Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Alessia Paganelli | -- | 1926 | 2023-11-22 16:14:32 | | | |
| 2 | Wendy Huang | Meta information modification | 1926 | 2023-11-23 12:30:43 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Paganelli, A.; Contu, L.; Condorelli, A.; Ficarelli, E.; Motolese, A.; Paganelli, R.; Motolese, A. Platelet-Rich Plasma Therapy for Lichen Sclerosus. Encyclopedia. Available online: https://encyclopedia.pub/entry/51935 (accessed on 07 February 2026).
Paganelli A, Contu L, Condorelli A, Ficarelli E, Motolese A, Paganelli R, et al. Platelet-Rich Plasma Therapy for Lichen Sclerosus. Encyclopedia. Available at: https://encyclopedia.pub/entry/51935. Accessed February 07, 2026.
Paganelli, Alessia, Luca Contu, Alessandra Condorelli, Elena Ficarelli, Alfonso Motolese, Roberto Paganelli, Alberico Motolese. "Platelet-Rich Plasma Therapy for Lichen Sclerosus" Encyclopedia, https://encyclopedia.pub/entry/51935 (accessed February 07, 2026).
Paganelli, A., Contu, L., Condorelli, A., Ficarelli, E., Motolese, A., Paganelli, R., & Motolese, A. (2023, November 22). Platelet-Rich Plasma Therapy for Lichen Sclerosus. In Encyclopedia. https://encyclopedia.pub/entry/51935
Paganelli, Alessia, et al. "Platelet-Rich Plasma Therapy for Lichen Sclerosus." Encyclopedia. Web. 22 November, 2023.
Copy Citation
Lichen sclerosus (LS) is a chronic inflammatory dermatosis mostly localized in the genital area, characterized by vulvar alterations that can severely impact a patient’s quality of life. Current treatment modalities often provide incomplete relief, and there is a need for innovative approaches to manage this condition effectively. Platelet-rich plasma (PRP) and adipose-derived stem cells (ADSCs) have emerged as potential regenerative therapies for LS, offering promising results in clinical practice.
lichen sclerosus
PRP
genital
skin
autoimmune
therapy
1. Introduction
Lichen sclerosus (LS) is a relatively rare and often misdiagnosed dermatological condition, that primarily affects the skin in the genital and perianal region [1]. While it is not a life-threatening condition, its impact on patient quality of life and psychological well-being should not be underestimated [2]. At its core, lichen sclerosus is a chronic inflammatory skin disorder that manifests as thin, white patches on the skin’s surface. These patches, often described as looking like “cigarette paper” or “parchment”, are characterized by their smooth, shiny appearance and can appear anywhere on the body [3]. However, they most commonly affect the genital and perianal regions in both sexes, leading to considerable discomfort and distress. Although less common, lichen sclerosus can also involve extragenital areas, such as the breasts, upper body, and thighs [4]. These extragenital manifestations can sometimes mimic other skin conditions, making it crucial for medical professionals to be well-versed in recognizing and differentiating lichen sclerosus. One of the hallmark symptoms of lichen sclerosus is pruritus [5]. Itching can be severe and debilitating, significantly impacting patient’s daily life [6]. Additionally, scratching can worsen skin inflammation and may result in further complications, such as fissures, bleeding, and even pain during sexual intercourse [7]. In addition to the physical symptoms, the emotional toll of LS should not be underestimated. Living with a chronic, often misunderstood condition can lead to anxiety, depression, and reduced self-esteem [8][9]. Diagnosing lichen sclerosus can be challenging, and misdiagnoses are not uncommon. Even expert dermatologists, in fact, may need to perform a biopsy to confirm this condition.
While the exact cause of lichen sclerosus remains unclear, several factors seem to contribute to its development. There is evidence to suggest that autoimmune factors may play a role, as the condition is associated with other autoimmune diseases such as thyroid disorders and vitiligo [10][11]. Hormonal imbalances are also believed to be a contributing factor, which could at least partially explain the higher prevalence of LS in postmenopausal women [12]. Genetics seem to also possibly play a role. However, further research is needed to fully understand the complex interplay of these factors in LS pathogenesis.
Topical corticosteroid creams or ointments are commonly prescribed to reduce inflammation and alleviate itching [13]. In some cases, other immunomodulatory medications may also be recommended to help manage the condition, such as topical calcineurin inhibitors or systemic immunosuppressants [14]. Despite optimal treatment, LS often poses significant challenges in terms of symptom control and management, since conventional therapies lead to limited success in a non-negligible proportion of cases. In fact, complete remission of LS-related signs and symptoms remains an unreachable goal for most of the patients. Since there is currently no availability of a definitive cure for LS, new strategies have recently been investigated; currently, LS treatment represents an expanding field of research. More specifically, platelet-rich plasma (PRP) therapy has emerged as a promising and innovative approach in the management of various dermatological conditions, and its potential benefits in treating LS are gaining increasing attention [15]. PRP therapy has generated interest for its regenerative properties and potential to alleviate the distressing symptoms associated with LS [15]. Nevertheless, adipose-tissue derived stromal cells (ADSCs) have also emerged as a novel therapeutic avenue, offering the potential not only to address the root causes of LS but also to promote tissue regeneration [16]. ADSC-based therapy is a cutting-edge and rapidly evolving field in regenerative medicine, which holds immense promise for individuals suffering from LS.
2. Platelet-Rich Plasma (PRP) Therapy
PRP is a hemoderivative rich in growth factors and cytokines, and is hypothesized to stimulate tissue regeneration and repair, making it a potential candidate for mitigating the symptoms and structural changes associated with LS [15][17].
Autologous and homologous PRP are two distinct approaches to harnessing the therapeutic potential of platelets in regenerative medicine. These techniques differ primarily in the source of the PRP and their applications. A notable advantage of autologous PRP therapy is its safety profile, as it utilizes the patient’s own blood components, minimizing the risk of adverse reactions or immune responses [18]. This type of PRP is already commonly used not only in dermatology but also in orthopedics and sports medicine with the aim of accelerating healing, reducing pain, and promoting tissue repair [19]. In contrast, homologous PRP is obtained from donor’s blood. This approach is less common and typically involves a careful screening process to ensure donor safety and compatibility. The use of homologous PRP is currently limited to specialized research settings but has been demonstrated to offer some advantages in terms of efficacy when compared to autologous PRP [20]. However, evidence on homologous PRP is currently limited to other research contexts since no clinical studies have been published so far on the use of homologous PRP in the setting of LS.
As previously mentioned, the therapeutic potential of PRP (either autologous or homologous) is closely related to their content rich in platelets [21][22]. Platelets release growth factors that stimulate cell proliferation and tissue regeneration, making PRP an attractive option for a variety of medical conditions (see Figure 1) [23].
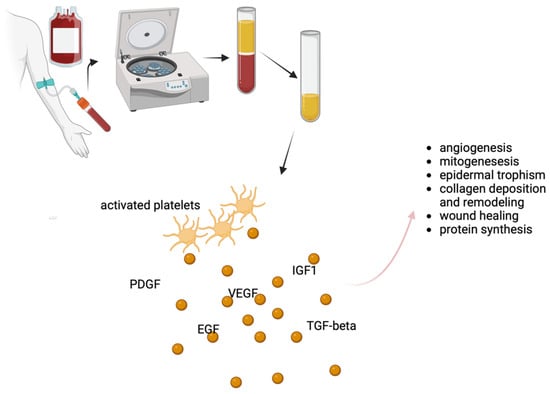
Figure 1. Schematic representation of the use of PRP in the setting of LS and possible mechanisms of action. PRP is obtained through centrifugation of blood and its content is particularly rich in platelets. When injected, activated platelets release a series of growth factors responsible for their therapeutic efficacy. PDGF: platelet-derived growth factor; EGF: epidermal growth factor; VEGF: vascular endothelial growth factor; IGF: insulin-like growth factor; TGF: transforming growth factor. Created with BioRender.com, accessed on 14 October 2023.
With regards to LS, early investigations have reported encouraging results, particularly in terms of symptom relief. PRP therapy has shown the potential to reduce itching, pain, and discomfort, which are hallmark symptoms of lichen sclerosus [16]. Furthermore, PRP’s regenerative capacity appears to have a positive impact on the structural changes associated with LS [24]. Preliminary studies suggest that PRP may promote the restoration of normal tissue architecture, potentially reducing the risk of scarring and fibrosis [25]. This is a significant consideration, as fibrotic changes can lead to structural alterations, further complicating the management of lichen sclerosus. Moreover, PRP’s anti-inflammatory properties may contribute to alleviating the chronic inflammation characteristic of the condition. An Australian study, for example, followed up for two years with 28 patients with confirmed vulvar LS were treated with autologous PRP [26]. All the patients were non-responders to topical steroid treatment. The results showed that almost all patients experienced clinical improvement in the size of their LS lesions. In eight cases, the lesions completely disappeared, and 23 out of the 28 patients eliminated the need for further steroid therapy, with complete remission of LS-related symptoms in 15 cases and significant improvement in the rest of the study population. Recently, symptomatic relief after platelet-rich plasma infiltration in vulvar LS was also described [27] by a Spanish group. Medina Garrido and collaborators performed a pilot study aimed at assessing the impact of PRP injections on symptom relief in postmenopausal women with vulvar LS who had not responded well to topical corticosteroid treatment. Three PRP infiltrations were administered to 28 patients, and changes in symptom scores were monitored using the clinical scoring system for vulvar lichen sclerosus (CSS) over the course of a year. The results revealed that women in the study experienced statistically significant improvements in self-assessed LS symptoms, and these improvements were sustained throughout the year of monitoring.
Several authors also focused on histological changes induced by PRP. Goldstein and collaborators, in fact, performed a randomized double-blind placebo-controlled trial to evaluate the safety and the efficacy of PRP in vulvar LS and chose the grade of inflammation in post-treatment biopsy as a primary endpoint [28][29]. Despite the study succeeding in demonstrating higher effectiveness of PRP compared to saline injection, histological improvement in terms of inflammatory infiltrates was demonstrated only in 5 out of 19 treated women. The group of Tedesco et al. followed up 31 patients (13 males, 18 females) for 12 months after a 3-session treatment with autologous PRP injected into affected areas [30]. All the cases of PRP were confirmed through biopsy. Possible comorbidities included psoriasis, esophagitis, lichen planus, myasthenia gravis, Hashimoto’s disease, and atrophic gastritis. After one year, nearly two thirds of the patients showed symptom improvement and stabilization of the disease were achieved in around one third of cases; only one subject experienced disease progression. Notably, female gender was a statistically significant factor for improvement, while age and comorbidities did not show statistical significance. A case report from Franic et al. also documented histological improvement after two injections of autologous PRP, with restoration or the physiological dermal and epidermal architecture [31]. On the contrary, an Italian group monitored the effectiveness of PRP therapy in the treatment of vulvar LS with non-invasive methods, proposing video thermography as a suitable tool in this setting [32].
However, it is important to note that the available data on PRP’s effectiveness for genital lichen sclerosus are limited, and larger, well-designed clinical trials are needed to establish its long-term benefits and safety. Moreover, the degree of improvement can vary among individuals, and not all patients may experience the same level of relief. While much of the research on PRP therapy for lichen sclerosus has focused on female patients, there is a growing interest in its applicability for males. Preliminary studies and clinical observations in male patients have suggested that PRP therapy may offer some degree of relief from the symptoms associated with lichen sclerosus. A recent study by Casabona et al. aimed to assess the effectiveness of PRP injections in treating penile LS [25]. Forty-five male patients with penile LS received autologous PRP injections, and various factors including age at diagnosis, treatment frequency, clinical conditions, symptoms, and treatment outcomes were examined. The results demonstrated that PRP treatment led to significant improvements in clinical conditions and symptom reduction in all patients. Topical steroid therapy, which was previously used, was not resumed after PRP treatment. The Investigator’s Global Assessment (IGA) and the Dermatology Life Quality Index (DLQI) both showed substantial improvements after PRP treatment. Another prospective multicentric study evaluated the safety and effectiveness of autologous PRP treatment for LS in male subjects refractory to conventional therapy for at least six months [33]. Five patients met the inclusion criteria and underwent PRP injections every eight weeks. After 18 months, significant decrease in IGA and DLQI was observed, although visual changes were minimal. All patients reported being symptom-free at 10 months, with only one patient experiencing a complication (balanitis). Possible gender-related differences were investigated in a very recent paper from Tedesco and coauthors [34]. A total of 43 males and 51 females received PRP treatment (three infiltrations, 15 days apart) for genital LS. The PRP treatment was well-tolerated, resulting in a significant overall symptom reduction after six months. Pain and burning sensation improved significantly in both genders, with a more pronounced effect in women. Itching reduction was similar in both sexes, while dyspareunia (pain during sexual intercourse) improved significantly only in males. Taken together, these data suggest that PRP therapy may play a crucial role in managing LS by improving quality of life and sexual function for both genders, while also highlighting gender-related differences in symptom severity and age of onset. However, further research, including larger clinical trials specifically focused on male patients, are needed to determine the long-term efficacy and safety of PRP therapy in this setting.
References
- Kirtschig, G. Lichen Sclerosus-Presentation, Diagnosis and Management. Dtsch. Arztebl. Int. 2016, 113, 337–343.
- Steben, M. Lichen Sclerosus: Why Do Most Women Struggle With Their Diagnosis? J. Obstet. Gynaecol. Can. 2022, 44, 119–120.e1.
- Meffert, J.J.; Davis, B.M.; Grimwood, R.E. Lichen Sclerosus. J. Am. Acad. Dermatol. 1995, 32, 393–416; quiz 417–418.
- Arif, T.; Fatima, R.; Sami, M. Extragenital Lichen Sclerosus: A Comprehensive Review. Aust. J. Dermatol. 2022, 63, 452–462.
- Tasker, G.L.; Wojnarowska, F. Lichen Sclerosus. Clin. Exp. Dermatol. 2003, 28, 128–133.
- Ranum, A.; Pearson, D.R. The Impact of Genital Lichen Sclerosus and Lichen Planus on Quality of Life: A Review. Int. J. Womens Dermatol. 2022, 8, e042.
- Felmingham, C.; Chan, L.; Doyle, L.W.; Veysey, E. The Vulval Disease Quality of Life Index in Women with Vulval Lichen Sclerosus Correlates with Clinician and Symptom Scores. Australas. J. Dermatol. 2020, 61, 110–118.
- Vittrup, G.; Mørup, L.; Heilesen, T.; Jensen, D.; Westmark, S.; Melgaard, D. Quality of Life and Sexuality in Women with Lichen Sclerosus: A Cross-Sectional Study. Clin. Exp. Dermatol. 2022, 47, 343–350.
- Casabona, F.; Gasparini, G.; Cozzani, E.; Barbazza, A.; Casabona, F.; Carmisciano, L.; Parodi, A. Improvement in Quality of Life and Sexual Function in Patients Affected by Vulvar Lichen Sclerosus Treated with Combined Autologous Platelet-Rich Plasma and Fat Grafting. Eur. J. Dermatol. 2023, 33, 249–254.
- Khan Mohammad Beigi, P. The Immunogenetics of Morphea and Lichen Sclerosus. Adv. Exp. Med. Biol. 2022, 1367, 155–172.
- Veronesi, G.; Virdi, A.; Leuzzi, M.; Gurioli, C.; Chessa, M.A.; Guglielmo, A.; Neri, I. Vulvar Vitiligo and Lichen Sclerosus in Children: A Clinical Challenge. Pediatr. Dermatol. 2021, 38, 1012–1019.
- Pérez-López, F.R.; Vieira-Baptista, P. Lichen Sclerosus in Women: A Review. Climacteric 2017, 20, 339–347.
- Fistarol, S.K.; Itin, P.H. Diagnosis and Treatment of Lichen Sclerosus: An Update. Am. J. Clin. Dermatol. 2013, 14, 27–47.
- Kirtschig, G.; Becker, K.; Günthert, A.; Jasaitiene, D.; Cooper, S.; Chi, C.-C.; Kreuter, A.; Rall, K.K.; Aberer, W.; Riechardt, S.; et al. Evidence-Based (S3) Guideline on (Anogenital) Lichen Sclerosus. J. Eur. Acad. Dermatol. Venereol. 2015, 29, e1–e43.
- White, C.; Brahs, A.; Dorton, D.; Witfill, K. Platelet-Rich Plasma: A Comprehensive Review of Emerging Applications in Medical and Aesthetic Dermatology. J. Clin. Aesthet. Dermatol. 2021, 14, 44–57.
- Eshtiaghi, P.; Sadownik, L.A. Fact or Fiction? Adipose-Derived Stem Cells and Platelet-Rich Plasma for the Treatment of Vulvar Lichen Sclerosus. J. Low. Genit. Tract. Dis. 2019, 23, 65–70.
- Emer, J. Platelet-Rich Plasma (PRP): Current Applications in Dermatology. Skin Ther. Lett. 2019, 24, 1–6.
- Leo, M.S.; Kumar, A.S.; Kirit, R.; Konathan, R.; Sivamani, R.K. Systematic Review of the Use of Platelet-Rich Plasma in Aesthetic Dermatology. J. Cosmet. Dermatol. 2015, 14, 315–323.
- Cook, C.S.; Smith, P.A. Clinical Update: Why PRP Should Be Your First Choice for Injection Therapy in Treating Osteoarthritis of the Knee. Curr. Rev. Musculoskelet. Med. 2018, 11, 583–592.
- Ince, B.; Yildirim, M.E.C.; Dadaci, M.; Avunduk, M.C.; Savaci, N. Comparison of the Efficacy of Homologous and Autologous Platelet-Rich Plasma (PRP) for Treating Androgenic Alopecia. Aesth Plast. Surg. 2018, 42, 297–303.
- Cecerska-Heryć, E.; Goszka, M.; Serwin, N.; Roszak, M.; Grygorcewicz, B.; Heryć, R.; Dołęgowska, B. Applications of the Regenerative Capacity of Platelets in Modern Medicine. Cytokine Growth Factor. Rev. 2022, 64, 84–94.
- Irmak, G.; Demirtaş, T.T.; Gümüşderelioğlu, M. Sustained Release of Growth Factors from Photoactivated Platelet Rich Plasma (PRP). Eur. J. Pharm. Biopharm. 2020, 148, 67–76.
- Alves, R.; Grimalt, R. A Review of Platelet-Rich Plasma: History, Biology, Mechanism of Action, and Classification. Skin. Appendage Disord. 2018, 4, 18–24.
- Prodromidou, A.; Grigoriadis, T.; Athanasiou, S. Platelet Rich Plasma for the Management of Urogynecological Disorders: The Current Evidence. Curr. Opin. Obstet. Gynecol. 2022, 34, 396–401.
- Casabona, F.; Gambelli, I.; Casabona, F.; Santi, P.; Santori, G.; Baldelli, I. Autologous Platelet-Rich Plasma (PRP) in Chronic Penile Lichen Sclerosus: The Impact on Tissue Repair and Patient Quality of Life. Int. Urol. Nephrol. 2017, 49, 573–580.
- Behnia-Willison, F.; Pour, N.R.; Mohamadi, B.; Willison, N.; Rock, M.; Holten, I.W.; O’Shea, R.; Miller, J. Use of Platelet-Rich Plasma for Vulvovaginal Autoimmune Conditions Like Lichen Sclerosus. Plast. Reconstr. Surg.-Glob. Open 2016, 4, e1124.
- Medina Garrido, C.; Cano García, A.; De La Cruz Cea, L.; Oreja Cuesta, A.B. Mid-Term Symptomatic Relief after Platelet-Rich Plasma Infiltration in Vulvar Lichen Sclerosus. Arch. Dermatol. Res. 2023, 315, 1527–1532.
- Goldstein, A.T.; Mitchell, L.; Govind, V.; Heller, D. A Randomized Double-Blind Placebo-Controlled Trial of Autologous Platelet-Rich Plasma Intradermal Injections for the Treatment of Vulvar Lichen Sclerosus. J. Am. Acad. Dermatol. 2019, 80, 1788–1789.
- Goldstein, A.T.; King, M.; Runels, C.; Gloth, M.; Pfau, R. Intradermal Injection of Autologous Platelet-Rich Plasma for the Treatment of Vulvar Lichen Sclerosus. J. Am. Acad. Dermatol. 2017, 76, 158–160.
- Tedesco, M.; Pranteda, G.; Chichierchia, G.; Paolino, G.; Latini, A.; Orsini, D.; Cristaudo, A.; Foddai, M.L.; Migliano, E.; Morrone, A. The Use of PRP (Platelet-rich Plasma) in Patients Affected by Genital Lichen Sclerosus: Clinical Analysis and Results. Acad. Dermatol. Venereol. 2019, 33, e58–e59.
- Franic, D.; Iternička, Z.; Franić-Ivanišević, M. Platelet-Rich Plasma (PRP) for the Treatment of Vulvar Lichen Sclerosus in a Premenopausal Woman: A Case Report. Case Rep. Women’s Health 2018, 18, e00062.
- Tedesco, M.; Garelli, V.; Elia, F.; Chicherchia, G.; Foddai, M.L.; Latini, A.; Morrone, A.; Migliano, E. Usefulness of Video Thermography in the Evaluation of Platelet-Rich Plasma Effectiveness in Vulvar Lichen Sclerosus: Preliminary Study. J. Dermatol. Treat. 2021, 32, 568–571.
- Navarrete, J.; Echarte, L.; Sujanov, A.; Guillones, A.; Vola, M.; Bunker, C.B.; Agorio, C.; Touriño, C. Platelet-rich Plasma for Male Genital Lichen Sclerosus Resistant to Conventional Therapy: First Prospective Study. Dermatol. Ther. 2020, 33, e14032.
- Tedesco, M.; Garelli, V.; Bellei, B.; Sperduti, I.; Chichierchia, G.; Latini, A.; Foddai, M.L.; Bertozzi, E.; Bonadies, A.; Pallara, T.; et al. Platelet-Rich Plasma for Genital Lichen Sclerosus: Analysis and Results of 94 Patients. Are There Gender-Related Differences in Symptoms and Therapeutic Response to PRP? J. Dermatol. Treat. 2022, 33, 1558–1562.
More
Information
Subjects:
Dermatology
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.1K
Revisions:
2 times
(View History)
Update Date:
23 Nov 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




