Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | kıvanç of kamburoğlu | -- | 2315 | 2023-08-28 12:26:11 | | | |
| 2 | Rita Xu | Meta information modification | 2315 | 2023-08-29 04:42:09 | | | | |
| 3 | Rita Xu | Meta information modification | 2315 | 2023-08-30 09:38:20 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Ozsari, S.; Güzel, M.S.; Yılmaz, D.; Kamburoğlu, K. Temporomandibular Joint Related Diseases. Encyclopedia. Available online: https://encyclopedia.pub/entry/48534 (accessed on 08 February 2026).
Ozsari S, Güzel MS, Yılmaz D, Kamburoğlu K. Temporomandibular Joint Related Diseases. Encyclopedia. Available at: https://encyclopedia.pub/entry/48534. Accessed February 08, 2026.
Ozsari, Sifa, Mehmet Serdar Güzel, Dilek Yılmaz, Kıvanç Kamburoğlu. "Temporomandibular Joint Related Diseases" Encyclopedia, https://encyclopedia.pub/entry/48534 (accessed February 08, 2026).
Ozsari, S., Güzel, M.S., Yılmaz, D., & Kamburoğlu, K. (2023, August 28). Temporomandibular Joint Related Diseases. In Encyclopedia. https://encyclopedia.pub/entry/48534
Ozsari, Sifa, et al. "Temporomandibular Joint Related Diseases." Encyclopedia. Web. 28 August, 2023.
Copy Citation
With rapid advances in technology, computer-based studies and Artificial Intelligence (AI) approaches are finding their place in every field, especially in the medical sector, where they attract great attention. The Temporomandibular Joint (TMJ) stands as the most intricate joint within the human body, and diseases related to this joint are quite common.
temporomandibular joint
temporomandibular joint diseases
artificial intelligence
1. Introduction
In recent years, technology has experienced rapid advancements, and its widespread application now touches almost every domain. The ability to perform numerous tasks online has significantly increased the amount of data being generated daily. To efficiently process this data, make automated inferences, and minimize reliance on human intervention, the adoption of artificial intelligence-based approaches becomes unavoidable.
AI can be defined as the process of transferring human intelligence to computers, while ML, a sub-field of AI, involves making inferences by learning from data. In recent years, Deep Learning (DL) approaches, a sub-field of Machine Learning (ML), have demonstrated remarkable effectiveness in various domains, including image processing, object detection, and classification. These DL techniques have also been applied in dentistry, as evidenced by studies such as [1][2][3][4][5][6]. The primary reason why deep learning architectures receive significant attention is their ability to automatically learn from diverse types of data, including images, signals, videos, and texts.
The ML and DL methodologies utilized in the research researchers examined were not explained in detail. For a more comprehensive understanding of these methods, researchers included two publications in the references [7][8], which provide general information about ML and DL algorithms. Researchers can refer to these and similar studies to obtain more in-depth information about the methodologies employed. The temporomandibular joint binds the mandible or lower jaw to the skull and is a complicated, delicate, and mobile joint [9]. The TMJ controls the movement of the jaw. The anatomy of the TMJ can be observed in Figure 1. Temporomandibular joint diseases, often related to muscles, are quite common. They present with various symptoms, including face, head, or jaw pain, and joint-induced sounds.
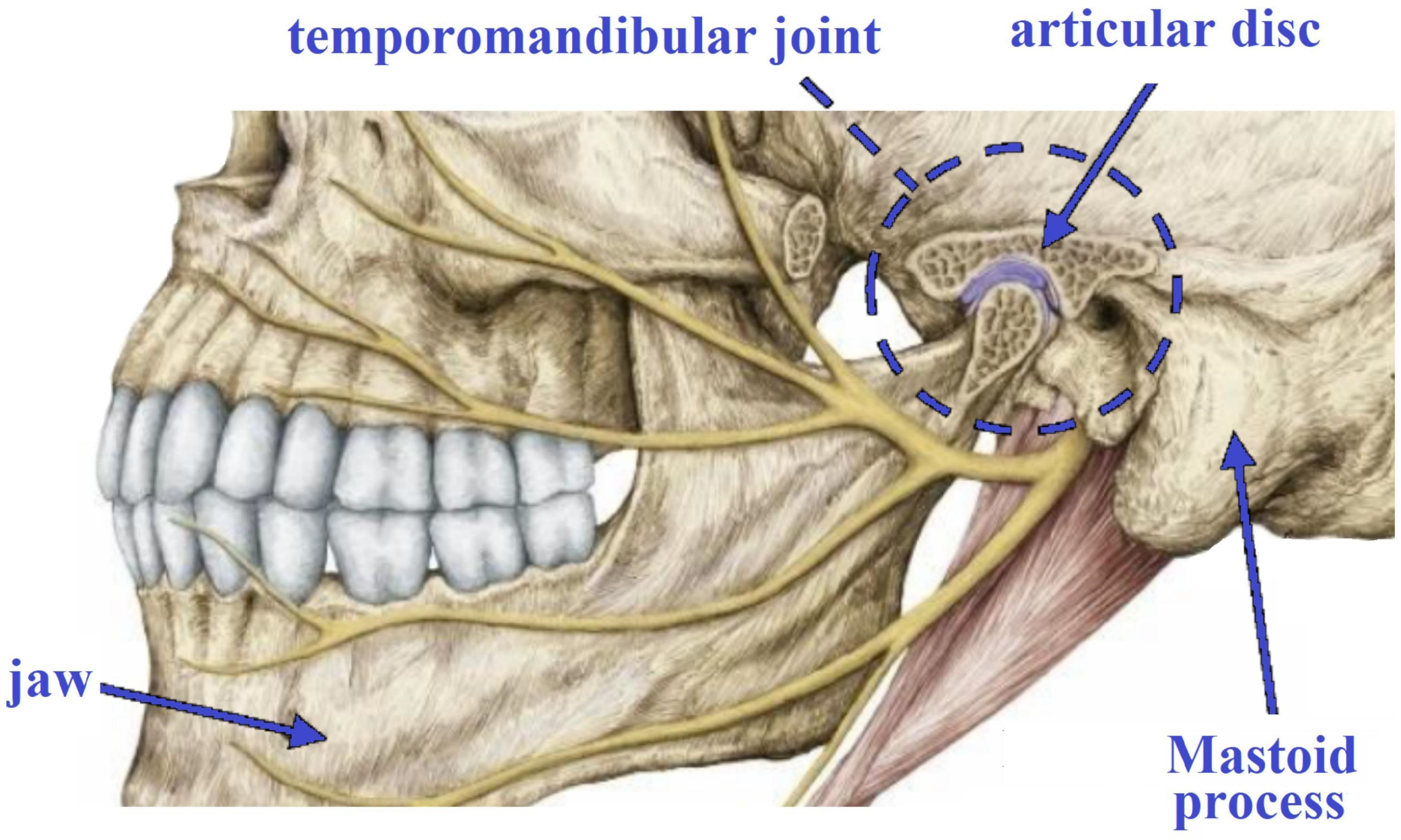
Figure 1. Anatomy of TMJ.
TMJ-related diseases are typically diagnosed through a patient’s clinical examination, anamnesis, and the interpretation and reporting of images by a radiologist. Nonetheless, this process can incur costs and consume a significant amount of time. To address this challenge, an automated system can be employed to assist physicians in the diagnosis process. Computer-aided approaches, especially those based on artificial intelligence, machine learning, and deep learning algorithms, have shown great promise in effectively tackling such diagnostic problems.
2. Fundamentals of TMJ
2.1. Diseases and Diagnostics
The temporomandibular joint is a sophisticated joint comprising different elements, such as bones, cartilage, ligaments, muscles, and a small cushioning disc between the bones. Its intricate structure and frequent use make it vulnerable to various issues and disorders. TMJ-related diseases encompass a range of medical conditions affecting the TMJ and its associated structures. These conditions can lead to jaw joint pain, dysfunction, and discomfort in the surrounding areas. Some of the typical TMJ-related diseases include TMD, TMJ OA, and JIA.
TMD is a comprehensive label that includes different conditions impacting the TMJ, such as joint inflammation, disc displacement, and degenerative alterations. These conditions can lead to symptoms such as jaw pain, restricted jaw movement, clicking or popping noises, and muscle stiffness. TMD is more common in individuals between the ages of 20 and 40, and it is also more prevalent in women than in men [10][11][12][13]. TMJ osteoarthritis is a degenerative joint condition marked by the deterioration of the cartilage within the TMJ. This ailment can result in discomfort, swelling, and limited jaw mobility. JIA is a chronic inflammatory condition that can impact the TMJ in children and adolescents. This disease may lead to joint pain, swelling, and deformities, potentially affecting jaw function.
The diagnosis of TMJ-related diseases requires a thorough evaluation by a healthcare professional, commonly a dentist, oral and maxillofacial surgeon, or orofacial pain specialist. The assessment typically encompasses medical history analysis, clinical examination, and the use of imaging techniques. The diagnosis process may include the following steps:
-
Gathering Medical History: the healthcare professional will start by obtaining a comprehensive medical history from the patient, including any past jaw-related problems, dental procedures, or recent injuries that could be pertinent to the current symptoms.
-
Comprehensive Clinical Assessment: a detailed examination of the jaw, face, head, and neck will be performed to evaluate the extent of movement, joint sounds, tenderness, and any indications of inflammation or swelling.
-
Diagnostic Imaging: X-rays, Computed Tomography (CT) scans, or Magnetic Resonance Imaging (MRI) can be employed to capture detailed images of the TMJ and adjacent structures. These imaging modalities have the capability to detect any irregularities, such as joint degeneration, disc displacement, or fractures [14].
-
Occlusion Assessment: the dentist will examine how the upper and lower teeth fit together (occlusion) to identify any malocclusion or teeth alignment issues that may contribute to TMJ problems.
-
TMJ Function Tests: specific tests will be conducted to assess the functioning of the TMJ and jaw muscles. These tests aid in detecting any limitations or irregularities in jaw movement.
-
Palpation: a gentle examination of the jaw area will be performed to locate tender points or areas of muscle tension.
-
Pain and Symptom Evaluation: the patient will be asked about the location, intensity, and duration of pain, as well as any accompanying symptoms such as headaches or earaches.
-
Exclusion of Alternative Causes: due to the potential overlap of TMJ-related symptoms with other conditions, the healthcare provider will carefully eliminate other potential causes of jaw pain or dysfunction.
Rapid completion of the diagnostic process is vital for effective treatment. Automated systems are well-suited for addressing such concerns. This research focused on investigating computer-based methods used for TMJ-related diseases, as previously mentioned. All diseases were searched using the following keywords: “artificial intelligence”, “machine learning”, and “deep learning”. For instance, the search terms used were “temporomandibular joint artificial intelligence”, “temporomandibular joint machine learning”, “temporomandibular joint deep learning”, “temporomandibular joint disorders artificial intelligence”, “temporomandibular joint disorders machine learning”, and “temporomandibular joint disorders deep learning”. Similar combinations were used for other diseases, such as TMJ OA, and JIA, during the screening process.
2.2. Independent Variables and Data Capturing
The TMJ is a complex joint that plays a crucial role in various functions, and several independent variables can influence the development and health of the temporomandibular joint. These variables can include demographic factors (age, gender, ethnicity, and socioeconomic status), medical history, lifestyle habits (teeth grinding (bruxism), clenching, nail-biting, or chewing gum), genetic predispositions, and various other biological and environmental factors. Understanding these variables helps in developing comprehensive models for the early detection and diagnosis of TMDs. Farook et al. [15] explored the digitization of jaw movement patterns using devices and analyzed how physiological factors and device-specific variables influenced jaw movements. The outcomes of their study demonstrated that factors such as mandibular and condylar growth, kinematic irregularities in the neuromuscular system, reduced dental arches, previous orthodontic interventions, variations in habitual head posture, TMDs, fricative phonetics, partially parafunctional habits, and imbalanced occlusal contact played a role as influencing factors on jaw movement paths as variables that could cause complications. However, these factors showed limited correlation with age, gender, or dietary habits.
TMJ image capture involves obtaining detailed images of the temporomandibular joint using various advanced imaging methods. X-rays, CT scans, MRIs, and Cone Beam Computed Tomography (CBCT) are commonly employed to visualize the TMJ and its associated structures. X-rays provide two-dimensional images that allow visualization of the bones and aid in identifying joint degeneration, osteoarthritis, or structural abnormalities in the joint. CT scans offer three-dimensional images, enabling a more comprehensive assessment of the TMJ’s bony structures, cartilage, and surrounding tissues. MRI, on the other hand, provides detailed soft tissue images, making it suitable for detecting disc displacement, inflammation, and joint effusion. CBCT combines the advantages of CT and panoramic X-rays, delivering high-resolution 3D images with reduced radiation exposure compared with traditional CT scans. These advanced imaging techniques play a crucial role in diagnosing TMJ-related diseases and guiding treatment decisions, as they provide essential information about the joint’s anatomy, function, and any potential abnormalities.
In the context of MRI, images of patients’ bilateral temporomandibular joints are typically captured in both sagittal and coronal oblique planes, with the jaw in both open and closed positions. This imaging is facilitated through the use of specific sequences, such as T1-weighted, MERGE, and Proton Density (PD) sequences. Within the realm of MR images focusing on the temporomandibular joint, comprehensive insights are drawn bilaterally. Experienced radiologists assess critical aspects such as the positioning of the disc, the identification of degenerative changes in the joint’s osseous structures, and the determination of effusion presence. This assessment involves the meticulous interpretation of slices ranging from 1 to 3 mm in thickness. The application of Magnetic Resonance Imaging devices operating at strengths of 1.5 to 3 Tesla yields detailed depictions of the intricate structures comprising the TMJ. Notably, the articular disc, an essential component of the TMJ, manifests as a distinctive biconcave image with a discernible low signal intensity in MRG. The mandibular condylar bone marrow showcases its characteristics in various sequences. Specifically, it produces a uniformly high signal intensity image in both T1-weighted and PD-weighted sequences while presenting a moderately graded signal intensity image in T2-weighted sequences. Conversely, bone marrow edema is visually indicated through low signal intensity in T1-weighted or PD-weighted sequences, and a contrastingly high signal intensity in T2-weighted sequences. In the domain of TMJ-related conditions, the presence of sclerosis and fibrosis is highlighted through the projection of low signal intensity images in T1-weighted, PD-weighted, and T2-weighted sequences. In contrast, osteonecrosis showcases a heterogeneous signal image, distinguishing itself from the other conditions under investigation [16][17][18].
In the realm of tomographic imaging, for a comprehensive radiographic assessment of the TMJ, it is imperative to execute two distinct scans, specifically in the closed and open mouth positions. The closed-mouth scan serves the purpose of establishing the functional position of the condyle within the mandibular fossa, a position defined by dental criteria. Depending on the clinician’s preference, the initial imaging should exhibit a medium level of resolution (with a nominal voxel size of 0.3 mm or smaller), while ensuring that the teeth are aligned in either maximum intercuspidation or centric relation. The field of view (FOV) should stretch roughly 1 cm above the glenoid fossa’s foundation (approximately at mid-orbital level), including the mandibular dentition, for the purpose of validating the occlusal alignment of the teeth. When there are concerns regarding alterations on the joint surface, it is advisable to enhance the voxel resolution (using a nominal voxel size of 0.25–0.125). To counteract the potential loss of cortical definition due to motion artifacts, it is crucial to maintain the stability of the patient’s head during the scanning process. The open mouth scan, on the other hand, serves to ascertain the extent of motion of the condylar head during mouth opening. For this purpose, a low-resolution scan with a reduced dose should be performed, employing a narrow FOV that encompasses the glenoid fossa base and the neck of the moving mandibular condyle. Ensuring the stability of the patient’s jaw is paramount during this open-scan phase. During the image reformatting process, adopting a standardized approach is indispensable to reconstructing and exhibiting the anatomical alterations in the shape and size of the TMJ’s bone components using sectional images. This method effectively minimizes discrepancies arising from parallax on the image screen and simplifies the comparison process across diverse patients or even across varying time intervals within the same patient. Protocols devised for the reformatting of TMJ images should guarantee a comprehensive assessment of articulation in standardized jaw positions (such as closed or open mouth), effectively preventing any instances where vital diagnostic information could be inadvertently disregarded. Opting for a TMJ protocol for radiological examination does not preclude the possibility of generating additional images, such as volumetric or shaded surface displays and Maximum Intensity Projections (MIPs). The primary objective of this protocol is to establish the minimum approach essential for a comprehensive interpretation. The foundational basis for reconstructing TMJ images is the creation of Multiplanar Reformat (MPR) images, oriented obliquely sagittal (or parasagittal) to the line perpendicular to the axis or plane positioned between the medial and lateral poles of the condyle, as based on the axial plane [17][19].
The data collected for automated diagnosis of TMDs plays a crucial role in ensuring the accuracy and reliability of the diagnostic process. The type and quality of data utilized for training and testing machine learning or deep learning algorithms significantly influence the system’s performance in identifying and categorizing TMD-related conditions. Automated TMD diagnostics employ diverse data types, including clinical examination results, patient medical history, imaging data (e.g., X-rays, CT scans, MRI), and patient-reported symptoms. Each data type contributes unique information about the TMJ and its associated structures, allowing the algorithm to detect specific abnormalities and patterns. The quality of the data, encompassing accuracy, completeness, and relevance, is pivotal in building robust diagnostic models. The use of clean and reliable data minimizes the risk of false positives or false negatives and enhances the overall system performance. The dataset’s size utilized for training the algorithm is of utmost importance. Larger datasets often lead to more accurate and generalizable models, while a limited dataset may result in overfitting, where the algorithm performs well on the training data but fails to generalize to new, unseen data. Ensuring diversity in the dataset, encompassing a wide range of TMD-related cases, is crucial for enabling the algorithm to handle various conditions and manifestations. A diverse dataset prevents bias towards specific types of TMDs and improves the system’s ability to recognize fewer common disorders. Currently, researchers are actively exploring the potential of machine learning and deep learning algorithms to automate the diagnostic process for TMDs. Studies have extensively investigated various data types, such as radiographic images, clinical findings, and patient-reported symptoms, to develop accurate and effective diagnostic models.
References
- Kermany, D.S.; Goldbaum, M.; Cai, W.; Valentim, C.C.; Liang, H.; Baxter, S.L.; McKeown, A.; Yang, G.; Wu, X.; Yan, F.; et al. Identifying medical diagnoses and treatable diseases by image-based deep learning. Cell 2018, 172, 1122–1131.
- Woerl, A.C.; Eckstein, M.; Geiger, J.; Wagner, D.C.; Daher, T.; Stenzel, P.; Fernandez, A.; Hartmann, A.; Wand, M.; Roth, W.; et al. Deep learning predicts molecular subtype of muscle-invasive bladder cancer from conventional histopathological slides. Eur. Urol. 2020, 78, 256–264.
- Savitha, G.; Jidesh, P. A holistic deep learning approach for identification and classification of sub-solid lung nodules in computed tomographic scans. Comput. Electr. Eng. 2020, 84, 106626.
- Guo, J.; Zhu, J.; Du, H.; Qiu, B. A bone age assessment system for real-world X-ray images based on convolutional neural networks. Comput. Electr. Eng. 2020, 81, 106529.
- Yang, Z.; Liu, Z. The risk prediction of Alzheimer’s disease based on the deep learning model of brain 18F-FDG positron emission tomography. Saudi J. Biol. Sci. 2020, 27, 659–665.
- Saha, S.; Pagnozzi, A.; Bourgeat, P.; George, J.M.; Bradford, D.; Colditz, P.B.; Boyd, R.N.; Rose, S.E.; Fripp, J.; Pannek, K. Predicting motor outcome in preterm infants from very early brain diffusion MRI using a deep learning convolutional neural network (CNN) model. Neuroimage 2020, 215, 116807.
- Mahesh, B. Machine learning algorithms-a review. Int. J. Sci. Res. 2020, 9, 381–386.
- Shrestha, A.; Mahmood, A. Review of deep learning algorithms and architectures. IEEE Access 2019, 7, 53040–53065.
- Ingawale, S.; Goswami, T. Temporomandibular joint: Disorders, treatments, and biomechanics. Ann. Biomed. Eng. 2009, 37, 976–996.
- Detamore, M.S.; Athanasiou, K.A. Structure and function of the temporomandibular joint disc: Implications for tissue engineering. J. Maxillofac. Surg. 2003, 61, 494–506.
- Detamore, M.S.; Athanasiou, K.A.; Mao, J. A call to action for bioengineers and dental professionals: Directives for the future of TMJ bioengineering. Ann. Biomed. Eng. 2007, 35, 1301–1311.
- Van Loon, J.P.; De Bont, L.; Stegenga, B.; Spijkervet, F.; Verkerke, G. Groningen temporomandibular joint prosthesis. Development and first clinical application. J. Maxillofac. Surg. 2002, 31, 44–52.
- Warren, M.P.; Fried, J.L. Temporomandibular disorders and hormones in women. Cells Tissues Organs 2001, 169, 187–192.
- Okeson, J.P. Management of Temporomandibular Disorders and Occlusion-E-Book; Elsevier Health Sciences: Amsterdam, The Netherlands, 2019.
- Farook, T.H.; Rashid, F.; Alam, M.K.; Dudley, J. Variables influencing the device-dependent approaches in digitally analysing jaw movement—A systematic review. Clin. Oral Investig. 2023, 27, 489–504.
- Larheim, T.A.; Westesson, P.L.; Hicks, D.G.; Eriksson, L.; Brown, D.A. Osteonecrosis of the temporomandibular joint: Correlation of magnetic resonance imaging and histology. J. Oral Maxillofac. Surg. 1999, 57, 888–898.
- Yılmaz, D.; Kamburoğlu, K. Comparison of the effectiveness of high resolution ultrasound with MRI in patients with temporomandibular joint dısorders. Dentomaxillofacial Radiol. 2019, 48, 20180349.
- Yılmaz, D.; Kamburoğlu, K.; Arslan, R. Quantitative volume and area assessment of masticatory muscles through magnetic resonance imaging in patients with temporomandibular joint disorders. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2023, 135, 548–557.
- Tsiklakis, K.; Syriopoulos, K.; Stamatakis, H. Radiographic examination of the temporomandibular joint using cone beam computed tomography. Dentomaxillofacial Radiol. 2004, 33, 196–201.
More
Information
Subjects:
Dentistry, Oral Surgery & Medicine
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
748
Revisions:
3 times
(View History)
Update Date:
30 Aug 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




