red circles indicate the required distance, which neoangiogenesis has to bridge to integrate a bone graft. The clinical limit is 3.7 mm. On the right side, it is shown that an interpositional graft between two vascularized bone surfaces doubles the bridging distance (7.4 mm), because blood vessels can grow from two directions as indicated by the red arrows.
Neoangiogenesis inside autogenous block grafts is enhanced by “creeping substitution” which involves “bone-cutting cones” similar to the remodeling of compact bone [49]. It has been reported that, on average, 5.8 mm of new bone can be substantially gained and remodeled within a few years [50]. For this reason, autologous block bone grafts became the traditional method for vertical augmentation of more than 3.7 mm.
With onlay grafts, the need for primary coverage causes soft tissue tension when mobilizing the flap, which can result in wound dehiscence with partial or complete loss of the bone graft, which has been reported as high as 33–40% [51] On the other hand, the sandwich interpositional graft requires less flap mobilization. Although a 25% incidence of wound dehiscence is reported, the incidence of graft infection and rejection after sandwich grafting in the mandible was only 1.3% [52].
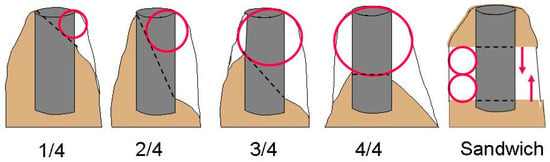
Coverage of an onlay bone block or vertical guided bone regeneration (GBR) site requires the buccal tissue to be moved crestally, advanced over the graft in a palatal or lingual direction, and finally further stretched down apically to engage the pristine lingual/palatal mucosal margin. This triple flap mobilization usually ends with a palatal or lingual shift of the mucogingival border (Figure 5).
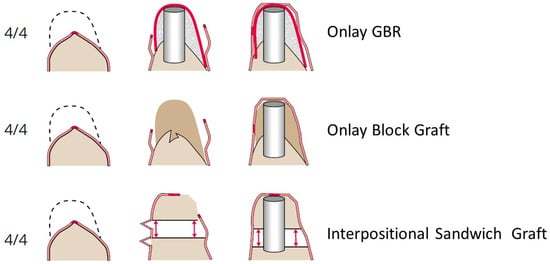
Figure 5. Different treatment options for a 4/4 defect. The dotted lines indicate the intended shape of the ridge after bone augmentation. The bold red part in the middle of the mucosal lining of the alveolar crest is the small area of fixed gingival tissue (masticatory gingiva). Due to the requirements of soft tissue coverage, the two onlay grafting options (GBR and block) cause a shift of the mucogingival junction, often requiring secondary soft tissue augmentation. In the interpositional grafting technique, the soft tissue on the lingual side stays attached to the bone segment, and this forms the new emergence profile of the dental implant. The implant is, therefore, covered from both sides with the original fixed gingival tissue. Very rarely, is secondary soft tissue augmentation needed.
Bone graft resorption is usually a surface resorption at denuded bone surfaces. During interpositional grafting, the lingual/palatal soft tissues stay attached to the transported bone segment [49]. Only the periosteum of the lingual or palatal flap has to be dissected to gain some freedom for the elevation of the transport segment. This is relatively easy in the mandible, but in the maxilla, the rigid palatal soft tissue allows only a vertical transport of 3–4 mm. The crestal soft tissues must not be detached from the transport segment because this would impede blood perfusion and result in surface resorption at the site where subsequent dental implants emerge. In sandwich grafting, the palatal or lingual soft tissues stay attached to the bone.
However, the limitations of interpositional grafting should be mentioned. When scar tissue or the rigid palatal mucoperiosteum allows only limited movements of the bone transport segment, distraction osteogenesis may be a better option [49]. The thin bone inferior to the maxillary sinus in the posterior maxilla is often a contraindication for segmental osteotomies, as well as a bone level of less than 4 mm superior to the alveolar nerve in the posterior mandible. In such situations, sinus grafting (inlay osteoplasty) or an onlay block graft in the mandible is indicated. However, in the posterior mandible with at least 4 mm or more residual bone superior to the nerve, the sandwich technique, even in a 3/4 defect with a knife edge ridge, is possible [49].
References
- Cawood, J.I.; Stoelinga, P.J.W. International academy for oral and facial rehabilitation—Consensus Report. Int. J. Oral. Maxillofac. Surg. 2006, 35, 195–198.
- Bell, R.B.; Blakey, G.H.; White, R.P.; Hillebrand, D.G.; Molina, A. Staged reconstruction of the severely atrophic mandible with autogenous bone graft and endosteal implants. J. Oral. Maxillofac. Surg. 2002, 60, 1135–1141.
- Sassano, P.; Gennaro, P.; Chisci, G.; Gabriele, G.; Aboh, I.V.; Mitro, V.; di Curzio, P. Calvarial onlay graft and submental incision in treatment of atrophic edentulous mandibles: An approach to reduce postoperative complications. J. Craniofac. Surg. 2014, 25, 693–697.
- Härle, F. Präprothetische Operationen; Hanser: Munich, Germany, 1983.
- Chisci, G.; Hatia, A.; Chisci, E.; Chisci, D.; Gennaro, P.; Gabriele, G. Socket Preservation after Tooth Extraction: Particulate Autologous Bone vs. Deproteinized Bovine Bone. Bioengineering 2023, 10, 421.
- Boven, G.C.; Meijer, H.J.A.; Vissink, A.; Raghoebar, G.M. Reconstruction of the extremely atrophied mandible with iliac crest onlay grafts followed by two endosteal implants: A retrospective study with long-term follow-up. Int. J. Oral. Maxillofac. Surg. 2014, 43, 626–632.
- den Hartog, L.; Slater, J.J.; Vissink, A.; Meijer, H.J.; Raghoebar, G.M. Treatment outcome of immediate, early and conventional single-tooth implants in the aesthetic zone: A systematic review to survival, bone level, soft-tissue, aesthetics and patient satisfaction. J. Clin. Periodontol. 2008, 35, 1073–1086.
- Couso-Queiruga, E.; Stuhr, S.; Tattan, M.; Chambrone, L.; Avila-Ortiz, G. Post-extraction dimensional changes: A systematic review and meta-analysis. J. Clin. Periodontol. 2021, 48, 126–144.
- Buser, D.; Chappuis, V.; Bornstein, M.M.; Wittneben, J.G.; Frei, M.; Belser, U.C. Long-term stability of contour augmentation with early implant placement following single tooth extraction in the esthetic zone: A prospective, cross-sectional study in 41 patients with a 5- to 9-year follow-up. J. Periodontol. 2013, 84, 1517–1527.
- Chappuis, V.; Rahman, L.; Buser, R.; Janner, S.F.M.; Belser, U.C.; Buser, D. Effectiveness of Contour Augmentation with Guided Bone Regeneration: 10-Year Results. J. Dent. Res. 2018, 97, 266–274.
- De Bruyckere, T.; Cosyn, J.; Younes, F.; Hellyn, J.; Bekx, J.; Cleymaet, R.; Eghbali, A. A randomized controlled study comparing guided bone regeneration with connective tissue graft to re-establish buccal convexity: One-year aesthetic and patient-reported outcomes. Clin. Oral Implant. Res. 2020, 31, 507–516.
- Raghoebar, G.M.; Korfage, A.; Meijer, H.J.A.; Gareb, B.; Vissink, A.; Delli, K. Linear and profilometric changes of the mucosa following soft tissue augmentation in the zone of aesthetic priority: A systematic review and meta-analysis. Clin. Oral Implant. Res. 2021, 32 (Suppl. S21), 138–156.
- Tavelli, L.; Barootchi, S.; Avila-Ortiz, G.; Urban, I.A.; Giannobile, W.V.; Wang, H.L. Peri-implant soft tissue phenotype modification and its impact on peri-implant health: A systematic review and network meta-analysis. J. Periodontol. 2021, 92, 21–44.
- Thoma, D.S.; Cosyn, J.; Fickl, S.; Jensen, S.S.; Jung, R.E.; Raghoebar, G.M.; Rocchietta, I.; Roccuzzo, M.; Sanz, M.; Sanz-Sanchez, I.; et al. Soft tissue management at implants: Summary and consensus statements of group 2. The 6th EAO Consensus Conference 2021. Clin. Oral Implant. Res. 2021, 32 (Suppl. S21), 174–180.
- Stefanini, M.; Tavelli, L.; Barootchi, S.; Sangiorgi, M.; Zucchelli, G. Patient-reported outcome measures following soft-tissue grafting at implant sites: A systematic review. Clin. Oral Implant. Res. 2021, 32 (Suppl. S21), 157–173.
- Thoma, D.S.; Gasser, T.J.W.; Hammerle, C.H.F.; Strauss, F.J.; Jung, R.E. Soft tissue augmentation with a volume-stable collagen matrix or an autogenous connective tissue graft at implant sites: Five-year results of a randomized controlled trial post implant loading. J. Periodontol. 2023, 94, 230–243.
- Cosyn, J.; Eeckhout, C.; De Bruyckere, T.; Eghbali, A.; Vervaeke, S.; Younes, F.; Christiaens, V. A multi-centre randomized controlled trial comparing connective tissue graft with collagen matrix to increase soft tissue thickness at the buccal aspect of single implants: 1-year results. J. Clin. Periodontol. 2022, 49, 911–921.
- Thoma, D.S.; Strauss, F.J.; Mancini, L.; Gasser, T.J.W.; Jung, R.E. Minimal invasiveness in soft tissue augmentation at dental implants: A systematic review and meta-analysis of patient-reported outcome measures. Periodontol. 2000 2023, 91, 182–198.
- Ramanauskaite, A.; Sader, R. Esthetic complications in implant dentistry. Periodontol. 2000 2022, 88, 73–85.
- Romanos, G.E.; Delgado-Ruiz, R.; Sculean, A. Concepts for prevention of complications in implant therapy. Periodontol. 2000 2019, 81, 7–17.
- Yang, X.; Sun, W.; Wang, Z.; Ji, A.P.; Bai, J. . Beijing Da Xue Xue Bao Yi Xue Ban 2021, 53, 384–389.
- Rakhshan, V. Meta-Analysis of Observational Studies on the Most Commonly Missing Permanent Dentition (Excluding the Third Molars) in Non-Syndromic Dental Patients or Randomly-Selected Subjects, and the Factors Affecting the Observed Rates. J. Clin. Pediatr. Dent. 2015, 39, 199–207.
- Tsigarida, A.; Toscano, J.; de Brito Bezerra, B.; Geminiani, A.; Barmak, A.B.; Caton, J.; Papaspyridakos, P.; Chochlidakis, K. Buccal bone thickness of maxillary anterior teeth: A systematic review and meta-analysis. J. Clin. Periodontol. 2020, 47, 1326–1343.
- Araújo, M.G.; Silva, C.O.; Misawa, M.; Sukekava, F. Alveolar socket healing: What can we learn? Periodontol. 2000 2015, 68, 122–134.
- Avila-Ortiz, G.; Chambrone, L.; Vignoletti, F. Effect of alveolar ridge preservation interventions following tooth extraction: A systematic review and meta-analysis. J. Clin. Periodontol. 2019, 46 (Suppl. S21), 195–223.
- Cordaro, L.; Amadé, D.S.; Cordaro, M. Clinical results of alveolar ridge augmentation with mandibular block bone grafts in partially edentulous patients prior to implant placement. Clin. Oral Implant. Res. 2002, 13, 103–111.
- Clavero, J.; Lundgren, S. Ramus or chin grafts for maxillary sinus inlay and local onlay augmentation: Comparison of donor site morbidity and complications. Clin. Implant. Dent. Relat. Res. 2003, 5, 154–160.
- Block, M.S.; Baughman, D.G. Reconstruction of severe anterior maxillary defects using distraction osteogenesis, bone grafts, and implants. J. Oral. Maxillofac. Surg. 2005, 63, 291–297.
- von Arx, T.; Buser, D. Horizontal ridge augmentation using autogenous block grafts and the guided bone regeneration technique with collagen membranes: A clinical study with 42 patients. Clin. Oral Implant. Res. 2006, 17, 359–366.
- Spin-Neto, R.; Stavropoulos, A.; Dias Pereira, L.A.; Marcantonio, E., Jr.; Wenzel, A. Fate of autologous and fresh-frozen allogeneic block bone grafts used for ridge augmentation. A CBCT-based analysis. Clin. Oral Implant. Res. 2013, 24, 167–173.
- Mangano, F.G.; Zecca, P.; Luongo, F.; Iezzi, G.; Mangano, C. Single-tooth morse taper connection implant placed in grafted site of the anterior maxilla: Clinical and radiographic evaluation. Case Rep. Dent. 2014, 2014, 183872.
- Sakkas, A.; Wilde, F.; Heufelder, M.; Winter, K.; Schramm, A. Autogenous bone grafts in oral implantology-is it still a “gold standard”? A consecutive review of 279 patients with 456 clinical procedures. Int. J. Implant. Dent. 2017, 3, 23.
- Yun, K.I.; Choi, H.; Wright, R.F.; Ahn, H.S.; Chang, B.M.; Kim, H.J. Efficacy of Alveolar Vertical Distraction Osteogenesis and Autogenous Bone Grafting for Dental Implants: Systematic Review and Meta-Analysis. Int. J. Oral Maxillofac. Implant. 2016, 31, 26–36.
- Zhao, K.; Wang, F.; Huang, W.; Wu, Y. Clinical Outcomes of Vertical Distraction Osteogenesis for Dental Implantation: A Systematic Review and Meta-Analysis. Int. J. Oral Maxillofac. Implant. 2018, 33, 549–564.
- Verdonck, H.W.; Meijer, G.J.; Laurin, T.; Nieman, F.H.; Stoll, C.; Riediger, D.; Stoelinga, P.J.; de Baat, C. Assessment of vascularity in irradiated and nonirradiated maxillary and mandibular minipig alveolar bone using laser doppler flowmetry. Int. J. Oral Maxillofac. Implant. 2007, 22, 774–778.
- Koga, D.H.; Salvajoli, J.V.; Alves, F.A. Dental extractions and radiotherapy in head and neck oncology: Review of the literature. Oral Dis. 2008, 14, 40–44.
- Bienz, S.P.; Pirc, M.; Papageorgiou, S.N.; Jung, R.E.; Thoma, D.S. The influence of thin as compared to thick peri-implant soft tissues on aesthetic outcomes: A systematic review and meta-analysis. Clin. Oral Implant. Res. 2022, 33 (Suppl. S23), 56–71.
- Hosseini, M.; Worsaae, N.; Gotfredsen, K. Tissue changes at implant sites in the anterior maxilla with and without connective tissue grafting: A five-year prospective study. Clin. Oral Implant. Res. 2020, 31, 18–28.
- Starch-Jensen, T.; Aludden, H.; Hallman, M.; Dahlin, C.; Christensen, A.E.; Mordenfeld, A. A systematic review and meta-analysis of long-term studies (five or more years) assessing maxillary sinus floor augmentation. Int. J. Oral Maxillofac. Surg. 2018, 47, 103–116.
- Esposito, M.; Grusovin, M.G.; Rees, J.; Karasoulos, D.; Felice, P.; Alissa, R.; Worthington, H.; Coulthard, P. Effectiveness of sinus lift procedures for dental implant rehabilitation: A Cochrane systematic review. Eur. J. Oral Implantol. 2010, 3, 7–26.
- Raghoebar, G.M.; Onclin, P.; Boven, G.C.; Vissink, A.; Meijer, H.J.A. Long-term effectiveness of maxillary sinus floor augmentation: A systematic review and meta-analysis. J. Clin. Periodontol. 2019, 46 (Suppl. S21), 307–318.
- Antonoglou, G.N.; Stavropoulos, A.; Samara, M.D.; Ioannidis, A.; Benic, G.I.; Papageorgiou, S.N.; Sándor, G.K. Clinical Performance of Dental Implants Following Sinus Floor Augmentation: A Systematic Review and Meta-Analysis of Clinical Trials with at Least 3 Years of Follow-up. Int. J. Oral Maxillofac. Implant. 2018, 33, e45–e65.
- Danesh-Sani, S.A.; Engebretson, S.P.; Janal, M.N. Histomorphometric results of different grafting materials and effect of healing time on bone maturation after sinus floor augmentation: A systematic review and meta-analysis. J. Periodontal Res. 2017, 52, 301–312.
- Corbella, S.; Taschieri, S.; Weinstein, R.; Del Fabbro, M. Histomorphometric outcomes after lateral sinus floor elevation procedure: A systematic review of the literature and meta-analysis. Clin. Oral Implant. Res. 2016, 27, 1106–1122.
- Cordaro, L.; Torsello, F.; Miuccio, M.T.; di Torresanto, V.M.; Eliopoulos, D. Mandibular bone harvesting for alveolar reconstruction and implant placement: Subjective and objective cross-sectional evaluation of donor and recipient site up to 4 years. Clin. Oral Implant. Res. 2011, 22, 1320–1326.
- Jensen, T.; Schou, S.; Svendsen, P.A.; Forman, J.L.; Gundersen, H.J.; Terheyden, H.; Holmstrup, P. Volumetric changes of the graft after maxillary sinus floor augmentation with Bio-Oss and autogenous bone in different ratios: A radiographic study in minipigs. Clin. Oral Implant. Res. 2012, 23, 902–910.
- Cosso, M.G.; de Brito, R.B., Jr.; Piattelli, A.; Shibli, J.A.; Zenóbio, E.G. Volumetric dimensional changes of autogenous bone and the mixture of hydroxyapatite and autogenous bone graft in humans maxillary sinus augmentation. A multislice tomographic study. Clin. Oral Implant. Res. 2014, 25, 1251–1256.
- Shanbhag, S.; Shanbhag, V.; Stavropoulos, A. Volume changes of maxillary sinus augmentations over time: A systematic review. Int. J. Oral Maxillofac. Implant. 2014, 29, 881–892.
- Terheyden, H. Augmentation Surgery; Quintessence: Berlin, Germany, 2022.
- Troeltzsch, M.; Troeltzsch, M.; Kauffmann, P.; Gruber, R.; Brockmeyer, P.; Moser, N.; Rau, A.; Schliephake, H. Clinical efficacy of grafting materials in alveolar ridge augmentation: A systematic review. J. Craniomaxillofac. Surg. 2016, 44, 1618–1629.
- Christensen, J.G.; Grønlund, G.P.; Georgi, S.R.; Starch-Jensen, T.; Bruun, N.H.; Jensen, S.S. Horizontal Alveolar Ridge Augmentation with Xenogenic Block Grafts Compared with Autogenous Bone Block Grafts for Implant-retained Rehabilitation: A Systematic Review and Meta-Analysis. J. Oral Maxillofac. Res. 2023, 14, e1.
- Geng, Y.M.; Zhou, M.; Parvini, P.; Scarlat, S.; Naujokat, H.; Abraha, S.M.; Terheyden, H. Sandwich osteotomy in atrophic mandibles: A retrospective study with a 2- to 144-month follow-up. Clin. Oral Implant. Res. 2019, 30, 1027–1037.
More
Information
Subjects:
Dentistry, Oral Surgery & Medicine
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.0K
Revisions:
2 times
(View History)
Update Date:
19 Jan 2024
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




