You're using an outdated browser. Please upgrade to a modern browser for the best experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Md. Al-Amin | -- | 1130 | 2023-03-21 03:27:49 | | | |
| 2 | Conner Chen | Meta information modification | 1130 | 2023-03-22 02:53:12 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Al-Amin, M.; Hossain, M.T.; Tahir, M.; Wyman, D.; Kabir, S.M.F. Mechanisms of Face Coverings. Encyclopedia. Available online: https://encyclopedia.pub/entry/42370 (accessed on 23 December 2025).
Al-Amin M, Hossain MT, Tahir M, Wyman D, Kabir SMF. Mechanisms of Face Coverings. Encyclopedia. Available at: https://encyclopedia.pub/entry/42370. Accessed December 23, 2025.
Al-Amin, Md., Md Tanjim Hossain, Muneeb Tahir, Diana Wyman, S M Fijul Kabir. "Mechanisms of Face Coverings" Encyclopedia, https://encyclopedia.pub/entry/42370 (accessed December 23, 2025).
Al-Amin, M., Hossain, M.T., Tahir, M., Wyman, D., & Kabir, S.M.F. (2023, March 21). Mechanisms of Face Coverings. In Encyclopedia. https://encyclopedia.pub/entry/42370
Al-Amin, Md., et al. "Mechanisms of Face Coverings." Encyclopedia. Web. 21 March, 2023.
Copy Citation
The filtration function provided by fabric face coverings is not necessarily based upon sieving out larger particles that attempt to pass through to the other side of the fibrous assembly, rather, it is delineated by aerodynamic, electrostatic, and molecular interactions. Therefore, textile-based face coverings use various means to offer protection against the virions riding atop respiratory droplets from reaching the respiratory tract.
COVID-19
face coverings
masks
reusable masks
1. Introduction
COVID-19 is part of a family of viruses known as coronaviruses. This contagious disease is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [1]. SARS-CoV-2 is a rapidly mutating virus, and the scientific community continues to learn more about various mutated strains of this pathogen over time. There is, however, a mature understanding among epidemiologists that the SARS-CoV-2 pathogen relies primarily on respiratory droplets of various sizes, including aerosols, for its transmission. There is a great deal of discussion but no clear scientific consensus on what size of an infectious respiratory droplet classifies as an aerosol. In this context, the World Health Organization (WHO) has proposed a basic definition to address the ambiguity. According to WHO, droplets of greater than 5-micron diameter classify as respiratory aerosols [2]. Studies have focused on observing the particle size distribution in aerosolization due to various activities including human speech, singing, coughing, sneezing, shouting, exhaling, etc. have produced inconsistent results [3][4][5][6]. This variation could be explained by different test methodologies and prevalent ambient conditions for these studies. Particle size distribution has a high degree of variability due to the interplay of factors such as the nature of the transmitted fluid under consideration, relative humidity, the temperature at which the testing is performed, age, health status, and gender of the test subject [2]. Airborne transmission of the pathogen beyond six feet is rare and depends on special circumstances [7]. Large-sized droplets can be blocked by filtration barriers with relative ease; however, more sophisticated processes and defensive mechanisms are required for protection from the contagion-loaded aerosol. In real-life conditions, a diverse set of variables dictate the particle size distribution in droplets that are generated from any form of expiratory exertion [8]. These variables, therefore, influence the chances of transmission among people. Against the backdrop of these variables, it is not realistic to completely eliminate the chances of pathogenic transfer and infection through respiration by adopting the habit of wearing a face covering. However, the use of face coverings is still presented as one of the most significant risk-mitigation strategies considering emergent epidemiological evidence [9]. In response to the SARS-CoV-2 pandemic, the use of fabric face coverings by the public is recommended by various governments and intergovernmental agencies to reduce transmission of the virus. The US Center for Disease Control and Prevention (CDC) issued a public advisory to wear face coverings in public gatherings, where social distancing was difficult to observe during the initial days of the COVID-19 pandemic. As this global health crisis has evolved, a voluminous body of independent research has continued to emerge that links the prevalence of face-covering use with reduced infection rates [10][11][12]. Therefore, it has become vital for global efforts to mitigate the health challenges posed by airborne or aerosol-based contagious pathogens such as SARS-CoV-2 and understand the protection mechanism of face coverings. [13][14][15]
There are three main types of face coverings available to reduce the spread or contraction of COVID-19. These types are fabric face coverings (woven, knitted, woven nonwoven/knitted nonwoven hybrids), surgical masks, and professional-grade medical respirators (N95). With limited supplies of personal protection equipment (N95s and surgical masks) for frontline medical workers amid a severe supply-side shock, CDC advised to use available household woven or knitted fabrics to make face coverings [16].
Our globalized world is currently reeling from multiple concurrent crises including the COVID-19 pandemic and the Russia–Ukraine conflict. These crises have spiraled fuel prices upwards and made international shipping cost prohibitive in many cases. Likewise, the global textile supply chain has been battered hard by simultaneous demand and supply shocks [17]. These uncertain times provide an opportunity to think about how future global health crises can be better managed via the utilization of alternative strategies such as the employment of reusable face coverings to combat scarcity [18]. There is a considerable gap in the research literature that informs scholastic understanding of the interactions between textile fibers and the viral load carrying droplets at the micro-level. Much of the existing scholarship about textile-based protection from pathogenic agents revolves around fabric construction parameters, fit, and types of apparel-sourced face-covering materials. To be viable and comfortable, face coverings need to be sufficiently breathable in addition to being efficient at blocking particles. Knitted face coverings can be good alternatives to disposable medical masks in critical coronavirus outbreak situations when communities are facing shortages of more “specialized,” single-use face coverings. Knitted face covers are cost-effective, environmentally friendly, and reusable. However, the research found that knitted fabrics show lower droplet-blocking efficiency compared to woven fabrics even when both fabrics have the same porosity [19].
2. Mechanisms of Face Coverings
The filtration function provided by fabric face coverings is not necessarily based upon sieving out larger particles that attempt to pass through to the other side of the fibrous assembly, rather, it is delineated by aerodynamic, electrostatic, and molecular interactions [20]. Therefore, textile-based face coverings use various means to offer protection against the virions riding atop respiratory droplets from reaching the respiratory tract. Woven or knitted fabric face coverings employ the same filtration mechanisms as N95 and surgical masks that might not be accessible to many economically vulnerable population segments around the world [21], albeit at a lower efficiency [22]. At least four papers reviewed include useful explanations of filtration mechanisms and how textile face-covering materials utilize these mechanisms [13][23][24][25]. No conflict was found among these explanations, and they provide context for data from other papers as well.
2.1. Interception and Impaction
Air curves around the fibers or yarns in textile structures; droplets are unable to follow the air’s trajectory and collide with the textile fibers instead (Figure 1). Interception and impaction mechanisms are relevant to fabric face coverings because viruses typically travel on droplets that are large enough to be stopped by contact with textile fibers. Droplet sizes of 0.1–1 micron are stopped by interception. Droplets larger than 1 micron experience impaction [13][24][25].
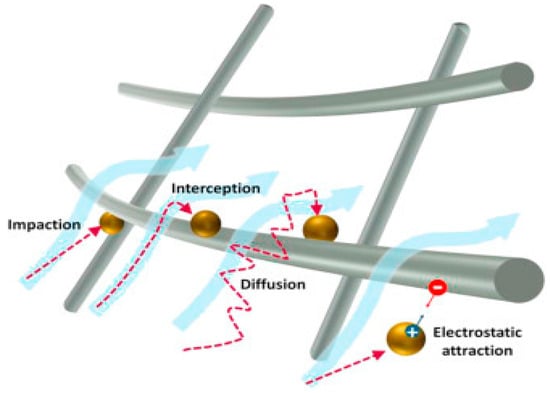
Figure 1. Filtration mechanism of face coverings [26].
2.2. Diffusion
At the submicron scale, pathogenic particles collide with the air molecules in a process called diffusion. Collisions with gaseous molecules cause these particles to slam into the fibers instead of following normal trajectories through the inter-fiber or inter-yarn voids (Figure 1) [24][25]. Filtration by diffusion requires very fine microfibers to trap very small particles. This mechanism is less commonly employed by woven and knitted face-covering fabrics [13].
2.3. Electrostatic Attraction
References
- Krammer, F. SARS-CoV-2 vaccines in development. Nature 2020, 586, 516–527.
- World Health Organization. Infection Prevention and Control of Epidemic-and Pandemic-Prone Acute Respiratory Infections in Health Care; World Health Organization: Geneva, Switzerland, 2014.
- Lindsley, W.G.; Pearce, T.A.; Hudnall, J.B.; Davis, K.A.; Davis, S.M.; Fisher, M.A.; Khakoo, R.; Palmer, J.E.; Clark, K.E.; Celik, I.; et al. Quantity and Size Distribution of Cough-Generated Aerosol Particles Produced by Influenza Patients During and after Illness. J. Occup. Environ. Hyg. 2012, 9, 443–449.
- Asadi, S.; Wexler, A.S.; Cappa, C.D.; Barreda, S.; Bouvier, N.M.; Ristenpart, W.D. Aerosol emission and superemission during human speech increase with voice loudness. Sci. Rep. 2019, 9, 2348.
- Alsved, M.; Matamis, A.; Bohlin, R.; Richter, M.; Bengtsson, P.-E.; Fraenkel, C.-J.; Medstrand, P.; Löndahl, J. Exhaled respiratory particles during singing and talking. Aerosol Sci. Technol. 2020, 54, 1245–1248.
- Zayas, G.; Chiang, M.C.; Wong, E.; Macdonald, F.; Lange, C.F.; Senthilselvan, A.; King, M. Cough aerosol in healthy participants: Fundamental knowledge to optimize droplet-spread infectious respiratory disease management. BMC Pulm. Med. 2012, 12, 11.
- Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19); Centers for Disease Control and Prevention: Atlanta, GA, USA, 2020.
- Sickbert-Bennett, E.E.; Samet, J.M.; Clapp, P.W.; Chen, H.; Berntsen, J.; Zeman, K.L.; Tong, H.; Weber, D.J.; Bennett, W.D. Filtration Efficiency of Hospital Face Mask Alternatives Available for Use During the COVID-19 Pandemic. JAMA Intern. Med. 2020, 180, 1607–1612.
- Howard, J.; Huang, A.; Li, Z.; Tufekci, Z.; Zdimal, V.; van der Westhuizen, H.-M.; von Delft, A.; Price, A.; Fridman, L.; Tang, L.-H.; et al. An evidence review of face masks against COVID-19. Proc. Natl. Acad. Sci. USA 2021, 118, e2014564118.
- Gallaway, M.S.; Rigler, J.; Robinson, S.; Herrick, K.; Livar, E.; Komatsu, K.K.; Brady, S.; Cunico, J.; Christ, C.M. Trends in COVID-19 incidence after implementation of mitigation measures—Arizona, January 22–August 7, 2020. Morb. Mortal. Wkly. Rep. 2020, 69, 1460.
- Van Dyke, M.E.; Rogers, T.M.; Pevzner, E.; Satterwhite, C.L.; Shah, H.B.; Beckman, W.J.; Ahmed, F.; Hunt, C.; Rule, J. Trends in county-level COVID-19 incidence in counties with and without a mask mandate—Kansas, June 1–August 23, 2020. Morb. Mortal. Wkly. Rep. 2020, 69, 1777.
- Mitze, T.; Kosfeld, R.; Rode, J.; Wälde, K. Face masks considerably reduce COVID-19 cases in Germany. Proc. Natl. Acad. Sci. USA 2020, 117, 32293–32301.
- Bhattacharjee, S.; Bahl, P.; Chughtai, A.A.; MacIntyre, C.R. Last-resort strategies during mask shortages: Optimal design features of cloth masks and decontamination of disposable masks during the COVID-19 pandemic. BMJ Open Respir. Res. 2020, 7, e000698.
- Clase, C.M.; Fu, E.L.; Ashur, A.; Beale, R.C.; Clase, I.A.; Dolovich, M.B.; Jardine, M.J.; Joseph, M.; Kansiime, G.; Mann, J.F.; et al. Forgotten Technology in the COVID-19 Pandemic: Filtration Properties of Cloth and Cloth Masks—A Narrative Review. Mayo Clin. Proc. 2020, 95, 2204–2224.
- Nanda, A.; Hung, I.; Kwong, A.; Man VC, M.; Roy, P.; Davies, L.; Douek, M. Efficacy of surgical masks or cloth masks in the prevention of viral transmission: Systematic review, meta-analysis, and proposal for future trial. J. Evid. Based Med. 2021, 14, 97–111.
- Mahase, E. COVID-19: What is the evidence for cloth masks? BMJ 2020, 369, m14222020.
- Milewska, B. The Impact of Instability in the Business Environment on the Competitiveness of Enterprises Using the Example of the Apparel Industry. Sustainability 2022, 14, 14673.
- Shruti, V.; Pérez-Guevara, F.; Elizalde-Martínez, I.; Kutralam-Muniasamy, G. Reusable masks for COVID-19: A missing piece of the microplastic problem during the global health crisis. Mar. Pollut. Bull. 2020, 161, 111777.
- Aydin, O.; Emon, B.; Cheng, S.; Hong, L.; Chamorro, L.P.; Saif, M.T.A. Performance of fabrics for home-made masks against the spread of COVID-19 through droplets: A quantitative mechanistic study. Extreme Mech. Lett. 2020, 40, 100924.
- Luisetto, M.; Nili, B.; Khaled, E.; Mashori, G.; Rafa, A.Y.; Latishev, O.Y. Bioaerosols and Corona Virus Diffusion, Transmission, Carriers, Viral Size, Surfaces Properties and other Factor Involved. Int. J. Med. Healthc. Reports 2021, 1, 1004.
- Tucho, G.T.; Kumsa, D.M. Universal Use of Face Masks and Related Challenges During COVID-19 in Developing Countries. Risk Manag. Healthc. Policy 2021, 14, 511–517.
- O’Kelly, E.; Pirog, S.; Ward, J.; Clarkson, P.J. Ability of fabric face mask materials to filter ultrafine particles at coughing velocity. BMJ Open 2020, 10, e039424.
- Hao, W.; Parasch, A.; Williams, S.; Li, J.; Ma, H.; Burken, J.; Wang, Y. Filtration performances of non-medical materials as candidates for manufacturing facemasks and respirators. Int. J. Hyg. Environ. Health 2020, 229, 113582.
- Gandhi, M.; Marr, L.C. Uniting Infectious Disease and Physical Science Principles on the Importance of Face Masks for COVID-19. Med 2020, 2, 29–32.
- Zhang, Z.; Ji, D.; He, H.; Ramakrishna, S. Electrospun ultrafine fibers for advanced face masks. Mater. Sci. Eng. R Rep. 2020, 143, 100594.
- Han, S.; Kim, J.; Ko, S. Advances in air filtration technologies: Structure-based and interaction-based approaches. Mater. Today Adv. 2021, 9, 100134.
More
Information
Subjects:
Others
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.1K
Revisions:
2 times
(View History)
Update Date:
22 Mar 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




