
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Jan Alexander | -- | 1982 | 2023-03-20 20:42:56 | | | |
| 2 | Lindsay Dong | Meta information modification | 1982 | 2023-03-21 01:45:49 | | |
Video Upload Options
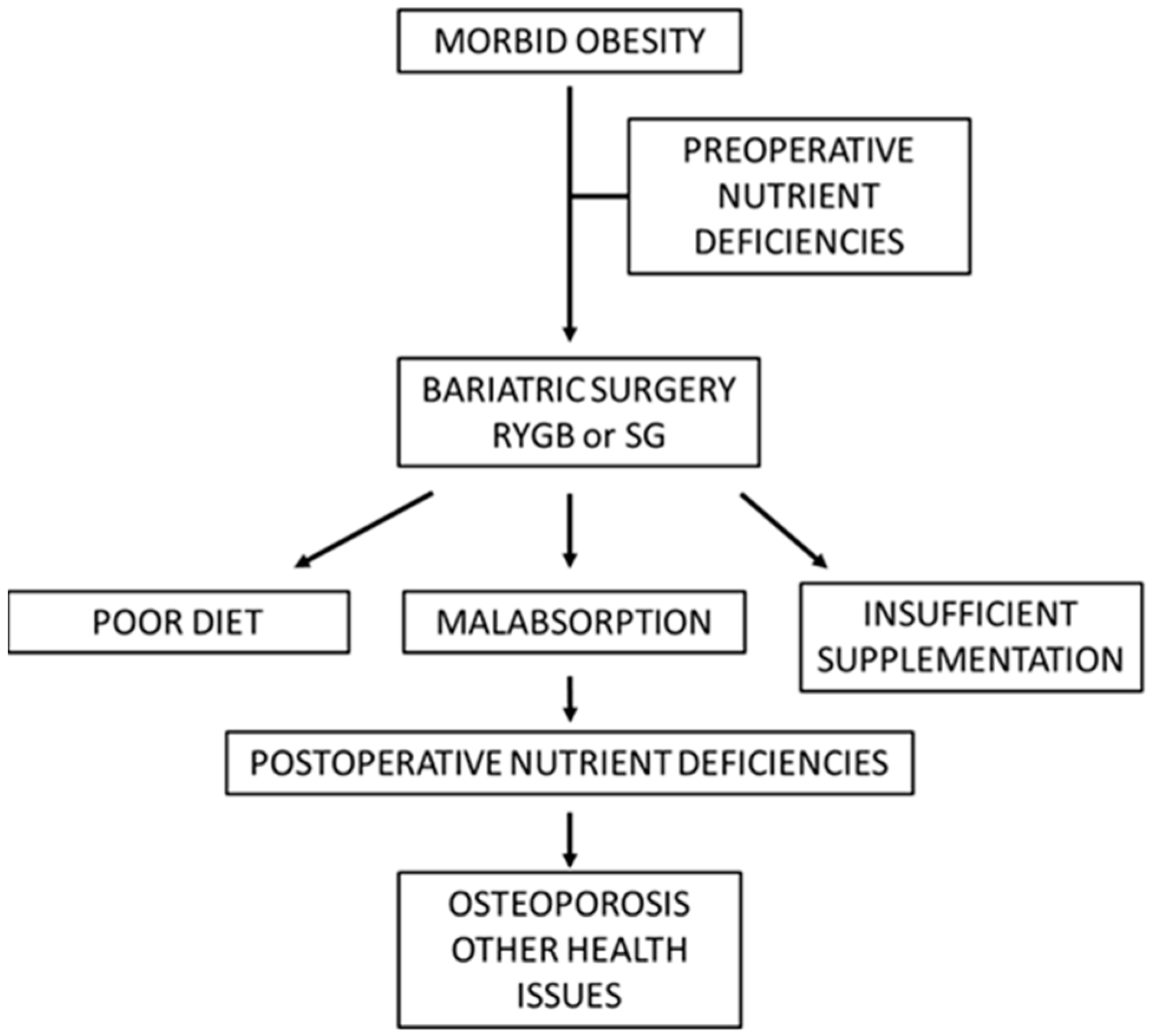
Obesity has become a worldwide epidemic accompanied by adverse health effects. The limited efficiency of traditional weight reduction regimens has led to a substantial increase in the use of bariatric surgery. Sleeve gastrectomy (SG) and Roux-en-Y-gastric bypass (RYGB) are the most used procedures. Preoperatively, the dietary habits of obese individuals might lead to deficiencies in vitamin D and other nutrients affecting bone mineral metabolism. Bariatric surgery with SG or RYGB can aggravate these deficiencies. The various surgical procedures appear to affect nutrient absorption differently. Being purely restrictive, SG may particularly affect the absorption of vitamin B12 and also vitamin D. In contrast, RYGB has a more profound impact on the absorption of fat-soluble vitamins and other nutrients, although both surgical methods induce only a mild protein deficiency. Despite adequate supplementation of calcium and vitamin D, osteoporosis may still occur after the surgery. This might be due to deficiencies in other micronutrients, e.g., vitamin K and zinc. Regular follow-ups with individual assessments and nutritional advice are indispensable to prevent osteoporosis and other adverse postoperative issues.
1. Introduction
2. Pathogenic Aspects of Bone Loss and Nutrient Deficiencies
2.1. Nutrient Deficiencies in Morbid Obesity before Bariatric Surgery
2.2. Postoperative Vitamin Deficiencies Which Can Lead to Bone Loss
2.3. Postoperative Mineral and Trace Element Deficiencies Which Can Accelerate Bone Loss
3. Postoperative Osteopenia and Osteoporosis
References
- Bluher, M. Obesity: Global epidemiology and pathogenesis. Nat. Rev. Endocrinol. 2019, 15, 288–298.
- Casimiro, I.; Sam, S.; Brady, M.J. Endocrine implications of bariatric surgery: A review on the intersection between incretins, bone, and sex hormones. Physiol. Rep. 2019, 7, e14111.
- Angrisani, L.; Santonicola, A.; Iovino, P.; Vitiello, A.; Higa, K.; Himpens, J.; Scopinaro, N.I.F.S.O. IFSO worldwide survey 2016: Primary, endoluminal, and revisional procedures. Obes. Surg. 2018, 28, 3783–3794.
- Dixon, J.B.; Zimmet, P.; Alberti, K.G.; Rubino, F. Bariatric surgery: An IDF statement for obese type 2 diabetes. Diabetes Med. 2011, 28, 628–642.
- Buchwald, H.; Oien, D.M. Metabolic/bariatric surgery worldwide 2008. Obes. Surg. 2009, 19, 1605–1611.
- Saad, R.K.; Ghezzawi, M.; Habli, D.; Alami, R.S.; Chakhtoura, M. Fracture risk following bariatric surgery: A systematic review and meta-analysis. Osteoporos. Int. 2022, 33, 511–526.
- Krzizek, E.C.; Brix, J.M.; Herz, C.T.; Kopp, H.P.; Schernthaner, G.H.; Schernthaner, G.; Ludvik, B. Prevalence of micronutrient deficiency in patients with morbid obesity before bariatric surgery. Obes. Surg. 2018, 28, 643–648.
- Hewitt, S.; Aasheim, E.T.; Søvik, T.T.; Jahnsen, J.; Kristinsson, J.; Eriksen, E.F.; Mala, T. Relationships of serum 25-hydroxyvitamin D, ionized calcium and parathyroid hormone after obesity surgery. Clin. Endocrinol. 2018, 88, 372–379.
- Paccou, J.; Caiazzo, R.; Lespessailles, E.; Cortet, B. Bariatric surgery and osteoporosis. Calcif. Tissue Int. 2022, 110, 576–591.
- Bernert, C.P.; Ciangura, C.; Coupaye, M.; Czernichow, S.; Bouillot, J.L.; Basdevant, A. Nutritional deficiency after gastric bypass: Diagnosis, prevention and treatment. Diabetes Metab. 2007, 33, 13–24.
- WHO Scientific Group on Prevention; Management of Osteoporosis; World Health Organization. Prevention and Management of Osteoporosis: Report of a WHO Scientific Group; No. 921; World Health Organization: Geneva, Switzerland, 2003.
- Karaguzel, G.; Holick, M.F. Diagnosis and treatment of osteopenia. Rev. Endocr. Metab. Disord. 2010, 11, 237–251.
- Franco, C.B. Osteoporosis in gastrointestinal diseases. Transl. Gastrointest. Cancer 2014, 4, 57–68.
- Xanthakos, S.A. Nutritional deficiencies in obesity and after bariatric surgery. Pediatr. Clin. 2009, 56, 1105–1121.
- Pereira-Santos, M.; Costa, P.D.F.; Assis, A.D.; Santos, C.D.S.; Santos, D.D. Obesity and vitamin D deficiency: A systematic review and meta-analysis. Obes. Rev. 2015, 16, 341–349.
- Ghergherechi, R.; Hazhir, N.; Tabrizi, A. Comparison of vitamin D deficiency and secondary hyperparathyroidism in obese and non-obese children and adolescents. Pak. J. Biol. Sci. PJBS 2012, 15, 147–151.
- Gillis, L.; Gillis, A. Nutrient inadequacy in obese and non-obese youth. Can. J. Diet. Pract. Res. 2005, 66, 237–242.
- Dennis, E.A.; Flack, K.D.; Davy, B.M. Beverage consumption and adult weight management: A review. Eat. Behav. 2009, 10, 237–246.
- Schweiger, C.; Weiss, R.; Berry, E.; Keidar, A. Nutritional deficiencies in bariatric surgery candidates. Obes. Surg. 2010, 20, 193–197.
- Mikalsen, S.M.; Aaseth, J.; Flaten, T.P.; Whist, J.E.; Bjørke-Monsen, A.L. Essential trace elements in Norwegian obese patients before and 12 months after Roux-en-Y gastric bypass surgery: Copper, manganese, selenium and zinc. J. Trace Elem. Med. Biol. 2020, 62, 126650.
- Bloomberg, R.D.; Fleishman, A.; Nalle, J.E.; Herron, D.M.; Kini, S. Nutritional deficiencies following bariatric surgery: What have we learned? Obes. Surg. 2005, 15, 145–154.
- Blom-Høgestøl, I.K.; Hewitt, S.; Chahal-Kummen, M.; Brunborg, C.; Gulseth, H.L.; Kristinsson, J.A.; Mala, T. Bone metabolism, bone mineral density and low-energy fractures 10 years after Roux-en-Y gastric bypass. Bone 2019, 127, 436–445.
- Chakhtoura, M.T.; Nakhoul, N.N.; Shawwa, K.; Mantzoros, C.; Fuleihan, G.A.E.H. Hypovitaminosis D in bariatric surgery: A systematic review of observational studies. Metabolism 2016, 65, 574–585.
- Hewitt, S.; Søvik, T.T.; Aasheim, E.T.; Kristinsson, J.; Jahnsen, J.; Birketvedt, G.S.; Mala, T. Secondary hyperparathyroidism, vitamin D sufficiency, and serum calcium 5 years after gastric bypass and duodenal switch. Obes. Surg. 2013, 23, 384–390.
- Lespessailles, E.; Toumi, H. Vitamin D alteration associated with obesity and bariatric surgery. Exp. Biol. Med. 2017, 242, 1086–1094.
- Lupoli, R.; Lembo, E.; Saldalamacchia, G.; Avola, C.K.; Angrisani, L.; Capaldo, B. Bariatric surgery and long-term nutritional issues. World J. Diabetes 2017, 8, 464.
- Lewis, C.A.; de Jersey, S.; Seymour, M.; Hopkins, G.; Hickman, I.; Osland, E. Iron, vitamin B12, folate and copper deficiency after bariatric surgery and the impact on anaemia: A systematic review. Obes. Surg. 2020, 30, 4542–4591.
- Macêdo, L.L.G.D.; Carvalho, C.M.R.G.D.; Cavalcanti, J.C. Vitamin B12, bone mineral density and fracture risk in adults: A systematic review. Rev. Da Assoc. Médica Bras. 2017, 63, 801–809.
- Patel, R.; Saumoy, M. Treatment of Micronutrient Deficiencies Pre and Post Bariatric Surgery. Curr. Treat. Options Gastroenterol. 2021, 19, 169–182.
- Al-Jafar, H.; Al-Zamil, K.; Al Ageeli, M.; Alhaifi, M.; Al-Sabah, S. Potential hematology and nutritional complications of bariatric surgery. Ann. Hematol. Oncol. 2018, 5, 1209.
- Antoniewicz, A.; Kalinowski, P.; Kotulecka, K.J.; Kocoń, P.; Paluszkiewicz, R.; Remiszewski, P.; Zieniewicz, K. Nutritional deficiencies in patients after Roux-en-Y gastric bypass and sleeve gastrectomy during 12-month follow-up. Obes. Surg. 2019, 29, 3277–3284.
- Herrmann, M.; Peter Schmidt, J.; Umanskaya, N.; Wagner, A.; Taban-Shomal, O.; Widmann, T.; Herrmann, W. The role of hyperhomocysteinemia as well as folate, vitamin B6 and B12 deficiencies in osteoporosis–a systematic review. Clin. Chem. Lab. Med. 2007, 45, 1621–1632.
- Aaseth, J.; Boivin, G.; Andersen, O. Osteoporosis and trace elements—An overview. J. Trace Elem. Med. Biol. 2012, 26, 149–152.
- Castiglioni, S.; Cazzaniga, A.; Albisetti, W.; Maier, J.A. Magnesium and osteoporosis: Current state of knowledge and future research directions. Nutrients 2013, 5, 3022–3033.
- Galchenko, A.; Gapparova, K.; Sidorova, E. The influence of vegetarian and vegan diets on the state of bone mineral density in humans. Crit. Rev. Food Sci. Nutr. 2021, 63, 845–861.
- Bae, Y.J.; Kim, M.H. Manganese supplementation improves mineral density of the spine and femur and serum osteocalcin in rats. Biol. Trace Elem. Res. 2008, 124, 28–34.
- Tsay, J.; Yang, Z.; Ross, F.P.; Cunningham-Rundles, S.; Lin, H.; Coleman, R.; Vogiatzi, M.G. Bone loss caused by iron overload in a murine model: Importance of oxidative stress. Blood J. Am. Soc. Hematol. 2010, 116, 2582–2589.
- Søgaard, A.J.; Holvik, K.; Omsland, T.K.; Tell, G.S.; Dahl, C.; Schei, B.; Meyer, H.E. Abdominal obesity increases the risk of hip fracture. A population-based study of 43,000 women and men aged 60–79 years followed for 8 years. Cohort of N orway. J. Intern. Med. 2015, 277, 306–317.
- Turer, C.B.; Lin, H.; Flores, G. Prevalence of vitamin D deficiency among overweight and obese US children. Pediatrics 2013, 131, e152–e161.
- Vranić, L.; Mikolašević, I.; Milić, S. Vitamin D deficiency: Consequence or cause of obesity? Medicina 2019, 55, 541.
- Briganti, S.I.; Naciu, A.M.; Tabacco, G.; Cesareo, R.; Napoli, N.; Trimboli, P.; Palermo, A. Proton pump inhibitors and fractures in adults: A critical appraisal and review of the literature. Int. J. Endocrinol. 2021, 2021, 8902367.
- Finnes, T.E.; Lofthus, C.M.; Meyer, H.E.; Søgaard, A.J.; Tell, G.S.; Apalset, E.M.; Holvik, K. A combination of low serum concentrations of vitamins K1 and D is associated with increased risk of hip fractures in elderly Norwegians: A NOREPOS study. Osteoporos. Int. 2016, 27, 1645–1652.
- Saad, R.; Habli, D.; El Sabbagh, R.; Chakhtoura, M. Bone health following bariatric surgery: An update. J. Clin. Densitom. 2020, 23, 165–181.
- Hao, G.; Zhang, B.; Gu, M.; Chen, C.; Zhang, Q.; Zhang, G.; Cao, X. Vitamin K intake and the risk of fractures: A meta-analysis. Medicine 2017, 96, e6725.
- Yamaguchi, M. Role of nutritional zinc in the prevention of osteoporosis. Mol. Cell. Biochem. 2010, 338, 241–254.
- Zheng, J.; Mao, X.; Ling, J.; He, Q.; Quan, J. Low serum levels of zinc, copper, and iron as risk factors for osteoporosis: A meta-analysis. Biol. Trace Elem. Res. 2014, 160, 15–23.
- Marquardt, M.L.; Done, S.L.; Sandrock, M.; Berdon, W.E.; Feldman, K.W. Copper deficiency presenting as metabolic bone disease in extremely low birth weight, short-gut infants. Pediatrics 2012, 130, e695–e698.
- Hofsø, D.; Hillestad, T.O.W.; Halvorsen, E.; Fatima, F.; Johnson, L.K.; Lindberg, M.; Hjelmesæth, J. Bone mineral density and turnover after sleeve gastrectomy and gastric bypass: A randomized controlled trial (Oseberg). J. Clin. Endocrinol. Metab. 2021, 106, 501–511.
- Brzozowska, M.M.; Tran, T.; Bliuc, D.; Jorgensen, J.; Talbot, M.; Fenton-Lee, D.; Center, J.R. Roux-en-Y gastric bypass and gastric sleeve surgery result in long term bone loss. Int. J. Obes. 2021, 45, 235–246.
- Svanevik, M.; Risstad, H.; Hofsø, D.; Blom-Høgestøl, I.K.; Kristinsson, J.A.; Sandbu, R.; Hjelmesæth, J. Bone turnover markers after standard and distal Roux-en-Y gastric bypass: Results from a randomized controlled trial. Obes. Surg. 2019, 29, 2886–2895.
- Liu, Y.; Côté, M.M.; Cheney, M.C.; Lindeman, K.G.; Rushin, C.C.; Hutter, M.M.; Elaine, W.Y. Examining zoledronic acid for the prevention of bone loss in patients receiving bariatric surgery. Bone Rep. 2021, 14, 100760.





