Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | xuanxuan he | -- | 1500 | 2023-12-20 12:33:33 | | | |
| 2 | Catherine Yang | Meta information modification | 1500 | 2023-12-21 01:47:27 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
He, X.; Jin, S.; Dai, X.; Chen, L.; Xiang, L.; Zhang, C. Visible Light as a Therapeutic Option for Pigmentary Disorders. Encyclopedia. Available online: https://encyclopedia.pub/entry/52980 (accessed on 07 February 2026).
He X, Jin S, Dai X, Chen L, Xiang L, Zhang C. Visible Light as a Therapeutic Option for Pigmentary Disorders. Encyclopedia. Available at: https://encyclopedia.pub/entry/52980. Accessed February 07, 2026.
He, Xuanxuan, Shanglin Jin, Xiaoxi Dai, Li Chen, Leihong Xiang, Chengfeng Zhang. "Visible Light as a Therapeutic Option for Pigmentary Disorders" Encyclopedia, https://encyclopedia.pub/entry/52980 (accessed February 07, 2026).
He, X., Jin, S., Dai, X., Chen, L., Xiang, L., & Zhang, C. (2023, December 20). Visible Light as a Therapeutic Option for Pigmentary Disorders. In Encyclopedia. https://encyclopedia.pub/entry/52980
He, Xuanxuan, et al. "Visible Light as a Therapeutic Option for Pigmentary Disorders." Encyclopedia. Web. 20 December, 2023.
Copy Citation
Visible-light therapy (VLT) is commonly used for various skin diseases, mostly as a second-line option. Likewise, it plays a primary or adjunctive role in the clinical management of pigmentary disorders. In the treatment of pigmentary disorders, there are three primary types of visible-light therapies utilized: laser, intense pulsed light (IPL), and LED therapy. Each type of light has unique features and mechanisms that cater to different skin conditions and disorders.
visible light
pigmentary disorders
laser
LEDs
IPL
1. Laser-Emitting Lights in the Visible Range
Visible lasers are a class of laser devices that emit light in the visible-spectrum region, containing pulsed dye laser (PDL), copper vapor laser, potassium titanyl phosphate laser (KTP), helium-neon (He-Ne), ruby laser, argon laser and krypton laser [1]. As a coherent light, laser has the advantages of high intensity, low divergence, and precise control over the amount and location of skin heating [2], which makes it an ideal method for treating skin diseases based on the principle of selective photothermalmolysis [3].
While PDL was initially designed for cutaneous vascular disorders, recent studies have shown that 595 nm and 607 nm PDL can also be used to treat benign epidermal pigmented lesions (EPLs) [4][5][6][7][8][9][10]. And 585 nm and 595 nm PDL have also been found to be effective in improving melasma lesions that exhibit increased vascularity, with or without the combination of other therapies [11][12][13].
Another type of laser that is highly specific for vascular lesions is copper vapor laser, emitting a dual wavelength comprising 10% 511 nm and 90% 578 nm, which is at the proximity of the absorption peak of hemoglobin [14]. Nonetheless, the dual-wavelength copper vapor laser shows great efficacy in eliminating congenital melanocytic nevi (CMN) [15], yet demonstrates less efficacy in treating melasma patients [14][16], except for those with pronounced vascular abnormality [17].
The KTP laser, also known as the (Q-switched) Nd:YAG double-frequency 532 nm laser, is another type of laser that has been proved effective in treating EPLs, such as ephelides or solar lentigines [18][19][20][21], physiological lip hyperpigmentation (PLH) [22][23], and even tattoos [24][25]. When combined with IPL, it has been successful in treating postoperative inflammatory hyperpigmentation [21].
The 633 nm He-Ne laser emitting red light is a popular choice for low-level light therapy (LLLT), and has been found to be effective for vitiligo. Yu et al. discovered that low-energy He-Ne lasers (632.8 nm) enhance melanocyte migration and proliferation, and even rescue damaged melanocytes, creating a positive microenvironment for repigmentation [26]. The same group also investigated the molecular mechanism and biological effects of the low-energy He-Ne laser on pigment cells at different maturation stages. They found that the laser induced differentiation and mitochondrial biogenesis of primitive pigment cells through calcium-dependent mitochondrial retrograde signaling [27], as well as stimulating the differentiation of immature melanoblasts through enhanced pp125FAK expression and the melanogenesis of more mature melanoblasts [28]. Furthermore, they explored the role of the low-energy He-Ne laser in melanocytes, and demonstrated enhanced functional melanocyte proliferation via increased expression of ɑ2β1 integrin and increased attachment to collagen IV [29]. These studies provide a solid theoretical basis for understanding how low-level laser therapy induces repigmentation in vitiligo. Clinical evidence also supports the application the of low-energy He–Ne laser in treating segmental-type vitiligo, with an effectiveness comparable to conventional therapies [26].
Interestingly, red light can also be used as an effective and safe modality for further depigmentation of vitiligo. The cosmetically disturbing remnants of normal pigmentation in patients with vitiligo whose skin has been almost depigmented on the whole can be removed by the Q-switched 694 nm Ruby laser (QSRL) [30]. The QSRL is particularly effective for treating benign pigmented diseases, such as tattoos, nevus of Ota and ephelides, due to its high absorption by melanin [31][32][33][34][35][36]. While QSRL was previously believed to be ineffective in treating melasma [37], recent studies with small sample sizes have demonstrated its efficacy [38][39][40]. Similarly, the Q-switched 755 nm Alexandrite laser (QSAL) can also be used to treat a variety of superficial and deep hyperpigmented diseases such as nevus of Ota/Ito, tattoos, café au lait macules and melasma [35][41][42][43]. QSRL and QSAL are considered the best choices as phototherapy for treating dermal pigmented lesions by Bogdan et al. [8]. Yet the newly developed picosecond laser with higher efficiency in pigment removal and less thermal damage is worthy of consideration [44][45].
Taken together, the visible laser can attenuate or eliminate hyperpigmentation to a certain extent, except for the He-Ne laser, which is usually used for depigmentation. Among them, the PDL and copper vapor laser are classic modalities for vascular lesions, with recently discovered use in benign EPLs and melasma with a vascular component. KTP can tackle both epidermal and dermal hyperpigmentation, with a better effect on the former. QSRL and QSAL are best applied in dermal hyperpigmentation, but also have solid efficacy on EPLs, with new findings relating to melasma treatment that may renew the conventional views.
2. Intense Pulsed Light (IPL)
IPL is a polychromatic and noncoherent light released by a high-energy tritium flashlamp under high voltage, featuring high intensity, a relatively concentrated wavelength, and a wide and tunable pulse width. The IPL spectrum primarily falls in the range of 500–1200 nm, and can be selectively filtered by filters based on the skin type and lesions. IPL also works based on the principles of selective photothermalmolysis effects, as does laser [46]. Clinical studies have demonstrated that IPL is capable of effectively decreasing melanin production and accumulation at the cellular level, making it a suitable treatment option for various types of hyperpigmented skin conditions [47].
IPL has been proven effective in treating lentigines, ephelides, poikiloderma of Civatte and other epidermal hyperpigmentation, as well as benign melanocytic nevi such as Becker’s nevus [4][48][49][50][51][52][53]. However, it should be noted that the Q-switched laser still remains the preferred choice in light therapy for treating benign pigmented lesions. Furthermore, IPL is not a viable solution for tattoo removal, as it lacks the ability to perform Q-switching in incoherent light sources [54].
In the treatment of melasma, IPL has demonstrated superior efficacy when compared to laser treatment. In a split-face comparative study conducted by Hassan et al., IPL was observed to more effectively lighten epidermal melasma and melasma lesions with vascular alteration, in comparison to PDL [12]. Li et al. also demonstrated that IPL was ideal for melasma treatment with minimal and acceptable adverse events [55], which is consistence with Yi’s conclusion [56]. In addition to skin brightening, IPL has been popularly employed for skin rejuvenation, owing to its remarkable efficacy in addressing photoaging concerns [57].
3. Light-Emitting Diodes (LEDs)
LEDs emit incoherent light with a narrow spectrum and low intensity, which induces a mild effect on cells for regulating biological activity, rather than a thermal or exfoliative effect. This process is referred to as photomodulation or photobiomodulation (PBM), also known as LLLT [58]. A vast array of LED semiconductor materials has been available at lower wavelengths, and research over the past decade suggests that LED therapy is more suitable than laser therapy for LLLT, due to its mild output and convenient accessibility [59]. LED therapy using VL for pigmentary disorders has been a controversial approach, but recent studies have shed light on its potential application in melasma (Figure 1).
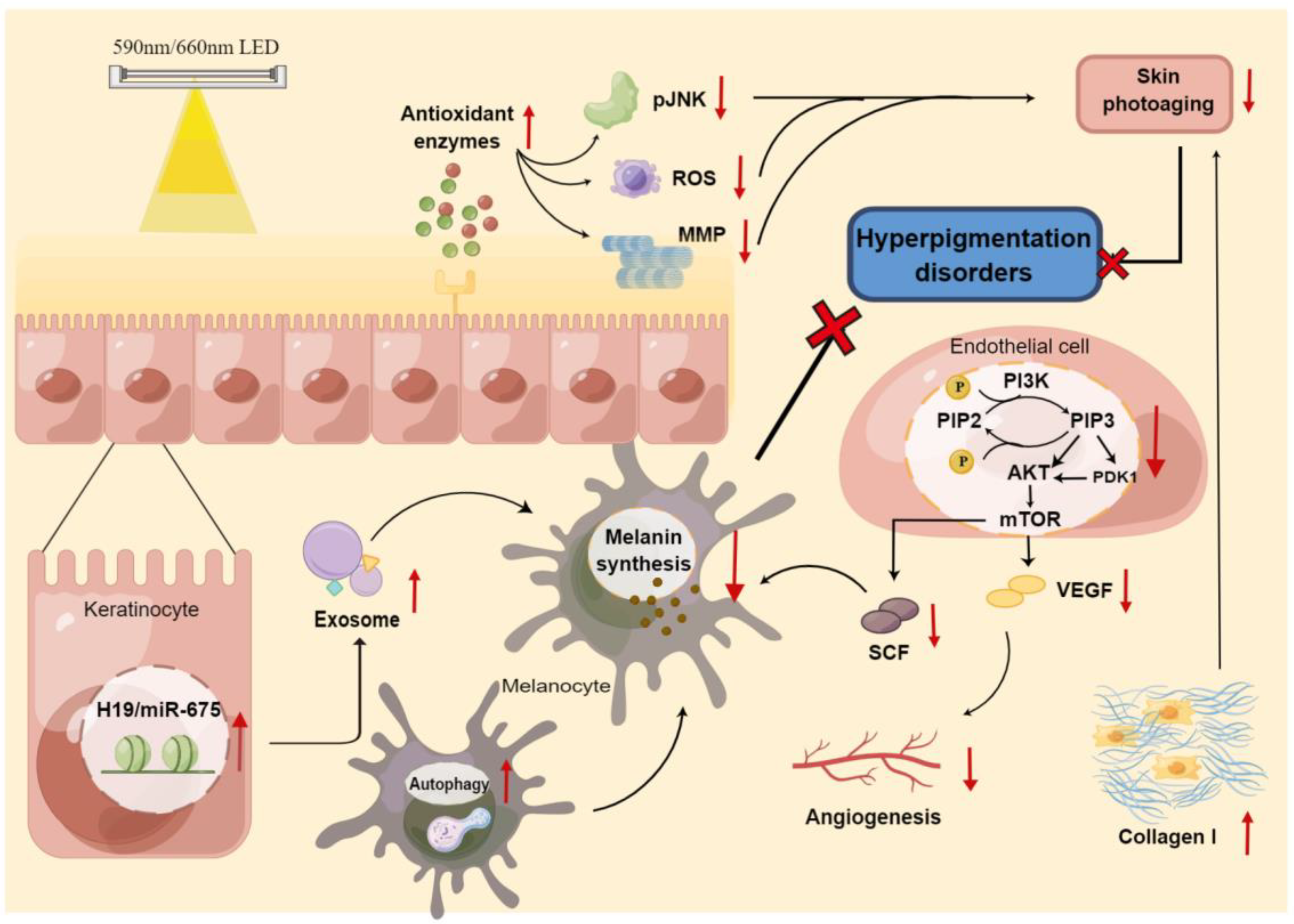
Figure 1. The mechanism of LED phototherapy for hyperpigmentation disorders.
As previously mentioned, 585 nm yellow LED light has been showed to inhibit melanogenesis in melanocytes by the inducing of autophagy [60]. This series of experimental data is consistent with Mpofana’s study, in which 633 nm-LED combined with 830 nm-LED exposure significantly ameliorated melasma in patients with skin types V and VI [61].
From another point of view, phototherapy using LED to treat skin photoaging is increasingly prevalent. Lee et al. conducted a prospective split-face clinical study on LED phototherapy for skin rejuvenation, and indicated an altered enzymatic activity related to dermal matrix remodeling, as well as a reduction in melanin content after irradiation with 633 nm red LED [62]. Moreover, 590 nm-LED or 660 nm-LED therapy increased collagen and decreased MMP-1 activity in the dermis, with pigmentation reduction [63][64][65][66], suggesting a novel perspective for LED therapy to tackle melasma, which is now defined as a photoaging disorder [67].
While yellow and red LEDs are promising for treating disorders of hyperpigmentation, LED blue light has been applied for vitiligo repigmentation. Research indicates that blue LED, combined with Buddleja officinalis, can be used to treat vitiligo through induced melanin production by promoting melanogenic signaling, in addition to CREB/MITF/TYR pathways [68]. A retrospective study also demonstrated that 417 nm blue LED induced repigmentation in 30 patients with localized vitiligo, of varying ages and different skin types [69]. Despite the relatively small sample, these results encouraged the utilization of LED on melanin-deficiency skin diseases.
Of note, LED treatments have the special advantages of high safety and convenience with fewer side effects, yet well-designed studies with larger sample sizes and repeated measures of response are sorely lacking and highly required.
LED can be applied in disorders of hyperpigmentation treatment by directly affecting melanin production through various pathways or by alleviating the photoaging process, including antioxidant enzyme and collagen I production. Red cross refers to inhibition; Red arrows refer to upregulation or downregulation. ROS, reactive oxygen species; MMP, matrix metalloproteinase; PIP, phosphatidylinositol phosphate; PI3K, phosphatidylinositol 3-kinase; mTOR, mammalian target of rapamycin; SCF, stem cell factor; VEGF, vascular endothelial growth factor; By figdraw.
References
- Avci, P.; Gupta, A.; Sadasivam, M.; Vecchio, D.; Pam, Z.; Pam, N.; Hamblin, M.R. Low-level laser (light) therapy (LLLT) in skin: Stimulating, healing, restoring. Semin. Cutan. Med. Surg. 2013, 32, 41–52.
- Ross, E.V. Laser versus intense pulsed light: Competing technologies in dermatology. Lasers Surg. Med. 2006, 38, 261–272.
- Anderson, R.R.; Parrish, J.A. Selective photothermolysis: Precise microsurgery by selective absorption of pulsed radiation. Science 1983, 4569, 524–527.
- Galeckas, K.J.; Collins, M.; Ross, E.V.; Uebelhoer, N.S. Split-face treatment of facial dyschromia: Pulsed dye laser with a compression handpiece versus intense pulsed light. Dermatol. Surg. 2008, 34, 672–680.
- Chern, P.L.; Domankevitz, Y.; Ross, E.V. Pulsed dye laser treatment of pigmented lesions: A randomized clinical pilot study comparison of 607- and 595-nm wavelength lasers. Lasers Surg. Med. 2010, 42, 865–869.
- Fateh, S.; Farnaghi, F.; Ehsani, A.H.; Noormohammadpour, P.; Seirafi, H. Efficacy and safety of long-pulse pulsed dye laser delivered with compression versus cryotherapy for treatment of solar lentigines. Indian J. Dermatol. 2011, 56, 48–51.
- Ghaninejhadi, H.; Ehsani, A.; Edrisi, L.; Gholamali, F.; Akbari, Z.; Noormohammadpour, P. Solar Lentigines: Evaluating Pulsed Dye Laser (PDL) as an Effective Treatment Option. J. Lasers Med. Sci. 2013, 4, 33–38.
- Allemanna, I.B.; Goldberg, D.J. (Eds.) Benign Pigmented Lesions. In Basics in Dermatological Laser Applications; Part of: Current Problems in Dermatology; S. Karger Publishing: Basel, Switzerland, 2011; pp. 81–96.
- Abd El-Naby, N.; Mostafa Ali, M.; Hawwam, S.A.; Sarhan, N. The clinical and electron microscopic evaluation of the impact of pulsed dye laser techniques on solar lentigines (randomized clinical trial). J. Dermatolog. Treat. 2022, 33, 361–368.
- Labadie, J.G.; Krunic, A.L. Long pulsed dye laser with a back-to-back double-pulse technique and compression for the treatment of epidermal pigmented lesions. Lasers Surg. Med. 2019, 51, 136–140.
- Geddes, E.R.; Stout, A.B.; Friedman, P.M. Retrospective analysis of the treatment of melasma lesions exhibiting increased vascularity with the 595-nm pulsed dye laser combined with the 1927-nm fractional low-powered diode laser. Lasers Surg. Med. 2017, 49, 20–26.
- Hassan, A.M.; Elfar, N.N.; Rizk, O.M.; Eissa, N.Y. Pulsed dye laser versus intense pulsed light in melasma: A split-face comparative study. J. Dermatolog. Treat. 2018, 29, 725–732.
- Kong, S.H.; Suh, H.S.; Choi, Y.S. Treatment of Melasma with Pulsed-Dye Laser and 1,064-nm Q-Switched Nd:YAG Laser: A Split-Face Study. Ann. Dermatol. 2018, 30, 1.
- Ghorbel, H.H.; Boukari, F.; Fontas, E.; Montaudié, H.; Bahadoran, P.; Lacour, J.P.; Passeron, T. Copper Bromide Laser vs Triple-Combination Cream for the Treatment of Melasma: A Randomized Clinical Trial. JAMA Dermatol. 2015, 151, 791–792.
- Ponomarev, I.V.; Topchiy, S.B.; Pushkareva, A.E.; Klyuchareva, S.V.; Andrusenko, Y.N. Treatment of Congenital Melanocytic Nevi With a Dual-Wavelengths Copper Vapor Laser: A Case Series. J. Lasers Med. Sci. 2021, 12, e5.
- Eimpunth, S.; Wanitphakdeedecha, R.; Triwongwaranat, D.; Varothai, S.; Manuskiatti, W. Therapeutic outcome of melasma treatment by dual-wavelength (511 and 578 nm) laser in patients with skin phototypes III-V. Clin. Exp. Dermatol. 2014, 39, 292–297.
- Lee, H.I.; Lim, Y.Y.; Kim, B.J.; Kim, M.N.; Min, H.J.; Hwang, J.H.; Song, K.Y. Clinicopathologic efficacy of copper bromide plus/yellow laser (578 nm with 511 nm) for treatment of melasma in Asian patients. Dermatol. Surg. 2010, 36, 885–893.
- Guss, L.; Goldman, M.P.; Wu, D.C. Picosecond 532 nm Neodymium-Doped Yttrium Aluminium Garnet Laser for the Treatment of Solar Lentigines in Darker Skin Types: Safety and Efficacy. Dermatol. Surg. 2017, 43, 456–459.
- Negishi, K.; Akita, H.; Matsunaga, Y. Prospective study of removing solar lentigines in Asians using a novel dual-wavelength and dual-pulse width picosecond laser. Lasers Surg. Med. 2018, 50, 851–858.
- Vachiramon, V.; Iamsumang, W.; Triyangkulsri, K. Q-switched double frequency Nd:YAG 532-nm nanosecond laser vs. double frequency Nd:YAG 532-nm picosecond laser for the treatment of solar lentigines in Asians. Lasers Med. Sci. 2018, 33, 1941–1947.
- Hom, D.B.; Ingraffea, A. Efficacy of Q-switched Nd:YAG Frequency Doubling 532nm Laser Combined with Photorejuvenation on Freckles. Med. Aesthet. Beauty 2020, 21, 41–45.
- Kerkar, S.; Shilpa, K.; Revathi, T.N. Efficacy of 532-nm Q-switched Nd:YAG Laser in the Treatment of Lip Melanosis. J. Cutan. Aesthet. Surg. 2021, 14, 203–207.
- Altalhab, S.; Aljamal, M.; Mubki, T.; AlNomair, N.; Algoblan, S.; Alalola, A.; Alissa, I.; Alissa, A. Q-switched 532 nm Nd:YAG laser therapy for physiological lip hyperpigmentation: Novel classification, efficacy, and safety. J. Dermatol. Treat. 2022, 33, 1324–1328.
- Alabdulrazzaq, H.; Brauer, J.A.; Bae, Y.-S.; Geronemus, R.G. Clearance of yellow tattoo ink with a novel 532-nm picosecond laser. Lasers Surg. Med. 2015, 47, 285–288.
- Bernstein, E.F.; Schomacker, K.T.; Basilavecchio, L.D.; Plugis, J.M.; Bhawalkar, J.D. A novel dual-wavelength, Nd:YAG, picosecond-domain laser safely and effectively removes multicolor tattoos. Lasers Surg. Med. 2015, 47, 542–548.
- Yu, H.-S.; Wu, C.-S.; Kao, Y.-H.; Chiou, M.-H.; Yu, C.-L. Helium-neon laser irradiation stimulates migration and proliferation in melanocytes and induces repigmentation in segmental-type vitiligo. J. Investig. Dermatol. 2003, 120, 56–64.
- Lan, C.-C.E.; Wu, S.-B.; Wu, C.-S.; Shen, Y.-C.; Chiang, T.-Y.; Wei, Y.-H.; Yu, H.-S. Induction of primitive pigment cell differentiation by visible light (helium–neon laser): A photoacceptor-specific response not replicable by UVB irradiation. J. Mol. Med. 2012, 90, 321–330.
- Lan, C.C.; Wu, C.S.; Chiou, M.H.; Hsieh, P.C.; Yu, H.S. Low-energy helium-neon laser induces locomotion of the immature melanoblasts and promotes melano genesis of the more differentiated melanoblasts: Recapitulation of vitiligo repigmentation in vitro. J. Investig. Dermatol. 2006, 126, 2119–2126.
- Lan, C.-C.; Wu, C.-S.; Chiou, M.-H.; Chiang, T.-Y.; Yu, H.-S. Low-energy helium—Neon laser induces melanocyte proliferation via interaction with type IV collagen: Visible light as a therapeutic option for vitiligo. Br. J. Dermatol. 2009, 2, 273–280.
- Boen, M.; Wilson, M.J.V.; Wu, D.C.; Goldman, M.P. Laser_Depigmentation_in_Extensive_Vitiligo.26. Dermatol. Surg. 2019, 4, 621–623.
- Taylor, C.R.; Anderson, R.R. Treatment of Benign Pigmented Epidermal Lesions by Q-Switched Ruby Laser. Int. J. Dermatol. 1993, 32, 908–912.
- Taylor, C.R.; Flotte, T.J.; Gange, R.W.; Anderson, R.R. Treatment of nevus of Ota by Q-switched ruby laser. J. Am. Acad. Dermatol. 1994, 30 Pt 1, 743–751.
- Watanabe, S.; Takahashi, H. Treatment of nevus of ota with the q-switched rubylaser. N. Engl. J. Med. 1994, 26, 1745–1750.
- Rathod, S.; Munshi, A.; Agarwal, J. Skin markings methods and guidelines: A reality in image guidance radiotherapy era. South Asian J. Cancer 2020, 1, 27–29.
- Ma, S.-Y.; Gong, Y.-Q.; Zhang, W.J.; Liang, B.-H.; Li, Y.-M.; Xie, Z.-M.; Zhu, H.-L. Split-face comparison of the efficacy of picosecond 532 nm Nd:YAG laser and Q-switched 755 nm Alexandrite laser for treatment of freckles. J. Cosmet. Laser Ther. 2022, 24, 22–27.
- Yamada-Kanazawa, S.; Jinnin, M.; Fukushima, S. Nevus of Ota on the auricle successfully treated with Q-switched ruby laser. Drug Discov. Ther. 2022, 16, 254–255.
- Taylor, C.R.; Anderson, R.R. Ineffective treatment of refractory melasma and postinflammatory hyperpigmentation by Q-switched ruby laser. J. Dermatol. Surg. Oncol. 1994, 20, 592–597.
- Jang, W.S.; Lee, C.K.; Kim, B.J.; Kim, M.N. Efficacy of 694-nm Q-Switched Ruby Fractional Laser Treatment of Melasma in Female Korean Patients. Dermatol. Surg. 2011, 37, 1133–1140.
- Hilton, S.; Heise, H.; Buhren, B.A.; Schrumpf, H.; Bölke, E.; Gerber, P.A. Treatment of melasma in Caucasian patients using a novel 694-nm Q-switched ruby fractional laser. Eur. J. Med. Res. 2013, 18, 43.
- Zhou, H.L.; Hu, B.; Zhang, C. Efficacy of 694-nm fractional Q-switched ruby laser (QSRL) combined with sonophoresis on levorotatory vitamin C for treatment of melasma in Chinese patients. Lasers Med. Sci. 2016, 31, 991–995.
- Li, Y.; Tong, X.; Yang, J.; Yang, L.; Tao, J.; Tu, Y. Q-switched alexandrite laser treatment of facial and labial lentigines associated with Peutz-Jeghers syndrome. Photodermatol. Photoimmunol. Photomed. 2012, 28, 196–199.
- Wattanakrai, P.; Mornchan, R.; Eimpunth, S. A randomized, split-face clinical trial of low-fluence Q-switched neodymium-doped yttrium aluminum garnet (1064 nm) laser versus low-fluence Q-switched alexandrite laser (755 nm) for the treatment of facial melasma. Lasers Surg. Med. 2014, 46, 531–537.
- Zhang, B.; Chu, Y.; Xu, Z.; Sun, Y.; Li, L.; Han, X.; Wang, C.; Wei, L.; Liu, Y.; Ma, L. Treatment of Café-Au-Lait Spots Using Q-Switched Alexandrite Laser: Analysis of Clinical Characteristics of 471 Children in Mainland China. Lasers Surg. Med. 2019, 51, 694–700.
- Manuskiatti, W.; Yan, C.; Tantrapornpong, P.; Cembrano, K.A.; Techapichetvanich, T.; Wanitphakdeedecha, R. A Prospective, Split-Face, Randomized Study Comparing a 755-nm Picosecond Laser With and Without Diffractive Lens Array in the Treatment of Melasma in Asians. Lasers Surg. Med. 2021, 53, 95–103.
- Vachiramon, V.; Namasondhi, A.; Anuntrangsee, T.; Jurairattanaporn, N. Randomized, evaluator-blinded comparative study of a potassium titanyl phosphate (KTP) 532-nm picosecond laser and an alexandrite 755-nm picosecond laser for the treatment of solar lentigines in Asians. J. Cosmet. Dermatol. 2022, 21, 4370–4377.
- Raulin, C.; Greve, B.; Grema, H. IPL technology: A review. Lasers Surg. Med. 2003, 32, 78–87.
- Kim, J.; Lee, J.; Choi, H. Intense Pulsed Light Attenuates UV-Induced Hyperimmune Response and Pigmentation in Human Skin Cells. Int. J. Mol. Sci. 2021, 22, 3173.
- Bjerring, P.; Christiansen, K. Intense pulsed light source for treatment of small melanocytic nevi and solar lentigines. J. Cutan. Laser Ther. 2000, 2, 177–181.
- Kawada, A.; Shiraishi, H.; Asai, M.; Kameyama, H.; Sangen, Y.; Aragane, Y.; Tezuka, T. Clinical improvement of solar lentigines and ephelides with an intense pulsed light source. Dermatol. Surg. 2002, 28, 504–508.
- Sasaya, H.; Kawada, A.; Wada, T.; Hirao, A.; Oiso, N. Clinical effectiveness of intense pulsed light therapy for solar lentigines of the hands. Dermatol. Ther. 2011, 24, 584–586.
- Friedmann, D.P.; Peterson, J.D. Efficacy and safety of intense pulsed light with a KTP filter for the treatment of solar lentigines. Lasers Surg. Med. 2019, 51, 500–508.
- Amornpetkul, W.; Kanokrungsee, S.; Kamanamool, N.; Udompataikul, M.; Rojhirunsakool, S. Comparison between the use of intense pulsed light and Q-switched neodymium-doped yttrium aluminum garnet laser for the treatment of axillary hyperpigmentation. J. Cosmet. Dermatol. 2021, 20, 2785–2793.
- Zhong, Y.; Huang, L.; Chen, Y.; Yan, T.; Yang, B.; Man, M.Q. The efficacy of intense pulsed light for Becker’s nevus: A retrospective analysis of 45 cases. J. Cosmet. Dermatol. 2021, 20, 466–471.
- Babilas, P.; Schreml, S.; Szeimies, R.-M.; Landthaler, M. Intense pulsed light (IPL): A review. Lasers Surg. Med. 2010, 42, 93–104.
- Li, Y.H.; Chen, J.Z.; Wei, H.C.; Wu, Y.; Liu, M.; Xu, Y.Y.; Dong, G.H.; Chen, H.D. Efficacy and Safety of Intense Pulsed Light in Treatment of Melasma in Chinese Patients. Dermatol. Surg. 2008, 34, 693–701.
- Yi, J.; Hong, T.; Zeng, H.; Li, P.; Li, P.; Wang, S.; Chen, J.; Li, P.; Zhou, J. A Meta-analysis-Based Assessment of Intense Pulsed Light for Treatment of Melasma. Aesthetic Plast. Surg. 2020, 44, 947–952.
- Dierickx, C.C.; Anderson, R.R. Visible light treatment of photoaging. Dermatol. Ther. 2005, 18, 191–208.
- Weiss, R.A.; McDaniel, D.H.; Geronemus, R.G.; Margaret, A.W.; Karen, L.B.; Munavalli, G.M.; Bellew, S.G. Clinical experience with light-emitting diode (LED) photomodulation. Dermatol. Surg. 2005, 31 Pt 2, 1199–1205.
- Heiskanen, V.; Hamblin, M.R. Photobiomodulation: Lasers vs. light emitting diodes? Photochem. Photobiol. Sci. 2018, 17, 1003–1017.
- Chen, L.; Xu, Z.; Jiang, M.; Zhang, C.; Wang, X.; Xiang, L. Light-emitting diode 585nm photomodulation inhibiting melanin synthesis and inducing autophagy in human melanocytes. J. Dermatol. Sci. 2018, 89, 11–18.
- Mpofana, N.; Abrahamse, H. The Management of Melasma on Skin Types V and VI Using Light Emitting Diode Treatment. Photomed. Laser Surg. 2018, 36, 522–529.
- Lee, S.Y.; Park, K.-H.; Choi, J.-W.; Kwon, J.-K.; Lee, D.R.; Shin, M.S.; Lee, J.S.; You, C.E.; Park, M.Y. A prospective, randomized, placebo-controlled, double-blinded, and split-face clinical study on LED phototherapy for skin rejuvenation: Clinical, profilometric, histologic, ultrastructural, and biochemical evaluations and comparison of three different treatment settings. J. Photochem. Photobiol. B 2007, 88, 51–67.
- Lan CC, E.; Ho, P.Y.; Wu, C.S.; Yang, R.C.; Yu, H.S. LED 590 nm photomodulation reduces UVA-induced metalloproteinase-1 expression via upregulation of antioxidant enzyme catalase. J. Dermatol. Sci. 2015, 78, 125–132.
- Weiss, R.A.; McDaniel, D.H.; Geronemus, R.G.; Weiss, M.A. Clinical trial of a novel non-thermal LED array for reversal of photoaging: Clinical, histologic, and surface profilometric results. Lasers Surg. Med. 2005, 36, 85–91.
- Barolet, D.; Roberge, C.J.; Auger, F.A.; Boucher, A.; Germain, L. Regulation of skin collagen metabolism in vitro using a pulsed 660 nm LED light source: Clinical correlation with a single-blinded study. J. Investig. Dermatol. 2009, 129, 2751–2759.
- A Weiss, R.; A Weiss, M.; Geronemus, R.G.; McDaniel, D.H. A novel non-thermal non-ablative full panel LED photomodulation device for reversal of photoaging: Digital microscopic and clinical results in various skin types. J. Drugs Dermatol. 2004, 3, 605–610.
- Passeron, T.; Picardo, M. Melasma, a photoaging disorder. Pigment. Cell Melanoma Res. 2018, 31, 461–465.
- Cho, H.; Kim, B.; Kim, O.S.; Kim, Y.; Yang, Y.; Song, J.; Liu, D.; Jeon, S.; Kim, O. Photochemical reaction to increase melanogenesis using Buddleja officinalis and blue light-emitting diode irradiation in B16F10. Photodiagn. Photodyn. Ther. 2021, 35, 102456.
- Lodi, G.; Del Re, C.; Nisticò, S.P.; Bennardo, L.; Cannarozzo, G.; Sannino, M. Blue light-emitting diodes for the treatment of localized vitiligo: A retrospective study. J. Cosmet. Dermatol. 2023, 22, 1273–1278.
More
Information
Subjects:
Dermatology
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
864
Revisions:
2 times
(View History)
Update Date:
25 Dec 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




