Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Maria de los Angeles Robinson-Agramonte | -- | 4077 | 2023-10-12 02:42:35 | | | |
| 2 | Jessie Wu | + 1 word(s) | 4078 | 2023-10-12 05:25:44 | | | | |
| 3 | Jessie Wu | Meta information modification | 4078 | 2023-10-12 05:26:35 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Robinson-Agramonte, M.D.L.A.; Sánchez, T.S.; García, E.N.; Barrera, O.R.S.; Siniscalco, D. COVID-19 and the Nervous System. Encyclopedia. Available online: https://encyclopedia.pub/entry/50165 (accessed on 07 February 2026).
Robinson-Agramonte MDLA, Sánchez TS, García EN, Barrera ORS, Siniscalco D. COVID-19 and the Nervous System. Encyclopedia. Available at: https://encyclopedia.pub/entry/50165. Accessed February 07, 2026.
Robinson-Agramonte, Maria De Los Angeles, Teresa Serrano Sánchez, Elena Noris García, Orlando Rafael Serrano Barrera, Dario Siniscalco. "COVID-19 and the Nervous System" Encyclopedia, https://encyclopedia.pub/entry/50165 (accessed February 07, 2026).
Robinson-Agramonte, M.D.L.A., Sánchez, T.S., García, E.N., Barrera, O.R.S., & Siniscalco, D. (2023, October 12). COVID-19 and the Nervous System. In Encyclopedia. https://encyclopedia.pub/entry/50165
Robinson-Agramonte, Maria De Los Angeles, et al. "COVID-19 and the Nervous System." Encyclopedia. Web. 12 October, 2023.
Copy Citation
Neuropsychiatric manifestations of viral infections (both per se and secondary to the neuroinflammatory reaction of the host) are mainly attributed to immunological reactions, so many aspects of their pathogenesis are still nuclear. Some novel therapeutic strategies are progressively emerging in which a vaccination may be having a particular impact on recovery and reduction of death. In this context, it is accepted that the SARS-CoV-2 virus is profoundly neurotropic and neuroinvasive, with various effects on the nervous system, although there is no complete understanding of the mechanism of neuroinvasion, brain injury, or short- or long-term neuropsychiatric sequelae.
COVID-19
nervous system
neuroinflammation
SARS-CoV-2
1. Neuropsychiatry Manifestation and COVID-19
The COVID-19 pandemic represents a challenge for the future in health systems due to its impact outside of the respiratory system. Identifying the main neurological and neuropsychiatric manifestations associated with COVID-19 has been the focus of several research groups around the world, either as reports of cases or papers describing the main clinical manifestations in the short or long term of COVID-19.
Aguiar-González et al. published two papers in 2021 in Magazine of the Medical University of the Province of Pinar del Río (www.revgaleno.sld.cu, accessed on 20 July 2023), one of which is titled “Neurological manifestations in patients with COVID-19” [1]. In this research, the authors referred to the challenge that the COVID-19 pandemic represents for health systems due to the impact on different body systems, such as the respiratory, cardiovascular, and nervous systems. From about 30 articles reviewed by these authors, several conclusions were reached: (1) The olfactory nerves and the invasion of the peripheral nerve terminals are the main suggested routes of entry of the SARS-CoV-2 virus into the brain [1], and (2) severe neural symptoms are associated with lesions of other organs such as the CNS and also with cytokine storm. In addition, the authors concluded that headache appears to be the most common neurological manifestation in patients with COVID-19, whereas rhabdomyolysis, acute necrotizing hemorrhagic encephalopathy, Guillain Barré syndrome (GBS), meningitis, and encephalitis are less frequent in COVID-19 patients [2][3][4]. This research described the most frequent neurological symptoms in patients in different age groups and with severe/mild COVID-19, stratified into CNS disorders and peripheral nervous system (PNS) disorders:
1.1. Most Frequent Symptom of Central Nervous System in COVID-19
Headache was the most common CNS neurological manifestation reported by patients with COVID-19. Between 8 and 34% of patients in China presented this symptom, generally with mild intensity [5]. In addition to headache, vomiting, and nausea, vertigo was a recurring symptom in 7–9% of patients with COVID-19.
The first one described in a general way the high probability that the ventilatory dysfunction of patients is based on the involvement of the cardiorespiratory center in the brain stem beyond lung lesions and why it is very important to be alert to neurological manifestations that can occur even in the early stages of patients with COVID-19. Experimental and clinical data from SARS-CoV-2 infections in the brain were presented to describe the different pathways through which the virus manages to invade the brain via the olfactory CNS to spread locally. The authors also described the trans-synaptic pathway, the pathway that connects the cardiorespiratory center with the mechanoreceptors and chemoreceptors of lung tissue and the respiratory tract, underlining the impact of this pathway on ventilatory failure in these patients. A particular aspect reviewed in this research is the invasion of neurons and neuroglia by coronaviruses, facilitated by the expression of ACE2 on their surface, which allows direct infection at the CNS level parallel to the inflammatory process at the systemic level that occurs during COVID-19. The latter compromises the BBB and provides access of inflammatory elements to the CNS and neuroinflammation, reactive astrogliosis, and microglial activation, which means that various neurological processes can potentially lead to ventilatory disorders based on the influence on the cardiorespiratory center due to the impact on the brainstem. Finally, the authors emphasized the need to be alerted early to the presence of neurological manifestations in patients with COVID-19, as well as the need to be able to count on tools to identify predictive biomarkers and prognoses for intervention and sequelae prevention [6].
The second article, titled “Olfactory dysfunction and COVID-19”, referred to the smell disorders that precede or accompany SARS-CoV-2 infection as a simple clinical manifestation of COVID-19 [7]. This research aimed to analytically summarize the scientific evidence of the relationship of olfactory dysfunction derived from SARS-CoV-2 infection and was designed by using the Google Scholar search engine with the descriptors “COVID-19”, “SARS-CoV-2”, “anosmia”, and “hyposmia”. The results of the review ranged from case reports to published research and review articles on the involvement of the olfactory pathway in COVID-19 and the possible pathophysiological mechanisms involved. Similar to other previous results discussed here, these authors concluded that olfactory disorders preceding or accompanying SARS-CoV-2 infection could be an isolated clinical manifestation of COVID-19 and therefore should be considered. Based on this last perspective, the authors also considered that quantitative neurophysiological testing and hybrid imaging of the olfactory bulb could be useful tools to clarify the mechanism and establish the probable association between the structural changes and connectivity produced by the invasion of SARS-CoV-2 of the olfactory pathway and suggested adding a history of smell disorders to the clinical history of patients with COVID-19 as mandatory data, since the demonstration of the relationship between smell disorders and SARS-CoV-2 infections could have diagnostic or prognostic value [7].
1.2. Most Frequent Symptoms of PNS in COVID-19
Based on this research, the authors considered that anosmia/hyposmia and, secondarily, taste disorders, constitute primary symptoms associated with SARS-CoV-2 infection and that their early identification is of vital importance to reducing the impact of the infection. Although anosmia is not specific to SARS-CoV-2 infection, it is linked to taste disorders, which are common in people with COVID-19, even in the absence of nasal symptoms [8], and could be early markers of SARS-CoV-2 infection. Regarding its origin, the authors stated that it follows direct damage to the olfactory receptor neurons [9]. This last hypothesis is favored by the expression of receptors for ACE 2 proteins and for serine transmembrane protease 2 (TMPRSS2) in cells of the olfactory epithelium, which are necessary for SARS-CoV-2 infection in humans [10][11] and were described in anosmia in 5.1% of patients and in ageusia in 5.6%.
Machado and DeFina also wrote about anosmia and ageusia, arguing that they are the only symptoms prior to COVID-19 [12]. Their article defines the terms “anosmia” as the temporary or permanent loss of the ability to detect one or more odors and “ageusia” as the loss of taste functions of the tongue, mainly including the inability to taste sweetness, acidity, bitterness, salinity, or umami—which is a pleasant/tasty taste—and the loss of olfactory neural pathways, considering that this olfactory conduction pathway begins with olfactory receptors and taste. The article also details how the mechanisms lead to loss of smell and taste from SARS-CoV-2 infection [13]. Regarding this last aspect, the authors emphasized that the loss of smell could be due to inflammation of the nose and paranasal sinuses due to chronic sinusitis, head injuries, or nervous disorders (such as Parkinson’s disease) [14]. In addition, they stated that loss of smell from a viral infection such as the common cold is the second most common cause of loss of smell, present in about 12% of all cases of anosmia, and noted that these episodes usually occur when the virus infects the nose [15]. In this research, the authors also reported that the peripheral trigeminal or olfactory nerves, known routes of penetration of coronaviruses into the CNS, can explain the complications derived from brain invasion by SARS-CoV-2, such as demyelination and mediated autoimmunity by T cells—reactions that may be part of the path of infection spread—so the incidence of dyssomnia and dysgeusia could be a potentially painful consequence of these brain lesions [13]. These authors considered the most relevant signs and symptoms of COVID-19 to be fever (98%), cough (76%), dyspnea (55%), and myalgia or fatigue (44%). However, an association between COVID-19 and altered olfactory and taste functions were suggested, although smell seems to be more affected than taste.
Robinson-Agramonte et al. published a relevant article titled “Impact of SARS-CoV-2 on neuropsychiatric disorders” in 2021 [16] based on the high number of reported case series and unclear evidence of the involvement of the immune system in the pathological mechanism of COVID-19. The authors focused the review on the suggested immunological mechanism involving the direct effect of SARS-CoV-2 infection on the CNS and neuroinflammation and described the neuropsychiatric disorders associated with COVID-19. Symptoms and signs such as depression, anxiety, mood disturbances, psychosis, post-traumatic stress disorder, delirium, and cognitive impairment appeared to be common in COVID-19 survivors, as well as a worsening of scores on psychopathology measures after a history of comorbidities. The authors also made a critical analysis of the innate and adaptive immune system aspects involved in the mental health disorders that occur with COVID-19 [16][17].
Following what has been described in these articles, neuroinflammation impacts disease pathology such as schizophrenia and autism and involves mental illness in COVID-19 in a close interaction between the systemic compartment and the brain [17].
Lorigados and Pavón summarized the main experiences reported in the presence of CNS conditions related to COVID-19 and analyzed the relationship between COVID-19 and neurological diseases [18]. They described the presence of IgM-class anti-CoV antibodies in 12% (n = 183) of patients with clinical suspicion of acute encephalitis, different from that reported for prior MERS-CoV infection (26% in patients with mental disorders and 9% in those with a history of seizures). The authors also referred to the behavior of the most frequent neurological manifestations associated with COVID-19 and pointed out that, in a record published by Ahmad I and Rathore FA in 2020, between 68 and 75% of COVID-19-positive patients had loss of smell and between 71 and 43% had dysgeusia. On the other hand, there is recent evidence of CNS invasion in patients with SARS-CoV-2 and with positive RNA in the CSF and on the neuropathological mechanisms that mediate CNS involvement, which are mediated by hypoxic brain damage and associated with immune mechanisms. The first of these mechanisms is a consequence of severe pneumonia, resulting in systemic hypoxia and leading to cerebral hypoxia; the second is due to an inflammatory cytokine storm followed by activation of T lymphocytes, macrophages, and endothelial cells. Interleukin 6 (IL-6) is known to cause vascular involvement, complement activation, and participate in the coagulation cascade, along with intravascular spread and organ damage.
Unlike the articles reviewed so far, this research described particular behavioral aspects of the neurological manifestations associated with COVID-19, such as Parkinson’s disease, encephalopathies, GBS, epilepsy, and stroke. In all cases, a clinical case was shown and the behavior of the SARS-CoV-2 infection and the disease was described, with clinical and paraclinical evidence [18]. Finally, the authors called attention to prioritizing the evaluation of neurological events present in these patients, both from the clinical and the prognostic point of view, in order to prevent the most severe course of the disease in SARS-CoV-2 patients.
Regarding neuropsychiatric disorders, Bender and colleagues summarized the scientific evidence on the impact of COVID-19 on neuropsychiatric disorders. The search with the Google Scholar engine was rich and the descriptors of “COVID-19”, “SARS-CoV-2”, and “neuropsychiatric manifestations” were used. This research described the general clinical manifestations of COVID-19 and subacute or chronic psychiatric sequelae in relation to SARS-CoV-2 infection, including depression, anxiety, and stress. Related to other works, the need for care for health personnel and patients with previous mental illness and chronic neurological diseases, in whom symptoms can worsen and even lead to suicide, is emphasized [19]. Long-term psychiatric complications after SARS-CoV-2 infection are currently unknown. In this research, the authors referred to studies published by Severance et al. M, who found a higher prevalence of antibodies against four strains of HCoV in patients with a recent psychotic episode compared to non-psychiatric controls, which allowed Severance et al. to suggest a possible relationship between CoV infections and psychosis, with potential for its occurrence following SARS-CoV-2 infection. The authors also made a specific reference to the works published by Valdés-Florido et al., referring to the occurrence of psychotic episodes during the first two weeks of quarantine in patients admitted in Seville, Spain, in whom the confirmation of the diagnosis followed the psychotic disorder criteria of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). In the opinion of the authors, the episodes were triggered by the stress derived from the COVID-19 pandemic, and half of the patients presented severe suicidal behavior on admission [20]. Bender et al. warned, in turn, about the risk presented by the increase in the number of brief reactive psychotic disorders as a result of the COVID-19 pandemic [19].
2. COVID-19 and Other Neurological Diseases
The involvement of the CNS has been considered since the first cases of COVID-19, and epilepsy, ataxia, and impaired consciousness are among the most frequent neurological manifestations [15].
2.1. Epilepsy and COVID-19
In a letter to the editor, Bender et al. reflected on the need to consider the action protocols related to the appearance of epilepsy seizures in COVID-19 based on the first published case associating epileptic seizures with the course of COVID-19 infection. In the opinion of these authors, many viruses may play a role in the development of epileptic seizures, and in this case the cause may be directly related to a primary infection of the CNS [21]. Another paper published by these authors sent a message to give a warning about the importance of monitoring seizures in epileptic patients who are infected with SARS-CoV-2, because it may increase the risk of epileptic seizures, similar to any acute infection, and in turn, the infection can become a triggering factor for crises. They also stressed that it is not the viral infection that can cause epileptic seizures but sepsis, the fever that accompanies it, and sleep deprivation [22]. Both articles also drew attention to the need for adherence of the professionals involved in the treatment of these patients to following the guidelines of the International League Against Epilepsy, which alerts, among other aspects, about the possible interactions of antiepileptic drugs with the drugs used in disease action protocols.
2.2. Hereditary Ataxias and COVID-19
Possible pathophysiological implications and recommendations are the topics of a review article by Velazquez et al. [23]. The authors argued how patients with hereditary ataxias constitute a vulnerable group, given the well-known functional disturbance of the immune system, the central disturbances of respiratory control, and the existence of comorbidities that increase the risk of health worsening derived from COVID-19, such as cardiopathies, diabetes mellitus, and cancer, and underlined a series of practical recommendations. The authors briefly summarized the characteristics of the main types of ataxia and the relationship between ataxin-2 and RNA+ virus infections and suggested that loss of biological function in patients could protect them against infections.
Friedreich’s ataxia is an autosomal recessive cerebellar ataxia caused by abnormally long expansions of the repetitive guanine–adenine–adenine (GAA) sequence, which prevents the correct expression of the Friedreich’s ataxia (FRDA) gene. In this disease, the main warning for its management in the case of SARS-CoV-2 infection is that these patients usually have heart disease and diabetes mellitus, two comorbid conditions that aggravate COVID-19 and increase mortality. On the other hand, these patients also present alterations in the regulation of the respiratory activity, mainly mediated by autonomic dysfunction [23]. This element could be disadvantageous for the disease.
Ataxia-telangiectasia, another type of ataxia with an autosomal recessive pattern of inheritance, is produced by localized mutations in the ATM gene (11q22.3) and is characterized by a cerebellar syndrome associated with a combined immunodeficiency that mainly affects the humoral immune response. Several authors considered that these patients should receive greater family and medical attention during the current pandemic, as they present a significant susceptibility to infections [23][24]. In general, the social isolation of these patients may have consequences on their physical and mental health, given their dependence on rehabilitation services and the emotional and social cognition alterations underlying the pandemic. Based on these elements, the authors suggested a series of recommendations for the management of these patients suffering from COVID-19. The recommendations are were made by the International Society for Movement Disorders and Parkinson’s Disease and the Specialized Committee on Neurogenetics belonging to the Chinese Medical Association [23], as well as by expert consensus on the management strategy of patients with hereditary ataxia during the prevention and control of the novel coronavirus pneumonia epidemic [24]: (1) Maintain the usual treatments, such as vitamin therapy, antioxidants, and others, according to the type of ataxia; (2) maintain physical–motor rehabilitation in a systematic way, fundamentally based on coordination, balance, and walking exercises in their own homes; (3) increase sleep hygiene measures to achieve restful sleep that should not exceed 8 h; (4) carry out relaxation strategies, such as meditation or yoga, in addition to associating the above with listening to relaxing music and maintaining a very optimistic state of mind; (5) maintain communication by telephone with specialist doctors, either at the ataxias center or in the health areas, and, in the event of a suspicious respiratory manifestation, go to the family doctor.
2.3. Cerebrovascular Disease and COVID-19
Cerebrovascular disease is the topic of a review article by Bender et al. [25]. Cerebrovascular diseases constitute a global health problem due to their incidence, prevalence, and mortality. In this research, the casuistry and reports of cases that have been described up to the time of writing and an analysis of the possible pathophysiological implication were included. Attention was drawn to the reduction in reported cases of cerebrovascular disease without casuistic support and alerts about its presentation and related risk factors. Relevant considerations of Morelli and collaborators from the Guglielmo da Saliceto Hospital in Piacenza, Milan, Italy, were shown in this research [25]. Ischemic accidents were described in cerebrovascular disorders as having almost disappeared from stroke units. The authors were of the opinion that the significant reduction in currently registered cerebrovascular accidents can be attributed to the fact that fewer people go to the hospital for fear of becoming infected, although this may be true only for mild and non-disabling cases. Brain bleeds are always disabling, and it is impossible to avoid hospitalization with such a serious condition. A hypothesis put forward by the authors refers to the fact that the increased risk of these vascular events could be related to the controversial role attributed to IL-6 in stroke, whose high levels have a negative effect on the volume of the cerebral infarct in the long term [25]. On the contrary, IL-6 has a protective effect in ischemic stroke that helps improve post-stroke angiogenesis. On the other hand, the presence of thrombocytopenia in patients with mild COVID-19 raises the question of whether decreased platelet levels have an impact on the reduction of strokes. The evidence-based answer stated that the burden of persistent chronic infections or past infections appears to be associated with the risk of stroke [25].
González-García et al. also wrote about some published studies related to the frequency of strokes in patients infected with the virus, which is considered to be between 5 and 20% of COVID-19 cases. They reported that, although the pathophysiological mechanisms by which a stroke can occur in these patients are still unknown, cases of SARS-CoV-2 infection associated with a prothrombotic state capable of causing arterial and venous thromboembolism have been described. In addition, it was argued that an exacerbated inflammatory response with recruitment of blood cells and disproportionate secretion of proinflammatory cytokines constitutes the biological basis of this process. In addition, hypoxia and cardioembolic phenomena were proposed as possible mechanisms. However, the conclusive criterion is the essential need to accurately define the pathophysiological mechanisms that link SARS-CoV-2 infection with the occurrence of stroke and the need to apply more specific treatments to avoid future complications [26].
Based on the impact of dementia in Latin American and Caribbean countries (LACs) and vulnerable populations, Ibanez and col. described, using an underscore report, the impact of SARS-CoV-2 on dementia among LACs, the specific strain on health systems devoted to dementia, and the subsequent effect of increasing inequalities among those with dementia in the region, and also called attention to the implementation of best practices for mitigation and containment, which are facing particularly steep challenges in LACs. They also advised on the necessity for a coordinated action plan, including the development of inexpensive mass testing and multilevel regional coordination for dementia care and related actions. Brain health diplomacy should lead to a shared and escalated response across the region, coordinating leadership, and interaction between governments and international multilateral networks [27].
3. Psychoneuroimmunology and COVID-19
The durability of COVID-19 worldwide and its impact outside the respiratory system makes it necessary to implement programs that allow the patient to be assessed as a biopsychosocial being in the search for better diagnostic and treatment strategies; in this context, psychoneuroimmunology approaches are necessary for the achievement of more humanistic medicine.
From this perspective, Monet and cols. reported on cases that occurred in Santiago de Cuba, a province in the eastern part of the country, after 11 March 2020. Early in the pandemic, attention was focused on the acute morbidity and mortality associated with COVID-19, whereas months later persistent physical and neuropsychiatric squeals were described after SARS-CoV-2 infection. The authors reported that, although residual or persistent neuropsychiatric symptoms are not uncommon in survivors, post-COVID-19 follow-up revealed a mild and/or asymptomatic infection responsible for cognitive impairment, delirium, extreme fatigue, and relevant mood symptoms, probably as result of the interaction between multiple factors: the nervous, endocrine, and immune systems, with the last one also involving a visceral stress response, with an impact on mental health, favoring the psychological manifestations linked to the severity of the somatic and psychiatric symptoms [28].
The neuropsychiatric manifestations of COVID-19 have an impact in the context of this pandemic due to their frequency and based on the clinical status of the patients. In this aspect, the authors referred in this research to the impact of comorbidities and the appearance of neuropsychiatric manifestations and followed the idea of comorbid states, such as immunodeficiencies, obesity, and autoimmune diseases, showing association with cognitive deterioration and Alzheimer’s disease, as well as with more severe forms of the disease. These states can also give rise to immunodeficiency due to their action on the hypothalamus–pituitary–adrenal axis and to the increase in cortisol levels. In addition, increased levels of cytokines (IL-6, IL-4, IL-10, and TNF-alpha) and proteins associated with CNS damage and neurotransmitters (epinephrine and serotonin) have been observed in psychiatric conditions such as schizophrenia and depression, which reinforces the role of the neuroendocrine axis as a relevant hypothesis in the occurrence of these disorders related to SARS-CoV-2 infection [27][29]. Similarly, increased levels of some biomarkers associated with CNS damage, such as the S100 B protein (protein calcium-binding B) and fibroglial acid protein (GFAP) have been observed during these post-COVID-19 neuropsychiatric manifestations [30].
4. COVID-19 and Autoimmune Diseases
Based on the experiences published by Noris and col, the authors emphasized that the best way to approach post-COVID-19 neuropsychiatric disease is a comprehensive and holistic approach. They considered that the latter helps to reduce the associated factors related not only to the possibility of contagion but also to the development of emotional manifestations that lead to greater vulnerability to contraction and to short- and long-term repercussions of the disease. Among the sequelae of SARS-CoV-2 infection, autoimmune diseases related to frequency of appearance and crises stand out [31]. In this sense, systemic lupus erythematosus (SLE) deserves special interest: Neuropsychiatric manifestations in patients with COVID-19 may be the result of CNS damage, aggravated by infection by this neurotrophic virus and/or by the ability of the virus to induce the appearance of SLE as a post-COVID-19 neuropsychiatric manifestation. In these cases, a research experience by Noris et al. demonstrated that the quantification of the S100B level is an useful variable in the early identification or diagnosis of these neuropsychiatric manifestations in the course of infection or after damage to the post-COVID-19 CNS [30] (Figure 1).
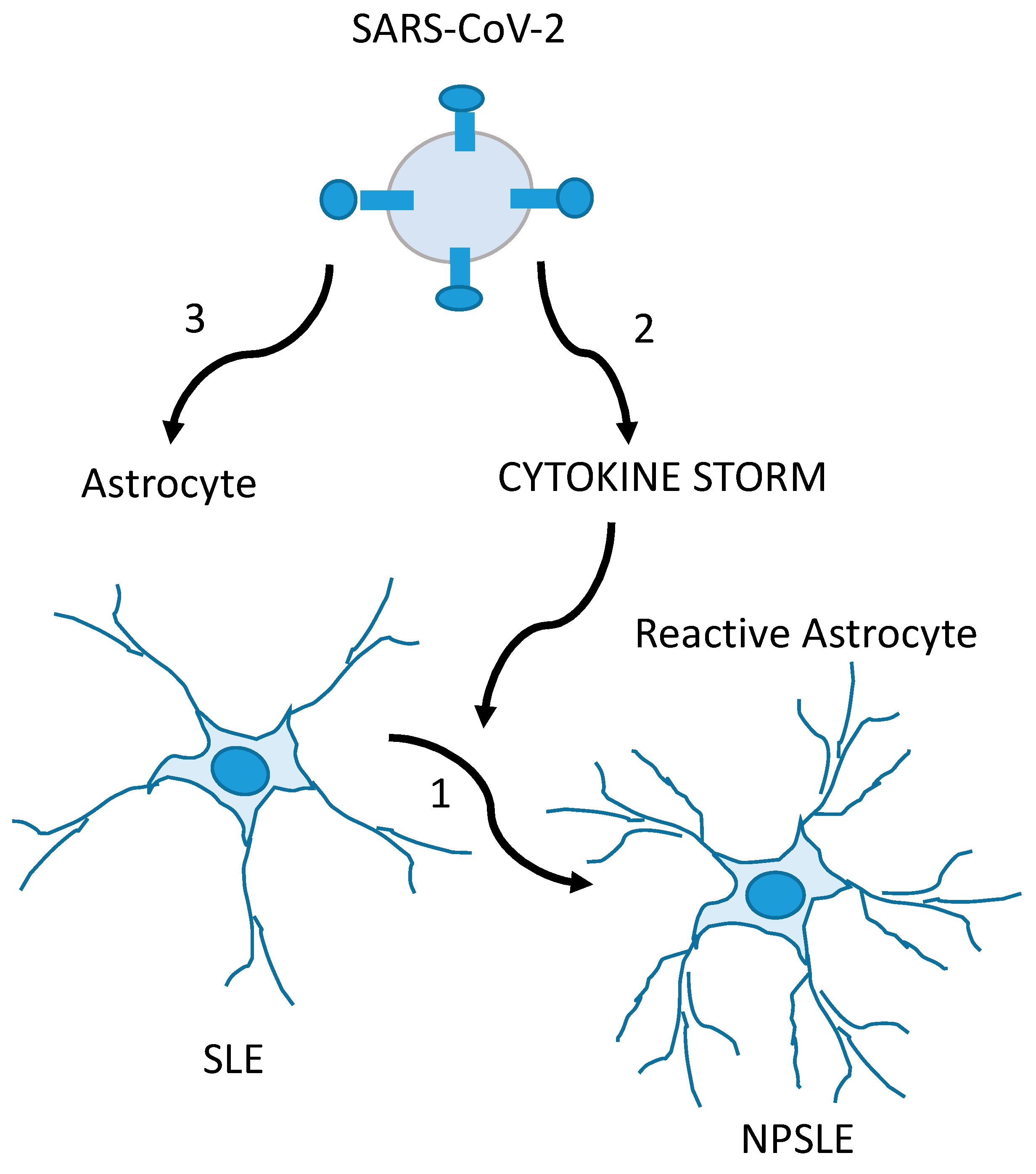
Figure 1. Glia-mediated neuropsychiatric manifestations in SLE (NPSLE) patients with COVID-19 are possibly caused by the CNS involvement of SLE and exacerbated by SARS-CoV-2. In the first mechanism, SLE triggers inflammatory events on normal-functioning astrocytes in the CNS, producing the glial hyper-reactivity (increase in GFAP levels and S100B secretion) found in NPSLE (1). In the second condition, the SARS-CoV-2-induced cytokine storm (together with hypoxemia and thrombotic events) causes glial reactivity, overlapping or not with mechanism 1 (2). In the third mechanism, SARS-CoV-2 is the direct cause of the glial reactivity, overlapping or not with mechanism 1 (3). Adapted from [30], with permission from Elsevier (license # 5586971171821).
References
- Aguiar, A.M.; Roque, L.; Morejón, M. Neurological manifestations in patients with COVID-19. Univ. Méd. Pinareña 2022, 18, e675.
- Moreno-Zambrano, D.; Arévalo-Mora, M.; Freire-Bonifacini, A.; García-Santibanez, R.; Santibañez-Vásquez, R. Manifestaciones neurológicas asociadas a la infección por SARS-CoV-2: Una neuro-revisión de COVID-19. Rev. Ecuat. Neurol. 2020, 29, 115–124.
- Rodriguez, A.J.; Cardona, J.A.; Gutiérrez, E.; Villamizar, R.; Holguin, Y.; Escalera, J.A.; Alvarado-Arnez, L.E.; Bonilla-Aldana, D.K.; Franco-Paredes, C.; Henao-Martinez, A.F.; et al. Clinical, laboratory and imaging features of COVID-19: A systematic review and meta-analysis. Travel Med. Infect. Dis. 2020, 34, 101623.
- Aldámiz, M.T.; Aledo, A.; Hernández, M.; Catalán, P.; Díez, C.; Martínez, E. COVID-19 Manual for the General Neurologist; SEN Editions: Madrid, Spain; Spanish Society of Neurology: Madrid, Spain, 2020; ISBN 978-84-946708-3-1.
- Xu, X.W.; Wu, X.X.; Jiang, X.G.; Xu, K.J.; Ying, L.J.; Ma, C.L.; Li, S.B.; Wang, H.Y.; Zhang, S.; Gao, H.N.; et al. Clinical fidings in a group of patients infected with the 2019 novel coronavirus (SARS-CoV-2) outside of Wuhan, China: Retrospective case series. BMJ 2019, 19, 368.
- León., R.; Bender, J.E.; Velázquez, L.C. Affectation of the nervous system by COVID-19. Ann. Cuba Acad. Sci. 2020, 10, 2.
- León, R.; Bender, J.E.; Velázquez, L.C. Olfactory dysfunction and COVID-19. Ann. Cuba Acad. Sci. 2020, 10, 2.
- Zhang, P. Be Cautious of Comorbidities of COVID-19 and Neurologic Diseases. Neurology Blogs. 2020. Available online: https://blogs.neurology.org/global/invited-commentary-be-cautious-of-comorbidities-of-COVID-19-and-neurologic-diseases/ (accessed on 6 September 2023).
- Li, Y.; Li, M.; Wang, M.; Zhou, Y.; Chang, J.; Xian, Y.; Wang, D.; Mao, L.; Jin, H.; Hu, B. Acute cerebrovascular disease following COVID-19: A single center, retrospective, observational study. Stroke Vasc. Neurol. 2020, 5, 279–284.
- Kempuraj, D.; Thangavel, R.; Kempuraj, D.; Ejaz, M.; Selvakumar, G.; Raikwar, S. Neuroprotective effects of flavone luteolin in neuroinflammation and neurotrauma. BioFactors 2020, 47, 190–197.
- Pentón, G.; Marín, J.; McCarty, M.F. C-Phycocyanin-derived Phycocyanobilin as a Potential Nutraceutical Approach for Major Neurodegenerative Disorders and COVID-19- induced Damage to the Nervous System. Curr. Neuropharmacol. 2021, 19, 2250–2275.
- Machado, C.; DeFina, P.A.; Chinchilla, M.; Machado, Y.; Machado, Y. Brainstem Dysfunction in SARS-CoV-2 Infection can be a Potential Cause of Respiratory Distress. Neurol. India 2020, 68, 989–993.
- Welge, A. Impaired sense of smell and taste. Therapy options in anosmia and dysgeusia. Laryngorhinootologie 2005, 84, S92–S100.
- Haehner, A.; Hummel, T.; Reichmann, H. A clinical approach towards smell loss in parkinson’s disease. J. Park. Dis. 2014, 4, 189–195.
- Anosmia and Ageusia as Initial or Unique Symptoms after SARS-CoV-2 Virus Infection. Available online: https://www.preprints.org/manuscript/202004.0272/v1 (accessed on 6 September 2023).
- Robinson, M.A.; Gonçalves, C.A.; Noris, E.; Rivero, N.P.; Brigida, A.L.; Schultz, S.; Siniscalco, D.; García, R.J.G. Impact of SARS-CoV-2 on neuropsychiatric disorders. World J. Psychiatry 2021, 11, 347–354.
- Robinson, M.A.; González, M.E.; Bergado, M.E. Autism, developmentand neural plasticity. In Translational Approaches to Autism Spectrum Disorder; Robinson Agramonte, M.A., Ed.; Springer: Berlin/Heidelberg, Germany, 2015; pp. 119–135.
- Lorigados, L.; Pavón, N. COVID-19 and neurological conditions. Panor. Cuba Health 2021, 16, 87–96.
- Bender, J.E.; Mendieta, M.; León, R.; Hernandez, L. Psychiatric manifestations in relation to SARS-CoV-2 infection. Ann. Cuba Acad. Sci. 2020, 10, 923.
- Valdés, M.J.; López, Á.; Palermo, F.J.; Martínez, I.; Martín, V.E.; Crespo, B.; Ruiz, M. Reactive psychoses in the context of the COVID-19 pandemic: Clinical perspectives from a case series. Rev. Psiquiatr. Salud Ment. 2020, 13, 90–94.
- Bender, J.E.; Mendieta, M.; León, R.; Hernandez, L. Epilepsy and COVID-19. Ann. Cuba Acad. Sci. 2020, 10.
- Bender, J.; Pedroso, M.D.; León, R.; Chacón, L. Epileptic Crisis, Epilepsy and COVID-19. EC Neurology 2021, 13, 8–18. Available online: https://www.ecronicon.com/ecne/pdf/ECNE-13-00845.pdf (accessed on 6 September 2023).
- Velázquez, L.; Vázquez, Y.; Rodríguez, R. Hereditary ataxias and COVID-19: Possible pathophysiological implications and recommendations. Ann. Cuba Acad. Sci. 2020, 10, e801. Available online: https://revistaccuba.sld.cu/index.php/revacc/article/view/801/830 (accessed on 6 September 2023).
- Specialized Committee of Neurogenetics Neurophysician Branch of Chinese Medical Doctor Association; Jiang, H.; Tang, B. Expert consensus on the management strategy of patients with hereditary ataxia during prevention and control of novel coronavirus pneumonia epidemic. Zhonghua Yi Xue Yi Chuan Xue Za Zhi 2020, 37, 359–366.
- Bender, J.E.; Mendieta, M.; León, R.; Hernandez, L. Cerebrovascular disease and COVID-19. Ann. Cuba Acad. Sci. 2020, 10, 1170–1172.
- Gonzalez, S.; Garófalo, N.; González, A.; Mezquia, N. COVID-19 infection and stroke. Cuba J. Biomed. Res. 2021, 40, E884.
- Ibanez, A.; Santamaria, H.; Guerrero, A.; Kornhuber, A.; Ton, A.M.M.; Slachevsky, A.; Teixeira, A.L.; Mar Meza, B.M.; Serrano, C.M.; Cano, C.; et al. The impact of SARS-CoV-2 in dementia across Latin America: Acall for an urgent regional plan and coordinated response. Alzheimer’s Dement. 2020, 6, e12092. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7683959/ (accessed on 6 September 2023).
- Monet, E.D.; Gross, V.Y.; Alvarez, J.T. COVID-19 from the perspective of Psychoneuroimmunoendocrinology. Ann. Cuba Acad. Sci. 2022, 12.
- Noris, E.; Robinson, M.A. Psychoneuroimmunoendocrinology and COVID-19. Electron. Mag. Dr. Zoilo E Mar. Vidaurreta 2021, 46, 2523. Available online: https://revzoilomarinello.sld.cu/index.php/zmv/article/view/2523 (accessed on 6 September 2023).
- Noris, E.; Robinson, M.A.; Gonçalves, C.A. Utility of serum s100b as a marker in systemic lupus erythematosus. Patients during and after the SARS-CoV-2 pandemic. Arch. Med. Res. 2022, 53, 543–544.
- Diaz, A.; Peláez, A.A.; Fuentes, M.; Cabrera, M.N.; Goncalves, C.A.; Schultz, S.; Siniscalco, D.; Robinson, M.A. SARS-CoV-2 Infection and Risk Management in Multiple Sclerosis. Diseases 2021, 9, 32.
More
Information
Subjects:
Neurosciences
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
604
Revisions:
3 times
(View History)
Update Date:
12 Oct 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




