Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Sonia Garrido Chamorro | -- | 2612 | 2023-08-09 16:00:00 | | | |
| 2 | Camila Xu | Meta information modification | 2612 | 2023-08-10 01:57:24 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Ibáñez, A.; Garrido-Chamorro, S.; Barreiro, C. Human Health and Climate Change. Encyclopedia. Available online: https://encyclopedia.pub/entry/47849 (accessed on 08 February 2026).
Ibáñez A, Garrido-Chamorro S, Barreiro C. Human Health and Climate Change. Encyclopedia. Available at: https://encyclopedia.pub/entry/47849. Accessed February 08, 2026.
Ibáñez, Ana, Sonia Garrido-Chamorro, Carlos Barreiro. "Human Health and Climate Change" Encyclopedia, https://encyclopedia.pub/entry/47849 (accessed February 08, 2026).
Ibáñez, A., Garrido-Chamorro, S., & Barreiro, C. (2023, August 09). Human Health and Climate Change. In Encyclopedia. https://encyclopedia.pub/entry/47849
Ibáñez, Ana, et al. "Human Health and Climate Change." Encyclopedia. Web. 09 August, 2023.
Copy Citation
Human health is also affected by climate change effects. According to the World Health Organization, the epidemiology of infectious diseases constantly fluctuates in response to environmental changes and interactions among pathogens, hosts, reservoirs and vectors.
climate change
microorganisms
fungi
bacteria
pests
diseases
1. Human Infective Diseases: Evolution and Expansion
Climate change can modify the relationship between humans and pathogens, thereby increasing their probability of contracting infections and diseases. Rising temperatures would modify the host immune system and boost the growth rate of pathogens, which supports their perpetuation and transfer [1][2] in a similar manner previously described for livestock. The most positively affected pathogens are those transmitted by vectors, food, air, water and other environmental agents [1]. Thus, the forecast for the near future is an increase in the infection transference and spread, as well as a change in the patterns of infectious pathologies due to rising temperatures, early changes of season and fluctuations in rainfall. For example, the spread of mosquito-borne diseases like dengue fever or Zika virus will be the result of increasing temperatures and changes in rainfall patterns, which lead to more breeding sites. In addition, infectious disease-causing pathogens are able to adapt to new climatic conditions that enhance their transmission and prevalence [3][4][5].
The impact of rising temperatures and the adaptation of pathogens to new conditions poses a significant threat, leading to the emergence of previously unrecorded human infectious diseases. A notable example is the Chikungunya virus, transmitted by mosquitoes, which causes fever and severe joint pain. Although it was initially identified in Tanzania in the 1950s, it has since spread to other parts of the world, including America and Asia [6][7]. Pathogens may develop thermotolerance as a survival mechanism in response to changing environmental conditions and their adaptation to new hosts. The acquisition of this thermotolerance involves various molecular and cellular mechanisms, such as (i) the activation of heat shock response genes encoding heat shock proteins (HSPs), (ii) DNA repair mechanisms, metabolic adaptations to optimize energy production and utilization at higher temperatures or (iii) gene regulatory network modulation and signaling pathways to coordinate the expression of heat-responsive genes [8]. As these pathogens adapt to higher temperatures, they acquire the ability to cross the mammalian endothermic barrier (which creates a zone of thermal inhibition to prevent infection), thereby adapting to the internal environment of the host. This, together with the increased population density of pathogens, poses a greater threat to human health and increases the likelihood of infection. For instance, certain strains of Vibrio, commonly found in coastal waters, have become more virulent in response to escalating ocean temperatures, leading to outbreaks of infections among individuals exposed to contaminated water or seafood. Additionally, pathogens preserved in Arctic permafrost may also resurface, causing diseases such as tularemia or anthrax, as old variants long forgotten by the immune system regain activity [9].
The effect of climate change on the expansion and proliferation of some human diseases is presented in this section based on their transmission manners (vector-borne, foodborne or waterborne diseases) (see Table 1 and Figure 1).
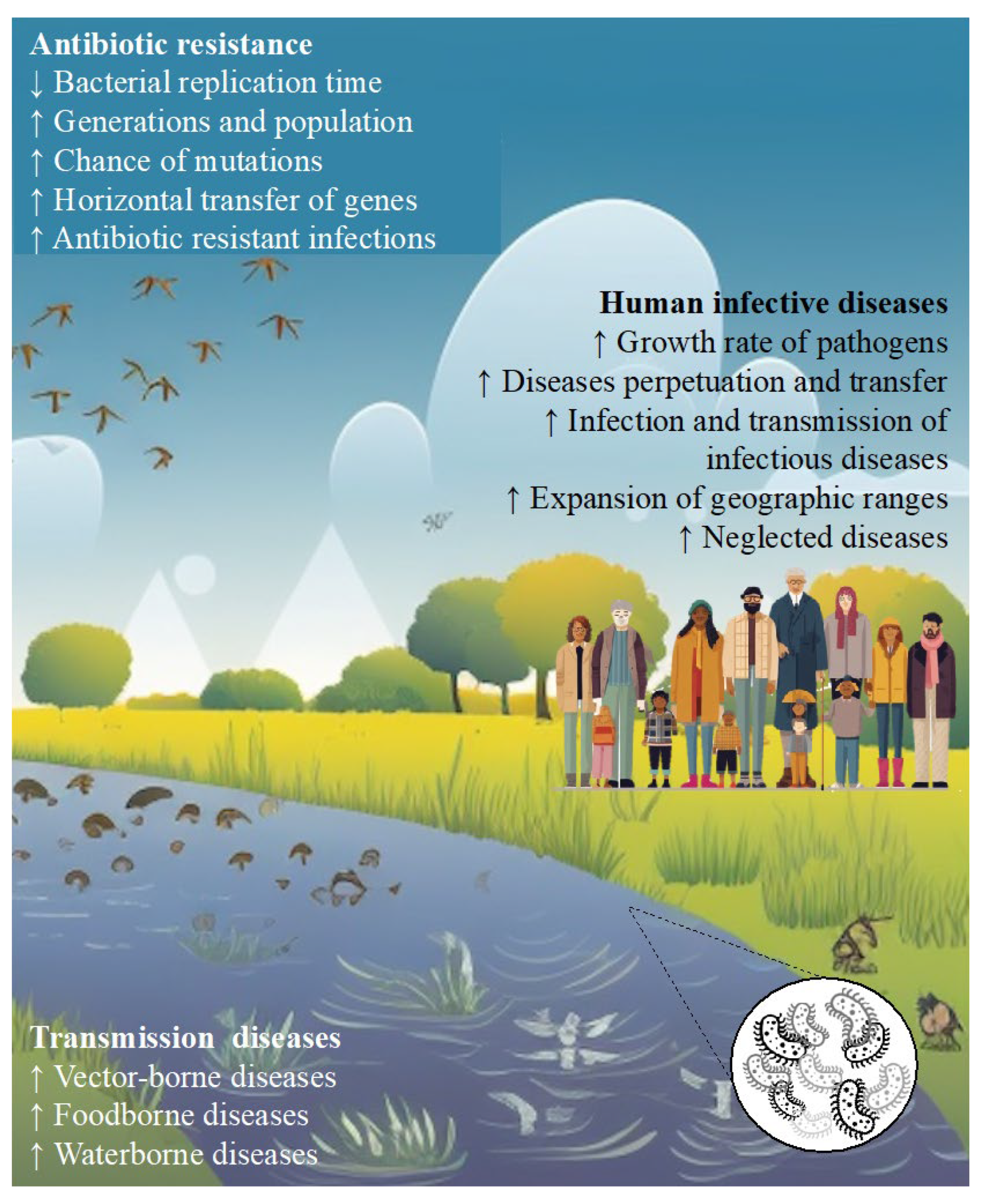
Figure 1. Summary of the main causes and effects of climate change on human health due to microbial global variations. White font: (up) factors that contribute to the worldwide increase in antibiotic resistance; (down) different sources of borne diseases. Black font: result on human health of the different factors presented in the manuscript.
1.1. Human Vector-Borne Diseases
The most important vector-borne diseases in Europe are caused by pathogens sensitive to climatic conditions because they are spread mostly by cold-blooded arthropods, which expand their geographic ranges owing to the effects of climate change (global warming, rainfall variations and extreme weather events) [1][9][10]. Vector-borne diseases account for more than 17% of all infectious diseases, causing 700,000 deaths every year worldwide. Although mosquitoes are the best-known disease vector in humans and animals, other arthropods, such as ticks, black flies, sandflies, midges, fleas and triatomine bugs, also act as relevant vectors and should be kept in mind [1][11][12][13].
The effects of climatic variations can be observed with the spread of some tropical diseases, such as dengue and Zika, both transmitted by mosquitoes of the Aedes family. Dengue transmission has increased since 1950 by 8.9% in the case of Aedes aegypti and by 15.0% when considering Aedes albopictus, reaching almost 4 billion people in over 128 countries at risk of contracting dengue [10][11][12][14]. In addition, there was a 50% increase between 2005 and 2015 in the number of deaths caused by dengue, which has become the most prevalent disease among travelers in Southeast Asia, surpassing malaria.
Table 1. Effect of climate change on the expansion and development of different diseases.
| Disease | Microorganism | Vector | Host | Origin | Spread and Development | Effects of Climate Change | Refs. | |
|---|---|---|---|---|---|---|---|---|
| Vector-borne diseases | Chikungunya | Chikungunya virus | Aedes albopictus | Human | Tanzania | Asia and Africa | Increase in temperatures, changes in rainfall and increase in the number and severity of extreme weather events multiply the risk and the ranges of infection and the spread of diseases | [11] |
| Dengue | Dengue virus (DENV) | Aedes aegypti | Human | Africa | Tropical and subtropical areas and Europe | [4][14] | ||
| Aedes albopictus | ||||||||
| Leishmaniasis | Leishmania spp. | Female sand-fly | Human | Africa | Southern countries of the European continent | [9][11] | ||
| Zika | Zika virus (ZIKV) | Aedes albopictus | Human | Africa | North America and South America | [9][11] | ||
| Foodborne diseases | Diarrheal disease | Campylobacter spp. | Contaminated food | Human | America | Worldwide | Temperatures rise favors the contamination of food by pathogens that cause diseases | [9][11] |
| Salmonellosis | Salmonella spp. | Contaminated food | Human | America | Worldwide | [11][15] | ||
| Waterborne diseases | Cholera | Vibrio cholerae | Contaminated water | Human | Asia and Africa | Africa, Asia and North America | Increased precipitation can wash pathogens into waterways, while rising sea temperatures activate impulses for pathogen spread and development | [16][17][18][19][20][21] |
| Leptospirosis | Leptospira spp. | Contaminated water | Human | Germany | Tropical and subtropical areas | Warmer temperatures and extreme weather events can create favorable conditions for the survival and persistence of Leptospira bacteria in the environment. Alterations in land use and deforestation can also increase human contact with animal reservoirs of leptospirosis | [1] |
Thus, a 30-fold increase in dengue incidence over the last 50 years, as well as an extension in the geographic area of this disease, is a clear warning sign. Hence, forecasts estimate the future expansion of dengue, which will increase the risk of infection in the global population [9][22]. Currently, the greatest concern is the mosquito A. albopictus, which can spread from temperate regions to higher altitudes. This mosquito species is known to transmit diseases such as chikungunya and Zika viruses, making its presence a cause for heightened attention and concern. Some studies have related the spread of outbreaks to an increase in total viral load with an increase in the number and range of vectors, which is directly related to climate change [11][22][23][24].
Leishmaniasis, which is transmitted in warm environments by protozoa of the Leishmania genus, is moving into regions that are now temperate as a result of climate change, including areas of southern Europe such as Italy, Greece and Spain, as well as regions in South America, such as Argentina and Brazil [25][26][27]. In this way, the reproduction and survival of protozoa are advantaged because although the number of protozoa per cell does not increase, the concentration of these protozoa in the environment rises, since warm temperatures enhance their reproductive cycle. This has resulted in an alarming growth of cutaneous leishmaniasis in areas where this protozoa was not previously detected (because temperatures were much lower before), such as the southern countries of Europe, especially in Mediterranean countries such as Spain, Italy, France and Greece [9][11][28].
The effectiveness of disease transmission by a vector depends on the time taken for the vector to become infectious after encountering an infected host. Higher temperatures play a significant role in boosting efficacy. When temperatures are higher, the time between contact with the infected host and the vector becoming infectious is shortened. This shorter timeframe results in higher vector concentrations. As a result, there are more opportunities for the vector to transmit the disease within its lifespan, thereby increasing the overall transmission potential. Hence, the spread of vector-borne diseases is favored by rising temperatures, lengthening transmission seasons, increasing pathogen replication in the vector and increasing geographic range [1].
1.2. Foodborne Diseases
Nowadays, more than 200 types of foodborne diseases have been reported, most of which could be affected by climate change [11][15]. Approximately 420,000 deaths per year are caused by foodborne diseases, and an increase is expected because rising temperatures favor food contamination and pathogen establishment in new temperate regions [11][15]. In addition, the more humid the environment, the greater the survival of pathogens (such as Trichinella spp. and Toxoplasma gondii) and parasite eggs, larvae and cysts. The rainfall rises and its intensity, as well as the increase in floods, favor crop and food contamination because the air bacterial concentration is increased after a drizzle. Additionally, after a flood, wastewater is more likely to overflow, causing contamination of fresh produce [5][29].
Several examples of climate change effects on foodborne diseases have been described, such as an increase in Campylobacter infections due to rising temperatures and intense rainfalls [30]. According to a study carried out by Kuhn and collaborators in 2020 [30], there is a possible increase of between 3 and 20% in cases of Campylobacter infections if climate change is not delayed. In addition, salmonellosis, transmitted by Salmonella species, which activates reproduction at high temperatures, is another relevant concern. Global warming has been linked to an increase in Salmonella infections, and it is estimated that every degree of temperature rise would cause a 5% to 10% increase in Salmonella infections [11][15][31]. Morgado and co-workers, in 2021 [32], showed a direct relationship between warm temperatures, increased rainfall (especially during extreme weather events) and a rise in diagnosed cases of salmonellosis. In this way, higher temperatures can lead to increased bacterial concentrations, potentially resulting in more severe cattle infections. This has significant implications for the food industry, as contaminated meat can contribute to outbreaks of salmonellosis in humans [33].
1.3. Waterborne Diseases
Increased rainfall can drive pathogens into waterways and overwhelm water treatment systems, causing different disease outbreaks. In addition, as presented in previous sections, the increase in sea temperature and salinity changes can cause the development and proliferation of numerous Vibrio species, such as Vibrio cholerae. Thus, it should be kept in mind that these temperature changes, no matter how small, can lead to significant alterations in host–pathogen relationships [4][11][31][34]. In addition, it must be considered that the spread and development of some pathogens (Vibrio cholerae, Cryptosporidium, Leptospira spp., etc.) can lead to the contamination of urban water, which can result in an increase in several diseases [35][36]. Most of these pathogens are transmitted by the fecal–oral route or indirectly through contaminated water, where they can survive for long periods, even though their nutrient access can be scarce [15][22]. An example is cholera disease, whose clinical impact has increased in recent years, mainly due to temperature and rainfall variations. In fact, it has been observed that each increased degree raises the risk of cholera infections by around 15–29% [22][37].
Other cases of waterborne infections are those caused by the toxic microalgae Vicicitus globosus (formerly Chattonella globosa), which contaminates the food chain through shellfish consumption. Hence, climate change has intensified the proliferation of this algae because of the increase in the concentration of CO2 in water, driving an upsurge in food poisoning outbreaks [1][38]. Ocean acidification has also been linked to the formation of toxic algal blooms. Some species of algae, including Emiliania huxleyi, produce toxins when their environment changes due to acidification. These blooms can lead to the accumulation of toxins in the food chain, causing harm to marine organisms and potentially even to humans who consume seafood [38].
2. Antibiotic Resistance
The World Health Organization indicates antibiotic resistance as “one of the greatest threats to global health, food security and development today” (https://www.who.int/en/news-room/fact-sheets/detail/antibiotic-resistance, accessed on 19 July 2023). In recent years, antibiotic resistance has risen sharply to become a public health problem, with 23,000 people dying annually as a result of antibiotic-resistant infections. This health threat has been due to the wide variety of antibiotic applications (e.g., human and animal health, growth promotion in food-producing animals, disease prevention, crop-disease control as pesticides) in the last 80 years [39]. Worldwide, antibiotic consumption rose by approximately 39% between 2000 and 2015, and it is estimated that it will continue to rise up to 200% in a few years. These data, which are worrying for public health, were reviewed by Jim O’Neill (UK Prime Minister commissioned the Review on Antimicrobial Resistance) in 2014 [40], who reported that deaths from untreatable infections could reach 10 million annually after 2050. In addition, there was a reminder a few years later in 2019 from the IACG (Interagency Coordinating Group on Antimicrobial Resistance) hosted by the WHO (World Health Organization) with contributions from FAO and OIE (Organization for Animal Health) [41].
Latest studies relate antibiotic resistance spread to temperature increase because bacterial duplication time is accelerated, multiplying the chance of mutations, the horizontal transfer of genes (some of them related to antibiotic resistance) and infectivity [1][40][42][43] (Figure 1). Particularly, this increase in resistance has been notably higher in southern Europe, where climate change has led to a rise in minimum temperatures. As a consequence of this temperature increase in these southern countries, the intensification of antibiotic resistance has increased from 0.33% to 1.2% per year [42]. Acinetobacter baumannii, Pseudomonas aeruginosa and Klebsiella pneumoniae are examples of this peculiar connection between temperature and antibiotic resistance, which is currently causing serious sequelae because some strains are hard to tackle with current antibiotic formulations [44][45]. In addition, the increase in deaths due to antibiotic-resistant strains of tuberculosis causes more than 2000 deaths annually [46].
Furthermore, it has been observed that the higher the temperature, the faster the new instances of resistance upsurge [42][47]. Thus, salmonellosis could increase both burden and morbidity due to global warming [48].
Another particular case is Candida auris, a new drug-resistant yeast species [46]. Its most enigmatic aspect is that it emerged simultaneously as a human pathogen on three continents in 2009, exhibiting antifungal agent resistance. One hypothesis is that the increase in environmental temperature increased the concentration of C. auris and favored the appearance of new mutations, including those for antibiotic resistance. In addition, seabirds acted as intermediate hosts and reservoirs, and it became a zoonotic disease after breaking the mammalian thermal barrier through adaptation to climate change. According to Casadevall’s conclusions [6], C. auris was the first human pathogen to appear as a result of climate change [6][46].
The increase in temperature leads to higher growth rates and enhanced survival of pathogens, resulting in higher population densities. This, in turn, leads to an increased number of pathogens, which subsequently contributes to an increased occurrence of random mutations [9][49]. It is important to note that resistance to one stressor, such as higher temperatures, can provide protection against other stressors (e.g., antibiotics) [50]. This phenomenon is known as collateral resistance or cross-protection, which was studied by Rodríguez-Verdugo et al. in 2013 [51]. Interestingly, certain generations of E. coli have acquired antibiotic resistance despite never being directly exposed to them. Instead, resistance emerged owing to exposure to elevated temperatures. Both temperature and antibiotics influence the transcription of RNA polymerase, leading to the acquisition of mutations as a survival mechanism against heat stress, conferring also resistance to antibiotics [46][51].
Additionally, warmer environmental temperatures promote biofilm formation, mainly because of the decrease in oxygen solubility with increasing temperature. In response to these changing conditions, bacteria adapt their growth and behavior, transitioning from planktonic bacteria to biofilms. Within biofilms, bacteria enter a dormant state, enabling them to better tolerate the presence of antibiotics. Consequently, biofilms exhibit increased resistance to antibiotics. In the context of reduced oxygen availability, certain bacterial species can adapt their metabolism and form biofilms to enhance their survival and persistence. Biofilms provide protection and access to nutrients, allowing bacteria to thrive in oxygen-depleted environments [50]. In summary, microorganisms have the ability to adapt and persist by undergoing genetic mutations and selecting strains that are better suited to their environment. This includes developing resistance to antibiotics as a means of survival in the presence of these drugs [46].
References
- Cavicchioli, R.; Ripple, W.J.; Timmis, K.N.; Azam, F.; Bakken, L.R.; Baylis, M.; Behrenfeld, M.J.; Boetius, A.; Boyd, P.W.; Classen, A.T.; et al. Scientists’ warning to humanity: Microorganisms and climate change. Nat. Rev. Microbiol. 2019, 17, 569–586.
- Raffel, T.R.; Romansic, J.M.; Halstead, N.T.; McMahon, T.A.; Venesky, M.D.; Rohr, J.R. Disease and thermal acclimation in a more variable and unpredictable climate. Nat. Clim. Change 2013, 3, 146–151.
- Tong, S.; Ebi, K.; Olsen, J. Infectious disease, the climate, and the future. Environ. Epidemiol. 2021, 5, e133.
- Thomas, M.B. Epidemics on the move: Climate change and infectious disease. PLoS Biol. 2020, 18, e3001013.
- Duchenne-Moutien, R.A.; Neetoo, H. Climate Change and Emerging Food Safety Issues: A Review. J. Food Prot. 2021, 84, 1884–1897.
- Casadevall, A.; Kontoyiannis, D.P.; Robert, V. On the Emergence of Candida auris: Climate Change, Azoles, Swamps, and Birds. mBio 2019, 10, e01397-19.
- Kurane, I. The effect of global warming on infectious diseases. Osong Public Health Res. Perspect. 2010, 1, 4–9.
- Richter, K.; Haslbeck, M.; Buchner, J. The Heat Shock Response: Life on the Verge of Death. Mol. Cell 2010, 40, 253–266.
- Coates, S.J.; Norton, S.A. The effects of climate change on infectious diseases with cutaneous manifestations. Int. J. Women’s Dermatol. 2021, 7, 8–16.
- Bartlow, A.W.; Manore, C.; Xu, C.; Kaufeld, K.A.; Del Valle, S.; Ziemann, A.; Fairchild, G.; Fair, J.M. Forecasting Zoonotic Infectious Disease Response to Climate Change: Mosquito Vectors and a Changing Environment. Vet. Sci. 2019, 6, 40.
- Semenza, J.C.; Paz, S. Climate change and infectious disease in Europe: Impact, projection and adaptation. Lancet Reg. Health Eur. 2021, 9, 100230.
- Semenza, J.C.; Suk, J.E. Vector-borne diseases and climate change: A European perspective. FEMS Microbiol. Lett. 2018, 365, fnx244.
- Caminade, C.; McIntyre, K.M.; Jones, A.E. Impact of recent and future climate change on vector-borne diseases. Ann. N. Y. Acad. Sci. 2019, 1436, 157–173.
- The Lancet Microbe. Climate change: Fires, floods, and infectious diseases. Lancet Microbe 2021, 2, e415.
- Fouladkhah, A. Changing climate: A ‘threat multiplier’ for foodborne and waterborne infectious diseases and antibiotic resistance. Res. Outreach 2020, 114, 130–133.
- Sobel, A.H.; Tippett, M.K. Extreme Events: Trends and Risk Assessment Methodologies. In Resilience: The Science of Adaptation to Climate Change; Zommers, Z., Alverson, K., Eds.; Elsevier: Amsterdam, The Netherlands, 2018; pp. 3–12. ISBN 9780128118917.
- Stephan, J.G.; de Miranda, J.R.; Forsgren, E. American foulbrood in a honeybee colony: Spore-symptom relationship and feedbacks between disease and colony development. BMC Ecol. 2020, 20, 16.
- FAO. The State of World Fisheries and Aquaculture 2020: Sustainability in Action; FAO (Food and Agriculture Organization): Budapest, Hungary, 2020.
- Bunse, C.; Lundin, D.; Karlsson, C.M.G.; Akram, N.; Vila-Costa, M.; Palovaara, J.; Svensson, L.; Holmfeldt, K.; González, J.M.; Calvo, E.; et al. Response of marine bacterioplankton pH homeostasis gene expression to elevated CO2. Nat. Clim. Change 2016, 6, 483–487.
- Wang, Z.; Tsementzi, D.; Williams, T.C.; Juarez, D.L.; Blinebry, S.K.; Garcia, N.S.; Sienkiewicz, B.K.; Konstantinidis, K.T.; Johnson, Z.I.; Hunt, D.E. Environmental stability impacts the differential sensitivity of marine microbiomes to increases in temperature and acidity. ISME J. 2021, 15, 19–28.
- Hutchins, D.A.; Fu, F. Microorganisms and ocean global change. Nat. Microbiol. 2017, 2, 17058.
- Williams, P.C.M.; Bartlett, A.W.; Howard-Jones, A.; McMullan, B.; Khatami, A.; Britton, P.N.; Marais, B.J. Impact of climate change and biodiversity collapse on the global emergence and spread of infectious diseases. J. Paediatr. Child Health 2021, 57, 1811–1818.
- Koch, L.K.; Kochmann, J.; Klimpel, S.; Cunze, S. Modeling the climatic suitability of leishmaniasis vector species in Europe. Sci. Rep. 2017, 7, 13325.
- Ryan, S.J.; Carlson, C.J.; Mordecai, E.A.; Johnson, L.R. Global expansion and redistribution of Aedes-borne virus transmission risk with climate change. PLoS Negl. Trop. Dis. 2019, 13, e0007213.
- Ashford, R.W. The leishmaniases as emerging and reemerging zoonoses. Int. J. Parasitol. 2000, 30, 1269–1281.
- Hotez, P.J.; Bottazzi, M.E.; Franco-Paredes, C.; Ault, S.K.; Periago, M.R. The Neglected Tropical Diseases of Latin America and the Caribbean: A Review of Disease Burden and Distribution and a Roadmap for Control and Elimination. PLoS Negl. Trop. Dis. 2008, 2, e300.
- Alvar, J.; Vélez, I.D.; Bern, C.; Herrero, M.; Desjeux, P.; Cano, J.; Jannin, J.; Boer, M. den Leishmaniasis Worldwide and Global Estimates of Its Incidence. PLoS ONE 2012, 7, e35671.
- Impactos del Cambio Climático en la Salud; Ministerio De Sanidad Igualdad y Servicios: Madrid, Spain, 2013.
- Pozio, E. How globalization and climate change could affect foodborne parasites. Exp. Parasitol. 2020, 208, 107807.
- Kuhn, K.G.; Nygård, K.M.; Guzman-Herrador, B.; Sunde, L.S.; Rimhanen-Finne, R.; Trönnberg, L.; Jepsen, M.R.; Ruuhela, R.; Wong, W.K.; Ethelberg, S. Campylobacter infections expected to increase due to climate change in Northern Europe. Sci. Rep. 2020, 10, 13874.
- Semenza, J.C.; Herbst, S.; Rechenburg, A.; Suk, J.E.; Höser, C.; Schreiber, C.; Kistemann, T. Climate Change Impact Assessment of Food and Waterborne Diseases. Crit. Rev. Environ. Sci. Technol. 2012, 42, 857–890.
- Morgado, M.E.; Jiang, C.; Zambrana, J.; Upperman, C.R.; Mitchell, C.; Boyle, M.; Sapkota, A.R.; Sapkota, A. Climate change, extreme events, and increased risk of salmonellosis: Foodborne diseases active surveillance network (FoodNet), 2004–2014. Environ. Health 2021, 20, 105.
- Li, X.; Yang, B.; Shi, C.; Wang, H.; Yu, R.; Li, Q.; Liu, S. Synergistic Interaction of Low Salinity Stress With Vibrio Infection Causes Mass Mortalities in the Oyster by Inducing Host Microflora Imbalance and Immune Dysregulation. Front. Immunol. 2022, 13, 859975.
- Semenza, J.C. Cascading risks of waterborne diseases from climate change. Nat. Immunol. 2020, 21, 484–487.
- Chala, B.; Hamde, F. Emerging and Re-emerging Vector-Borne Infectious Diseases and the Challenges for Control: A Review. Front. Public Health 2021, 9, 715759.
- Costa, F.; Hagan, J.E.; Calcagno, J.; Kane, M.; Torgerson, P.; Martinez-Silveira, M.S.; Stein, C.; Abela-Ridder, B.; Ko, A.I. Global Morbidity and Mortality of Leptospirosis: A Systematic Review. PLoS Negl. Trop. Dis. 2015, 9, e0003898.
- Trærup, S.L.M.; Ortiz, R.A.; Markandya, A. The costs of climate change: A study of cholera in Tanzania. Int. J. Environ. Res. Public Health 2011, 8, 4386–4405.
- Riebesell, U.; Aberle-Malzahn, N.; Achterberg, E.P.; Algueró-Muñiz, M.; Alvarez-Fernandez, S.; Arístegui, J.; Bach, L.T.; Boersma, M.; Boxhammer, T.; Guan, W.; et al. Toxic algal bloom induced by ocean acidification disrupts the pelagic food web. Nat. Clim. Change 2018, 8, 1082–1086.
- Barreiro, C.; Barredo, J.L. Worldwide Clinical Demand for Antibiotics: Is It a Real Countdown? Methods Mol. Biol. 2021, 2296, 3–15.
- O’Neill, J. Antimicrobial Resistance: Tackling a Crisis for the Health and Wealth of nations. Rev. Antimicrob. Resist. 2014, 1–18.
- IACG. No Time to Wait: Securing the Future from Drug-Resistant Infections; WHO (World Health Organization): New York, NY, USA, 2019.
- McGough, S.F.; MacFadden, D.R.; Hattab, M.W.; Mølbak, K.; Santillana, M. Rates of increase of antibiotic resistance and ambient temperature in Europe: A cross-national analysis of 28 countries between 2000 and 2016. Eurosurveillance 2020, 25, 1900414.
- Barreiro, C.; Gutiérrez, S.; Olivera, E.R. Fungal Horizontal Gene Transfer: A History Beyond the Phylogenetic Kingdoms. In Horizontal Gene Transfer; Villa, T., Viñas, M., Eds.; Springer: Berlin/Heidelberg, Germany, 2019; pp. 315–336. ISBN 978-3-030-21861-4.
- Souli, M.; Galani, I.; Giamarellou, H. Emergence of extensively drug-resistant and pandrug-resistant Gram-negative bacilli in Europe. Eurosurveillance 2008, 13, 19045.
- Gifford, D.R.; Moss, E.; MacLean, R.C. Environmental variation alters the fitness effects of rifampicin resistance mutations in Pseudomonas aeruginosa. Evolution 2016, 70, 725–730.
- Rodríguez-Verdugo, A.; Lozano-Huntelman, N.; Cruz-Loya, M.; Savage, V.; Yeh, P. Compounding Effects of Climate Warming and Antibiotic Resistance. iScience 2020, 23, 101024.
- MacFadden, D.R.; McGough, S.F.; Fisman, D.; Santillana, M.; Brownstein, J.S. Antibiotic Resistance Increases with Local Temperature. Nat. Clim. Change 2018, 8, 510–514.
- Burnham, J.P. Climate change and antibiotic resistance: A deadly combination. Ther. Adv. Infect. Dis. 2021, 8, 2049936121991374.
- Waits, A.; Emelyanova, A.; Oksanen, A.; Abass, K.; Rautio, A. Human infectious diseases and the changing climate in the Arctic. Environ. Int. 2018, 121, 703–713.
- Andersson, D.I.; Hughes, D. Antibiotic resistance and its cost: Is it possible to reverse resistance? Nat. Rev. Microbiol. 2010, 8, 260–271.
- Rodríguez-Verdugo, A.; Gaut, B.S.; Tenaillon, O. Evolution of Escherichia coli rifampicin resistance in an antibiotic-free environment during thermal stress. BMC Evol. Biol. 2013, 13, 50.
More
Information
Subjects:
Microbiology
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
626
Revisions:
2 times
(View History)
Update Date:
10 Aug 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




