
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Domenico Plantone | -- | 2304 | 2023-10-18 19:09:53 | | | |
| 2 | Peter Tang | Meta information modification | 2304 | 2023-10-19 04:33:18 | | |
Video Upload Options
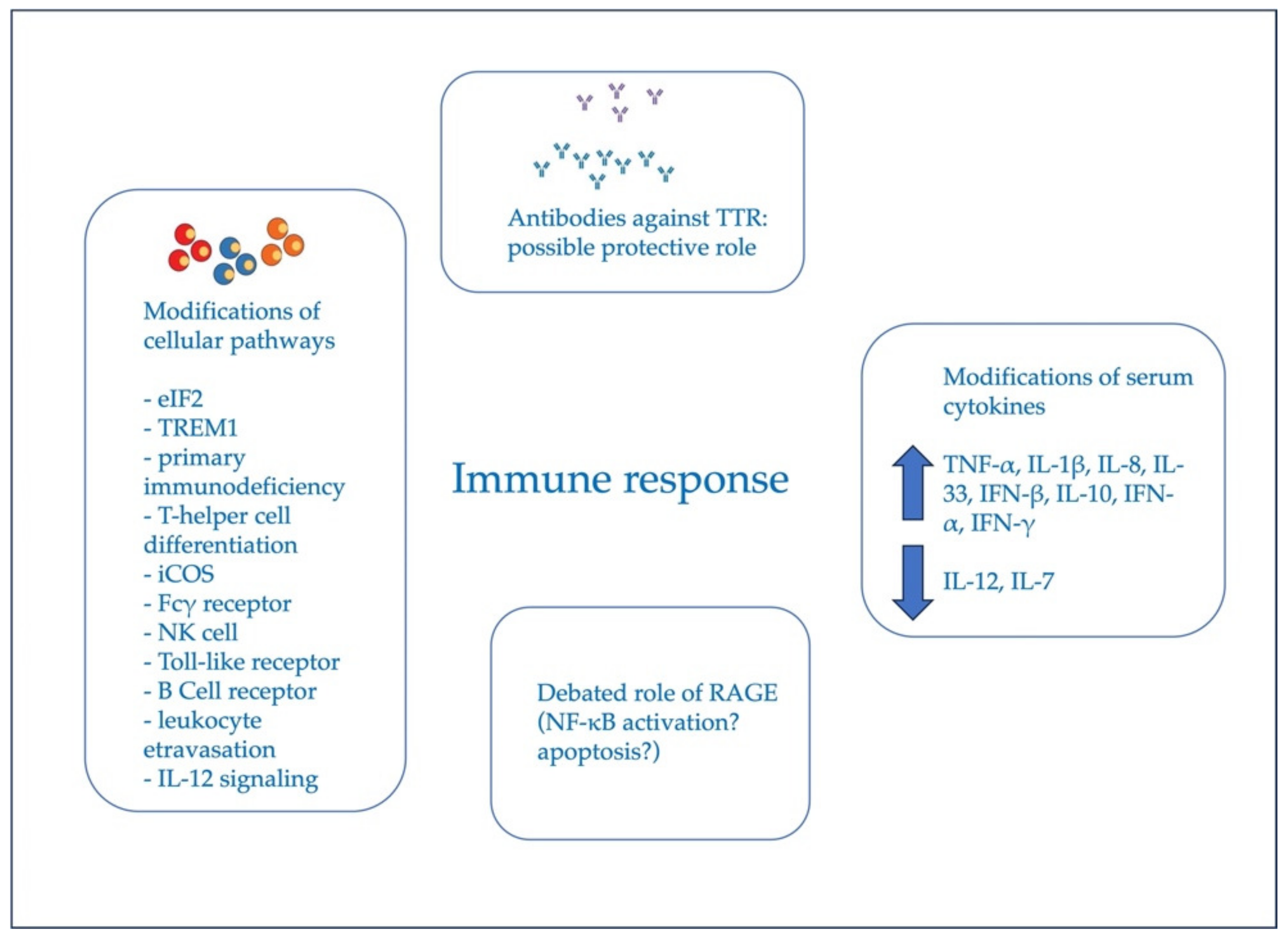
Hereditary transthyretin (ATTRv) amyloidosis with polyneuropathy, also known as familial amyloid polyneuropathy (FAP), represents a progressive, heterogeneous, severe, and multisystemic disease caused by pathogenic variants in the TTR gene. This autosomal-dominant neurogenetic disorder has an adult onset with variable penetrance and an inconstant phenotype, even among subjects carrying the same mutation. Historically, ATTRv amyloidosis has been viewed as a non-inflammatory disease, mainly due to the absence of any mononuclear cell infiltration in ex vivo tissues; nevertheless, a role of inflammation in its pathogenesis has been highlighted. The immune response may be involved in the development and progression of the disease. Fibrillary TTR species bind to the receptor for advanced glycation end products (RAGE), probably activating the nuclear factor κB (NF-κB) pathway. Moreover, peripheral blood levels of several cytokines, including interferon (IFN)-gamma, IFN-alpha, IL-6, IL-7, and IL-33, are altered in the course of the disease.
1. Introduction
2. Hereditary Transthyretin Amyloidosis with Polyneuropathy: Current Pathogenetic View
3. Evidence of Immune Response in ATTRv Amyloidosis
3.1. Human Studies: State of the Field
|
Reference |
Methods and Techniques |
Main Findings |
|---|---|---|
|
Sousa et al., 2001 [52] |
Analysis of nerve biopsy samples from patients by semiquantitative immunohistology and in situ hybridization |
Increased levels of RAGE beginning at the earliest stages of the disease; upregulation of TNF-α, IL1- β, and iNOS in a distribution overlapping RAGE expression. |
|
Matsunaga et al., 2002 [53] |
IHC and sequential IF staining |
RAGE and AGE have a distribution strongly correlated to that of amyloid deposits. However, no correlation was detected between NF-κB, apoptotic marker, and amyloid deposits. |
|
Azevedo et al., 2019 [7] |
ELISA |
Increased serum levels of TNF-α, IL-1β, IL-8, IL-33, IFN-β and IL-10, and decreased levels of IL-12 in ATTRv patients. |
|
Luigetti M et al., 2022 [8] |
Luminex XMAP multiplexing technology |
Increased serum levels of IFN-alpha and IFN-gamma, and decreased serum levels of IL-7 in ATTRv patients. |
|
Suenaga et al., 2017 [6] |
ELISA, cell culture, and Bio-Plex pro cytokine assay kit |
IL-6 serum concentration was elevated in FAP carriers. In native TTR culture conditions, IL-6 increased in CD14 + monocytes in the presence of V30M-mutated TTR, compared with wild-type TTR, in a TTR-dose-dependent manner. IL-6 concentration increased in CD4 + T cells and CD8 + T cells in a TTR-dose-dependent manner. IL-1β, TNF-α, and IL-10 increased in a TTR-dose-dependent manner in CD14 + monocytes. |
|
Kurian et al., 2016 [54] |
Microarray technology and Luminex bead assays |
Downregulation of eIF2 pathway in all symptomatic subjects, as well as primary immunodeficiency signaling, and purine nucleotide biosynthesis. Signaling networks for FCγ, TREM1, NK cells, IL3, IL15, and IL22 were all upregulated in FAP patients. Symptomatic females showed a downregulation of eIF2, primary immunodeficiency, T-helper cell differentiation, and iCOS signaling pathways. In symptomatic males, 29 significant canonical pathways linked to immunity, including Fcγ receptor, NK cell, Toll-like receptor, B-cell receptor, leukocyte etravasation, and IL-12 signaling, were all upregulated. There was a trend towards the normalization of all these altered gene expressions in patients treated with tafamidis. |
|
Moreira et al., 2023 [55] |
Real-time PCR, cell culture |
Plasma levels of S100A8 protein were lower in ATTR V30M patients compared to healthy controls; S100A8/9 levels in Schwann cells were dysregulated after incubation with human V30M TTR and by mutated bone marrow-derived macrophages in response to Toll-like receptor agonists. |
AGE, advanced glycation end products; ATTRv, transthyretin amyloidosis; CD, cluster of differentiation; eIF2, eukaryotic initiation factor-2; ELISA, enzyme-linked immunosorbent assays; FAP, familial amyloid polyneuropathy; iCOS, inducible T-cell costimulator; IF, immunofluorescence; IFN, interferon; IHC, immunohistochemistry; IL, interleukin; iNOS, inducible form of nitric oxide synthase; MCSF, macrophage colony-stimulating factor; NF-kB nuclear factor kappaB; NK, natural killer; RAGE, receptor for advanced glycation end products; SQ-IHC, semi-quantitative immunohistochemistry; TNF-α, tumor necrosis factor alpha; TREM1, triggering receptor expressed on myeloid cells 1; TTR, transthyretin.
3.2. Mechanistic Insight from Animal Studies
|
Reference |
Animal Model |
Methods and Techniques |
Main Findings |
|---|---|---|---|
|
Santos et al., 2010 [58] |
V30M TTR/HSF1 mice vs. WT mice |
SQ-IHC |
Increase in pro-inflammatory cytokines TNF- α and IL1-β, and NF-kB activation occurring in dorsal roots ganglia. |
|
Gonçalves et al., 2014 [59] |
V30M TTR/HSF1 mice vs. WT mice |
Flow cytometry and SQ-IHC |
Downregulation of Cxcl-3, Cxcl-2, Cxcl-12, and TLR 1. Lower expressions of TNF-α and IL-1β. Upregulation of IL-10. No difference in the expression of IL-6. |
|
Gonçalves et al., 2016 [60] |
V30M TTR/HSF1 mice vs. WT mice |
Microarray technology |
TLR 1, Cxcl2, and Cxcl 3 were confirmed to be downregulated. |
|
Moreira et al., 2021 [61] |
V30M TTR/mice vs. WT mice |
Real-time PCR |
Decreased expressions of chemokines, such as Ccl20, Ccl8, Ccl5, Cxcl5, Ccl2, Cxcl2, and Cxcl3. Downregulation of IL-6. |
|
Moreira et al., 2023 [62] |
V30M TTR/mice vs. WT mice |
Real-time PCR, cell culture |
The expressions of several chemokines by bone marrow-derived macrophages generated from V30M TTR mice after stimulation with TLR4 and TLR2 agonists decreased; p38, which has a pivotal role for TLR4 and TLR2 signaling pathways, presented a reduced phosphorylation in V30M macrophages, compared to WT ones. |
|
Gonçalves et al., 2015 [63] |
V30M TTR/mice vs. WT mice |
SQ-IHC; double immunofluorescence; immunogold labeling; real-time PCR; flow cytometry; Western blot; sciatic nerve morphometric analysis |
Treatment with the IL-1 receptor antagonist Anakinra in FAP mice decreased inflammation markers and improved axonal non-myelinated fibers. |
|
Buxbaum et al., 2012 [64] |
Transgenic model expressing approximately 90 copies of the wild-type human TTR gene under the control of its own promoter |
Transcriptomic analysis |
Hepatic chaperone activity was deficient in mice with cardiac deposition; robust cardiac inflammatory response in 3-month-old mice who have no cardiac deposits, which changes in the hearts of 15–24-month-old mice with either fibrillar or non-fibrillar deposits. |
ATTR, transthyretin amyloidosis; Ccl, chemokine ligand; Cxcl, C-X-C motif chemokine ligand 1; HSF1, heat shock factor 1; IL, interleukin; NF-kB, nuclear factor kappaB; PCR, polymerase chain reaction; SQ-IHC, semi-quantitative immunohistochemistry; TLR, Toll-like receptor; TNF-α, tumor necrosis factor-alpha; TTR, transthyretin; WT, wild type.
References
- Luigetti, M.; Romano, A.; Di Paolantonio, A.; Bisogni, G.; Sabatelli, M. Diagnosis and Treatment of Hereditary Transthyretin Amyloidosis (hATTR) Polyneuropathy: Current Perspectives on Improving Patient Care. Ther. Clin. Risk Manag. 2020, 16, 109–123.
- Adams, D.; Ando, Y.; Beirão, J.M.; Coelho, T.; Gertz, M.A.; Gillmore, J.D.; Hawkins, P.N.; Lousada, I.; Suhr, O.B.; Merlini, G. Expert consensus recommendations to improve diagnosis of ATTR amyloidosis with polyneuropathy. J. Neurol. 2021, 268, 2109–2122.
- Manganelli, F.; Fabrizi, G.M.; Luigetti, M.; Mandich, P.; Mazzeo, A.; Pareyson, D. Hereditary transthyretin amyloidosis overview. Neurol. Sci. 2022, 43 (Suppl. 2), 595–604.
- Adams, D.; Koike, H.; Slama, M.; Coelho, T. Hereditary transthyretin amyloidosis: A model of medical progress for a fatal disease. Nat. Rev. Neurol. 2019, 15, 387–404.
- Schmidt, H.H.; Waddington-Cruz, M.; Botteman, M.F.; Carter, J.A.; Chopra, A.S.; Hopps, M.; Stewart, M.; Fallet, S.; Amass, L. Estimating the global prevalence of transthyretin familial amyloid polyneuropathy. Muscle Nerve 2018, 57, 829–837.
- Suenaga, G.; Ikeda, T.; Masuda, T.; Motokawa, H.; Yamashita, T.; Takamatsu, K.; Misumi, Y.; Ueda, M.; Matsui, H.; Senju, S.; et al. Inflammatory State Exists in Familial Amyloid Polyneuropathy That May Be Triggered by Mutated Transthyretin. Sci. Rep. 2017, 7, 1579.
- Azevedo, E.P.; Guimaraes-Costa, A.B.; Bandeira-Melo, C.; Chimelli, L.; Waddington-Cruz, M.; Saraiva, E.M.; Palhano, F.L.; Foguel, D. Inflammatory Profiling of Patients with Familial Amyloid Polyneuropathy. BMC Neurol. 2019, 19, 146.
- Luigetti, M.; Romano, A.; Guglielmino, V.; Sciarrone, M.A.; Vitali, F.; Carbone, C.; Piro, G.; Sabino, A.; De Stefano, N.; Plantone, D.; et al. Serum Inflammatory Profile in Hereditary Transthyretin Amyloidosis: Mechanisms and Possible Therapeutic Implications. Brain Sci. 2022, 12, 1708.
- Cras-Meneur, C.; Inoue, H.; Zhou, Y.; Ohsugi, M.; Bernal-Mizrachi, E.; Pape, D.; Clifton, S.W.; Permutt, M.A. An expression profile of human pancreatic islet mRNAs by Serial Analysis of Gene Expression (SAGE). Diabetologia 2004, 47, 284–299.
- Buxbaum, J.N.; Reixach, N. Transthyretin: The Servant of Many Masters. Cell. Mol. Life Sci. 2009, 66, 3095–3101.
- Ueda, M. Transthyretin: Its Function and Amyloid Formation. Neurochem. Int. 2022, 155, 3095–3101.
- Palha, J.A. Transthyretin as a Thyroid Hormone Carrier: Function Revisited. Clin. Chem. Lab. Med. 2002, 40, 1292–1300.
- Blake, C.C.F.; Geisow, M.J.; Swan, I.D.A.; Rerat, C.; Rerat, B. Structure of Human Plasma Prealbumin at 2.5 A Resolution. A Preliminary Report on the Polypeptide Chain Conformation, Quaternary Structure and Thyroxine Binding. J. Mol. Biol. 1974, 88, 1–12.
- Tozza, S.; Severi, D.; Spina, E.; Iovino, A.; Aruta, F.; Ruggiero, L.; Dubbioso, R.; Iodice, R.; Nolano, M.; Manganelli, F. The Neuropathy in Hereditary Transthyretin Amyloidosis: A Narrative Review. J. Peripher. Nerv. Syst. 2021, 26, 155–159.
- Dyck, P.J.B.; Coelho, T.; Waddington Cruz, M.; Brannagan, T.H.; Khella, S.; Karam, C.; Berk, J.L.; Polydefkis, M.J.; Kincaid, J.C.; Wiesman, J.F.; et al. Neuropathy Symptom and Change: Inotersen Treatment of Hereditary Transthyretin Amyloidosis. Muscle Nerve 2020, 62, 509–515.
- Fernandes, A.; Coelho, T.; Rodrigues, A.; Felgueiras, H.; Oliveira, P.; Guimarães, A.; Melo-Pires, M.; Taipa, R. Clinicopathological Correlations of Sural Nerve Biopsies in TTR Val30Met Familial Amyloid Polyneuropathy. Brain Commun. 2019, 1, fcz032.
- Skrahina, V.; Grittner, U.; Beetz, C.; Skripuletz, T.; Juenemann, M.; Krämer, H.H.; Hahn, K.; Rieth, A.; Schaechinger, V.; Patten, M.; et al. Hereditary Transthyretin-Related Amyloidosis Is Frequent in Polyneuropathy and Cardiomyopathy of No Obvious Aetiology. Ann. Med. 2021, 53, 1787–1796.
- Sekijima, Y. Transthyretin (ATTR) Amyloidosis: Clinical Spectrum, Molecular Pathogenesis and Disease-Modifying Treatments. J. Neurol. Neurosurg. Psychiatry 2015, 86, 1036–1043.
- Carroll, A.; Dyck, P.J.; De Carvalho, M.; Kennerson, M.; Reilly, M.M.; Kiernan, M.C.; Vucic, S. Novel Approaches to Diagnosis and Management of Hereditary Transthyretin Amyloidosis. J. Neurol. Neurosurg. Psychiatry 2022, 93, 668–678.
- Cortese, A.; Vegezzi, E.; Lozza, A.; Alfonsi, E.; Montini, A.; Moglia, A.; Merlini, G.; Obici, L. Diagnostic Challenges in Hereditary Transthyretin Amyloidosis with Polyneuropathy: Avoiding Misdiagnosis of a Treatable Hereditary Neuropathy. J. Neurol. Neurosurg. Psychiatry 2017, 88, 457–458.
- Mathis, S.; Magy, L.; Diallo, L.; Boukhris, S.; Vallat, J.M. Amyloid Neuropathy Mimicking Chronic Inflammatory Demyelinating Polyneuropathy. Muscle Nerve 2012, 45, 26–31.
- Planté-Bordeneuve, V.; Said, G. Familial Amyloid Polyneuropathy. Lancet Neurol. 2011, 10, 1086–1097.
- Vera-Llonch, M.; Reddy, S.R.; Chang, E.; Tarbox, M.H.; Pollock, M. The Patient Journey toward a Diagnosis of Hereditary Transthyretin (ATTRv) Amyloidosis. Orphanet. J. Rare Dis. 2021, 16, 25.
- Koike, H.; Katsuno, M. Transthyretin Amyloidosis: Update on the Clinical Spectrum, Pathogenesis, and Disease-Modifying Therapies. Neurol Ther. 2020, 9, 317–333.
- Stewart, M.; Shaffer, S.; Murphy, B.; Loftus, J.; Alvir, J.; Cicchetti, M.; Lenderking, W.R. Characterizing the High Disease Burden of Transthyretin Amyloidosis for Patients and Caregivers. Neurol. Ther. 2018, 7, 349–364.
- Yarlas, A.; Gertz, M.A.; Dasgupta, N.R.; Obici, L.; Pollock, M.; Ackermann, E.J.; Lovley, A.; Kessler, A.S.; Patel, P.A.; White, M.K.; et al. Burden of Hereditary Transthyretin Amyloidosis on Quality of Life. Muscle Nerve 2019, 60, 169–175.
- Tozza, S.; Luigetti, M.; Antonini, G.; Mazzeo, A.; Severi, D.; Di Paolantonio, A.; Leonardi, L.; Russo, M.; Romano, A.; Forcina, F.; et al. Neuropathic Pain Experience in Symptomatic and Presymptomatic Subjects Carrying a Transthyretin Gene Mutation. Front. Neurol. 2023, 14, 1109782.
- Coelho, T.; Waddington Cruz, M.; Chao, C.C.; Parman, Y.; Wixner, J.; Weiler, M.; Barroso, F.A.; Dasgupta, N.R.; Jung, S.W.; Schneider, E.; et al. Characteristics of Patients with Hereditary Transthyretin Amyloidosis-Polyneuropathy (ATTRv-PN) in NEURO-TTRansform, an Open-Label Phase 3 Study of Eplontersen. Neurol. Ther. 2023, 12, 267–287.
- Benbrahim, M.; Norman, K.; Sanchorawala, V.; Siddiqi, O.K.; Hughes, D. A Review of Novel Agents and Clinical Considerations in Patients with ATTR Cardiac Amyloidosis. J. Cardiovasc. Pharmacol. 2021, 77, 544–548.
- Ferraro, P.M.; D’Ambrosio, V.; Di Paolantonio, A.; Guglielmino, V.; Calabresi, P.; Sabatelli, M.; Luigetti, M. Renal Involvement in Hereditary Transthyretin Amyloidosis: An Italian Single-Centre Experience. Brain Sci. 2021, 11, 980.
- Ando, Y.; Adams, D.; Benson, M.D.; Berk, J.L.; Planté-Bordeneuve, V.; Coelho, T.; Conceição, I.; Ericzon, B.G.; Obici, L.; Rapezzi, C.; et al. Guidelines and New Directions in the Therapy and Monitoring of ATTRv Amyloidosis. Amyloid 2022, 29, 143–155.
- Dardiotis, E.; Kyriakides, T. Drug and Gene Therapy for Treating Variant Transthyretin Amyloidosis (ATTRv) Neuropathy. Curr. Neuropharmacol. 2022, 21, 471–481.
- Holmgren, G.; Steen, L.; Suhr, O.; Ericzon, B.G.; Groth, C.G.; Andersen, O.; Wallin, B.G.; Seymour, A.; Richardson, S.; Hawkins, P.N.; et al. Clinical Improvement and Amyloid Regression after Liver Transplantation in Hereditary Transthyretin Amyloidosis. Lancet 1993, 341, 1113–1116.
- Okamoto, S.; Wixner, J.; Obayashi, K.; Ando, Y.; Ericzon, B.G.; Friman, S.; Uchino, M.; Suhr, O.B. Liver Transplantation for Familial Amyloidotic Polyneuropathy: Impact on Swedish Patients’ Survival. Liver Transplant. 2009, 15, 1229–1235.
- Wilczek, H.E.; Larsson, M.; Ericzon, B.G. Long-Term Data from the Familial Amyloidotic Polyneuropathy World Transplant Registry (FAPWTR). Amyloid 2011, 18 (Suppl. 1), 193–195.
- Sekijima, Y.; Tojo, K.; Morita, H.; Koyama, J.; Ikeda, S.I. Safety and Efficacy of Long-Term Diflunisal Administration in Hereditary Transthyretin (ATTR) Amyloidosis. Amyloid 2015, 22, 79–83.
- Merlini, G.; Planté-Bordeneuve, V.; Judge, D.P.; Schmidt, H.; Obici, L.; Perlini, S.; Packman, J.; Tripp, T.; Grogan, D.R. Effects of Tafamidis on Transthyretin Stabilization and Clinical Outcomes in Patients with Non-Val30Met Transthyretin Amyloidosis. J. Cardiovasc. Transl. Res. 2013, 6, 1011–1120.
- Adams, D.; Gonzalez-Duarte, A.; O’Riordan, W.D.; Yang, C.-C.; Ueda, M.; Kristen, A.V.; Tournev, I.; Schmidt, H.H.; Coelho, T.; Berk, J.L.; et al. Patisiran, an RNAi Therapeutic, for Hereditary Transthyretin Amyloidosis. N. Engl. J. Med. 2018, 379, 11–21.
- Benson, M.D.; Waddington-Cruz, M.; Berk, J.L.; Polydefkis, M.; Dyck, P.J.; Wang, A.K.; Planté-Bordeneuve, V.; Barroso, F.A.; Merlini, G.; Obici, L.; et al. Inotersen Treatment for Patients with Hereditary Transthyretin Amyloidosis. N. Engl. J. Med. 2018, 379, 22–31.
- Benson, M.D.; Dasgupta, N.R.; Rissing, S.M.; Smith, J.; Feigenbaum, H. Safety and Efficacy of a TTR Specific Antisense Oligonucleotide in Patients with Transthyretin Amyloid Cardiomyopathy. Amyloid 2017, 24, 219–225.
- Adams, D.; Tournev, I.L.; Taylor, M.S.; Coelho, T.; Planté-Bordeneuve, V.; Berk, J.L.; González-Duarte, A.; Gillmore, J.D.; Low, S.C.; Sekijima, Y.; et al. Efficacy and safety of vutrisiran for patients with hereditary transthyretin-mediated amyloidosis with polyneuropathy: A randomized clinical trial. Amyloid 2023, 30, 1–9.
- Koike, H.; Nishi, R.; Ikeda, S.; Kawagashira, Y.; Iijima, M.; Sakurai, T.; Shimohata, T.; Katsuno, M.; Sobue, G. The Morphology of Amyloid Fibrils and Their Impact on Tissue Damage in Hereditary Transthyretin Amyloidosis: An Ultrastructural Study. J. Neurol. Sci. 2018, 394, 99–106.
- Koike, H.; Ikeda, S.; Takahashi, M.; Kawagashira, Y.; Iijima, M.; Misumi, Y.; Ando, Y.; Ikeda, S.I.; Katsuno, M.; Sobue, G. Schwann Cell and Endothelial Cell Damage in Transthyretin Familial Amyloid Polyneuropathy. Neurology 2016, 87, 2220–2229.
- Coimbra, A.; Andrade, C. Familial Amyloid Polyneuropathy: An Electron Microscope Study of the Peripheral Nerve in Five Cases. I. Interstitial Changes. Brain 1971, 94, 199–206.
- Ando, Y.; Nyhlin, N.; Suhr, O.; Holmgren, G.; Uchida, K.; El Sahly, M.; Yamashita, T.; Terasaki, H.; Nakamura, M.; Uchino, M.; et al. Oxidative Stress Is Found in Amyloid Deposits in Systemic Amyloidosis. Biochem. Biophys. Res. Commun. 1997, 232, 497–502.
- Koike, H.; Misu, K.; Sugiura, M.; Iijima, M.; Mori, K.; Yamamoto, M.; Hattori, N.; Mukai, E.; Ando, Y.; Ikeda, S.; et al. Pathology of Early- vs Late-Onset TTR Met30 Familial Amyloid Polyneuropathy. Neurology 2004, 63, 129–138.
- Ihse, E.; Ybo, A.; Suhr, O.B.; Lindqvist, P.; Backman, C.; Westermark, P. Amyloid Fibril Composition Is Related to the Phenotype of Hereditary Transthyretin V30M Amyloidosis. J. Pathol. 2008, 216, 253–261.
- Saraiva, M.J.; Magalhaes, J.; Ferreira, N.; Almeida, M.R. Transthyretin deposition in familial amyloidotic polyneuropathy. Curr. Med. Chem. 2012, 19, 2304–2311.
- Sousa, M.M.; Saraiva, M.J. Neurodegeneration in Familial Amyloid Polyneuropathy: From Pathology to Molecular Signaling. Prog. Neurobiol. 2003, 71, 385–400.
- Sousa, M.M.; Ferraõ, J.; Fernandes, R.; Guimarães, A.; Geraldes, J.B.; Perdigoto, R.; Tomé, L.; Mota, O.; Negrão, L.; Furtado, A.L.; et al. Deposition and Passage of Transthyretin through Blood-Nerve Barrier in Recipients of Familial Amyloid Polyneuropathy Livers. Lab. Investig. 2004, 84, 865–873.
- Macedo, B.; Batista, A.R.; do Amaral, J.B.; Saraiva, M.J. Biomarkers in the assessment of therapies for familial amyloidotic polyneuropathy. Mol. Med. 2007, 13, 584–591.
- Sousa, M.M.; Yan, S.D.; Fernandas, R.; Guimarães, A.; Stern, D.; Saraiva, M.J. Familial Amyloid Polyneuropathy: Receptor for Advanced Glycation End Products-Dependent Triggering of Neuronal Inflammatory and Apoptotic Pathways. J. Neurosci. 2001, 21, 7576–7586.
- Matsunaga, N.; Anan, I.; Forsgren, S.; Nagai, R.; Rosenberg, P.; Horiuchi, S.; Ando, Y.; Suhr, O.B. Advanced Glycation End Products (AGE) and the Receptor for AGE Are Present in Gastrointestinal Tract of Familial Amyloidotic Polyneuropathy Patients but Do Not Induce NF-ΚB Activation. Acta Neuropathol. 2002, 104, 441–447.
- Kurian, S.M.; Novais, M.; Whisenant, T.; Gelbart, T.; Buxbaum, J.N.; Kelly, J.W.; Coelho, T.; Salomon, D.R. Peripheral Blood Cell Gene Expression Diagnostic for Identifying Symptomatic Transthyretin Amyloidosis Patients: Male and Female Specific Signatures. Theranostics 2016, 6, 1792–1809.
- Moreira, J.; Martins, S.; Saraiva, M.; Saraiva, M.J. Decreased expression of S100A8/A9 in V30M related ATTRv amyloidosis. Amyloid 2023, 30, 1–8.
- Faravelli, G.; Mondani, V.; Mangione, P.P.; Raimondi, S.; Marchese, L.; Lavatelli, F.; Stoppini, M.; Corazza, A.; Canetti, D.; Verona, G.; et al. Amyloid Formation by Globular Proteins: The Need to Narrow the Gap Between in Vitro and in Vivo Mechanisms. Front. Mol. Biosci. 2022, 9, 830006.
- Yi, S.; Takahashi, K.; Naito, M.; Tashiro, F.; Wakasugi, S.; Maeda, S.; Shimada, K.; Yamamura, K.; Araki, S. Systemic Amyloidosis in Transgenic Mice Carrying the Human Mutant Transthyretin (Met30) Gene. Pathologic Similarity to Human Familial Amyloidotic Polyneuropathy, Type I. Am. J. Pathol. 1991, 138, 403–412.
- Santos, S.D.; Fernandes, R.; Saraiva, M.J. The Heat Shock Response Modulates Transthyretin Deposition in the Peripheral and Autonomic Nervous Systems. Neurobiol. Aging 2010, 31, 280–289.
- Gonçalves, N.P.; Teixeira-Coelho, M.; Saraiva, M.J. The Inflammatory Response to Sciatic Nerve Injury in a Familial Amyloidotic Polyneuropathy Mouse Model. Exp. Neurol. 2014, 257, 76–87.
- Gonçalves, N.P.; Martins, D.; Saraiva, M.J. Overexpression of Protocadherin-10 in Transthyretin-Related Familial Amyloidotic Polyneuropathy. Am. J. Pathol. 2016, 186, 1913–1924.
- Moreira, J.; Costelha, S.; Saraiva, M.; Saraiva, M.J. The Expression of Chemokines Is Downregulated in a Pre-Clinical Model of TTR V30M Amyloidosis. Front. Immunol. 2021, 12, 1823.
- Moreira, J.; Martins, H.; Saraiva, M.; Saraiva, M.J. TLR2 and 4 signaling pathways are altered in macrophages from V30M TTR mice with down-regulated expression of chemokines. Clin. Sci. 2023, 137, 355–366.
- Gonçalves, N.P.; Teixeira-Coelho, M.; Saraiva, M.J. Protective role of anakinra against transthyretin-mediated axonal loss and cell death in a mouse model of familial amyloidotic polyneuropathy. J. Neuropathol. Exp. Neurol. 2015, 74, 203–217.
- Buxbaum, J.N.; Tagoe, C.; Gallo, G.; Walker, J.R.; Kurian, S.; Salomon, D.R. Why are some amyloidoses systemic? Does hepatic “chaperoning at a distance” prevent cardiac deposition in a transgenic model of human senile systemic (transthyretin) amyloidosis? FASEB J. 2012, 26, 2283–2293.




