Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Virendra Kumar Yadav | -- | 2580 | 2022-11-30 11:06:46 | | | |
| 2 | Rita Xu | Meta information modification | 2580 | 2022-11-30 11:20:57 | | | | |
| 3 | Rita Xu | Meta information modification | 2580 | 2022-11-30 11:21:59 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Gupta, N.; Yadav, V.K.; Gacem, A.; Al-Dossari, M.; Yadav, K.K.; El-Gawaad, N.S.A.; Khedher, N.B.; Choudhary, N.; Kumar, P.; Cavalu, S. Air Pollution on Human Microbial Community. Encyclopedia. Available online: https://encyclopedia.pub/entry/37327 (accessed on 07 February 2026).
Gupta N, Yadav VK, Gacem A, Al-Dossari M, Yadav KK, El-Gawaad NSA, et al. Air Pollution on Human Microbial Community. Encyclopedia. Available at: https://encyclopedia.pub/entry/37327. Accessed February 07, 2026.
Gupta, Nishant, Virendra Kumar Yadav, Amel Gacem, M. Al-Dossari, Krishna Kumar Yadav, N. S. Abd El-Gawaad, Nidhal Ben Khedher, Nisha Choudhary, Pankaj Kumar, Simona Cavalu. "Air Pollution on Human Microbial Community" Encyclopedia, https://encyclopedia.pub/entry/37327 (accessed February 07, 2026).
Gupta, N., Yadav, V.K., Gacem, A., Al-Dossari, M., Yadav, K.K., El-Gawaad, N.S.A., Khedher, N.B., Choudhary, N., Kumar, P., & Cavalu, S. (2022, November 30). Air Pollution on Human Microbial Community. In Encyclopedia. https://encyclopedia.pub/entry/37327
Gupta, Nishant, et al. "Air Pollution on Human Microbial Community." Encyclopedia. Web. 30 November, 2022.
Copy Citation
A balanced microbiota composition is requisite for normal physiological functions of the human body. Several environmental factors such as air pollutants may perturb the human microbiota composition. It is noticeable that currently around 99% of the world’s population is breathing polluted air. Air pollution’s debilitating health impacts have been studied scrupulously, including in the human gut microbiota.
air pollution
human microbiota
particulate matter
autoimmune diseases
1. Introduction
The human body is the home of trillions of microorganisms including viruses, bacteria, archaea, and protists [1]. Excluding parasites and viruses, a healthy individual contains more bacterial cells than his/her own cells, approximately 30 trillion human cells and 39 trillion bacterial cells (Figure 1). However, these bacterial cells are 1000 times smaller than human cells and comprise only ~2% (1.5 kg) of a healthy adult human body mass. Usually, those bacterial cell numbers may vary from person to person [2][3][4]. Figure 1 shows organ-specific bacteria in the human body.
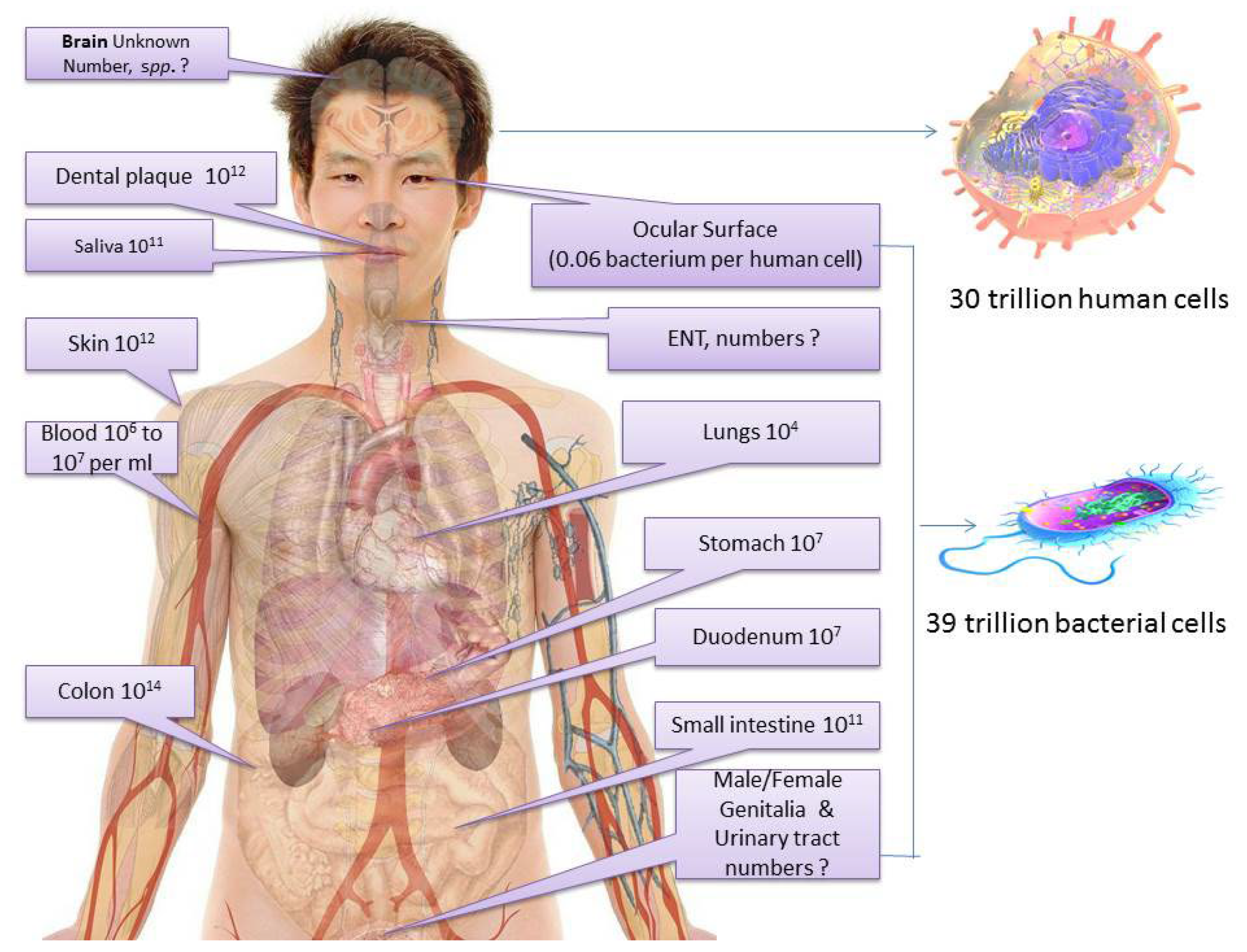
Figure 1. Organ-specific symbiotic bacterial cells in the human body.
The numbers and arrangement of bacterial species are also different in each organ. Generally, a healthy adult human colon has the highest amount of bacteria (1014), followed by the skin (1012), dental plaque (1012), lower intestine (1011), saliva (1011), stomach (107), duodenum (107) [4], the bloodstream (106 to 107 per mL), eyes (0.06 bacterium per human cell) (Gomes et al., 2020), and the respiratory system (around 104 microorganisms per mL) (Mathieu et al., 2018). Some studies even suggest bacterial cells are present in organs previously known as sterile, such as the brain and blood cells [5]. Pioneering microbiologist Louis Pasteur once stated that “life without bacteria would be unthinkable”. In fact, humans are considered superorganisms consisting of symbiotic microorganisms and cells [6]. Undoubtedly, a microorganism plays a significant role in human lives. In addition to dreadful infections, they also represent a crucial component of the human body; these commensal microbes in the body, collectively known as microbiota, are required for vital functions [7]. In particular, bacteria are a major part of the human microbiota.
These beneficial, neutral, and sometimes opportunistic microbes within the human body are known as normal microbial flora. The human body usually retains these microbes from birth. However, a few studies detected microbial cells in womb tissues as well. The normal microbiome of the human body influences physiology, anatomy, and morbidity as well as susceptibility to pathogenic germs. However, there are many factors that alter the normal microflora compositions and contribute to turning them into opportunistic pathogens [8].
Recent studies suggested air pollution’s role in symbiotic microbial dysbiosis (imbalance). Even short-term exposure to air pollutants showed strong effects against microbial interactions [9].
Air pollution may also exacerbate or facilitate pathogens’ infections such as tuberculosis, meningitis [10], and COVID-19 mortality [11][12]. Recent studies have highlighted air pollution’s role in previously less-studied gastrointestinal diseases such as increased peptic ulcer hospitalization due to PM10, O3, and NO2 air pollutants [13].
The debilitating impact of air pollution on human health is widely studied. Air pollution exposure can increase risk to maternal health and neonatal health and susceptibility to respiratory diseases, neurological disorders, cognitive ailments, cancers, and diabetes. Air pollutants enter the human body through the respiratory pathway and dissolve in the bloodstream, which may trigger inflammation, oxidative stress, immunosuppression, and mutagenicity in cells, affecting the respiratory system and other internal organs and ultimately causing diseases [14].
Undoubtedly, air pollution is a serious environmental and health concern. According to the WHO’s recent update, air pollution has affected almost all the global population; currently, 99% of people breathe air that exceeds the WHO clean air quality limits. However, the proportion and exposure of air pollution are highest among low- to middle-income nations, especially in Asian countries [15]. According to the United States Environmental Protection Agency (US EPA), common air pollutants, such as particulate pollutants (PM2.5, PM10), sulphur dioxide (SO2), carbon monoxide (CO), lead (Pb), ozone (O3), and nitrogen dioxide (NO2), are the most harmful pollutants to environmental and human health [16].
There is limited but growing evidence suggesting that exposure to environmental pollutants may lead to the dysbiosis of the human microbiota including the respiratory tract, female reproductive system, and gut. Dysbiosis of the microbiota may facilitate the overgrowth of pathogens and disrupt beneficial metabolite production, resulting in numerous health issues [17].
Most of the existing research and systematic reviews have focused on air pollution’s impact on particular types of human microbiotas such as the gut microbiota, which is considered most important for overall health. The gut microbiota was found to be extremely sensitive to drugs, diet, and even environmental pollutants [18]. However, the direct impact of air pollution on the gut seems to be underestimated [19]. Similarly, very few or negligible studies have focused on the relationship between air pollution and other microbiotas.
2. Air Pollutants and Dysbiosis of Human Microbiota
Alterations in the microbiota can be due to exposure to various environmental factors [20]. Air pollutants such as particulate matter (PM0.1, PM2.5, PM10), O3, and polycyclic aromatic hydrocarbon (PAH) inhalation may alter the human microbiota by various pathways, depending on the type of exposure. In particular, there are several courses for air pollutants and gut microbiota interactions. For instance, the gastrointestinal tract may have exposure to air pollutants via inhalation and ingestion. Usually, large particulate pollutants are deposited in the upper airway such as the trachea; but the finer pollutants, such as PM2.5, reach into the lung’s alveolar space, further moved and hidden by alveolar macrophages [21][22].
Air pollutants are associated with dysbiosis of the human microbiota, particularly the gastrointestinal microbiota. Air pollutant polycyclic aromatic hydrocarbons (PAH) may alter the commensal as well as environmental microbial communities. Air pollutant PAH can affect the purine pyrimidine metabolites’ signaling pathways and lipid metabolism [22]. An animal (broilers) study showed ammonia inhalation can also alter tracheal and ileal microbiotas by the TLR4 signaling pathway [23].
Studies showed that high concentrations of inhaled particulate matter are transported through the mucociliary pathway and that the pollutant is rapidly cleared from the lung’s alveolar cells but further transported to the intestine. Ingested particulate matter triggered gastrointestinal inflammation-induced dysbiosis of gut microbes [24]. Gut microbiota dysbiosis causes several health issues including mental health via the gut-brain axis. Gut microbes can influence the central nervous system via the vagus nerve [25][26]. Particulate matter (PM) and heavy metal air pollutants are exposed to the gut via inhalation or ingestion. PMs cause gut dysbiosis, which further disturbs or alters the composition of gut microbiota-associated regulatory metabolites such as short-chain fatty acid (SCFA), which is required for brain-gut neurotransmitter signals [27].
Short-chain fatty acid (SCFA) is the predominant anion and is usually produced by the commensal gut bacterial fermentation of undigested carbohydrates. Interestingly, up to 95% of SCFA is absorbed by colon cells (colonocytes) as an energy substrate. Colonocytes usually derive their energy (up to 70%) from SCFA’s oxidation, which provides nearly 10% of the daily calories required for the human body.
Most studies focused on gut microbiota dysbiosis, due to its role in several diseases and since the gut microbiota is associated with various ailments and may influence host cognitive function and behavior by communicating altered signals to the hypothalamus–pituitary–adrenal (HPA) axis [20]. Figure 2 shows a possible mechanism of air pollution associated with dysbiosis of gut microbiota and health issues.
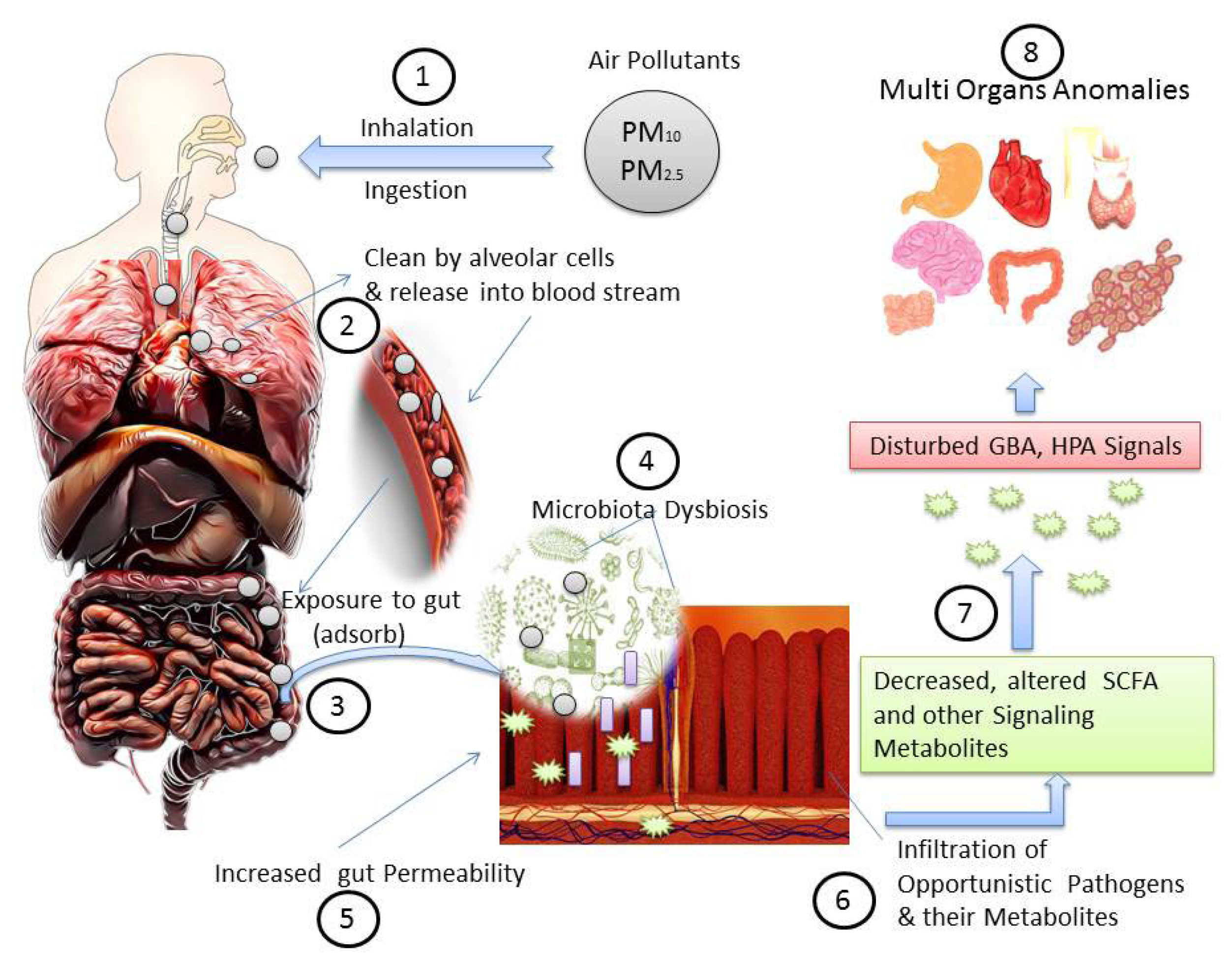
Figure 2. A possible mechanism of air pollution associated gut microbiota dysbiosis and health issues: (1) air pollutant entry; (2) respiratory system response; (3) reached to gastrointestinal tract and adsorbed; (4) dysbiosis and alteration of commensal gut microbiota; (5) altered microbial cells and their metabolites increased gut permeability and susceptibility to pathogens; (6) infiltration of harmful metabolites and pathogens decrease gut microbiota-dependent metabolites such as short-chain fatty acid (SCFA); (7) disturbed gut-brain axis (GBA) and hypothalamus–pituitary–adrenal axis (HPA); (8) altered signaling metabolites influence several organs’ functionalities.
Another proposed mechanism explains how ingested pollutants enter and are further adsorbed into the intestine from the bloodstream. These pollutants are also oxidized into the liver, form conjugates such as glutathione, and are excreted into the intestine again. The gut microbiota interferes with normal glutathione secretion; gut microbes additionally metabolize those pollutants, which disturb their composition as well, which could be responsible for the inactivation or re-activation of the specific metabolites or compounds responsible for various associated health conditions including cancer [28]. Certain commensal bacterial species such as Escherichia coli also turn invasive and cause metabolic endotoxemia, which increases the permeability of the gut wall, decreases mucus thickness, and allows pathogenic invasive bacterial species to infiltrate [29].
Studies have suggested air pollution’s negative impact on human microbiome development, which is associated with serious health outcomes including obesity, gastric ailments, and autism. Up to this time, air pollution garnered less attention despite the potential risk of negative alterations [8][30].
Several studies have explained gut microbiota dysbiosis; however, it is a multifactorially dependent, complex event to understand clearly, so far. More comprehensive research is required to understand air pollutant exposure associated with microbiota dysbiosis, especially to explain the other microbiotas’ dysbiosis of the human body.
3. Air Pollution Impact on Nasal Microbiota
The human nasal tract is the home of diverse bacterial communities. Nasal microbiota plays a pivotal role in personal and public health as well. Human nostrils are colonized by various microbes just after birth. Usually, pediatric and adult nasal microbiotas are distinguished from each other. Pediatric nasal microbiota usually belongs to the Gram-negative bacteria Haemophilus and Moraxella and Gram-positive bacteria Streptococcus, Staphylococcus, Dolosigranulum, and Corynebacterium. In the case of adults, the nasal microbiota is mostly Gram-positive (Firmicutes and Actinobacteria). Despite ample exposure to oxygen, the most frequent nasal bacterial species are either facultative anaerobes or aerotolerant. There are lesser-known factors that influence and alter nasal microbiota; age, season, and climate may also alter the nasal microbiota [31]. Additionally, air pollution, even low exposure, may influence the nasal microbiota during the first year of life; especially, exposure to air pollutants PM2.5 and NO2 is associated with nasal microbiota alteration, respiratory infections, and asthma development during early life [32][33].
Nasal microbiota is different from the upper respiratory tract (URT). The upper respiratory tract has constant airflow, which prevents the spread of pathogens to the lower respiratory tract. Usually, the nasal microbiota remains almost unchanged in adulthood. A few studies suggested that the nasal microbiota has been significantly associated with the central nervous system and immune system. Dysbiosis in the nasal microbiota may lead to inflammatory diseases and pathological invasion of the nasal cavity, which may damage the olfactory system [34].
The altered composition of beneficial bacteria residing in the nasal sinus cavity was found to be associated with Parkinson’s disease [35]. Growing evidence suggests that particulate air pollutants (PM2.5, PM10) may alter the nasal bacterial community [36][37].
4. Air Pollution and Oral Microbiota Dysbiosis
A balanced, normal composition of oral microbiota is required for the oral and probably overall health of the host. Being a compatible environment, the oral cavity facilitates the growth of many distinct commensal as well as harmful microbes. In recent years, the importance of the oral microbiome has also increased in dental medicine. The oral cavity is susceptible to constant environmental factors including host eating habits, saliva secretion, mastication, and exposure to outside microbes [38][39]. Air pollutants such as ultrafine particles (PM0.1) can affect the oral microflora and promote inflammation in the oral cavity of children [40].
In 2010, research highlighted the importance of the oral microbiome for the first time. Most recently, oral microbiota dysbiosis has emerged as one of the contributing factors to diseases such as schizophrenia and osteoporosis. Until now, probiotics were found to be useful for the restoration of oral dysbiosis [41]. Similarly, several molecules from saliva form a specific film to minimize dysbiosis; therefore, the process of dysbiosis may increase if the amount of saliva decreases [42].
Oral microbiota may influence other distant organs. Altered oral microbiota can disseminate to other organs via ingestion and systemic circulation. Recent findings indicate an association between altered oral microbiota and liver and pancreatic diseases [43], oral cancer [44], and Alzheimer’s disease [45]. A recent metagenomic analysis revealed that oropharyngeal microbiota dysbiosis was linked with COVID-19 severity [46]. In addition, oral and gut microbiotas’ crosstalk may increase the complication of oral dysbiosis to other organs [47].
5. Air Pollution Impact on Pharyngeal Microbiota
The pharyngeal microbial communities are important in the airflow cavity to stimulate the immune system and prevent unwanted pathogenesis of airborne germs. These local microbes provide a defense line against newly emerging pathogens. The most common pharyngeal microbiota belongs to bacterial genera such as Campylobacter, Capnocytophaga, Haemophilus, Neisseria, Streptococcus, Prevotella, and Veillonella. To retain proper health, a balance of common microbiota is necessary for all. However, the epithelial microbial community in the pharynx can be damaged by factors such as air pollutants, smoking, and infections [48].
It has been reported that even a few days of exposure to particulate air pollutants may alter the pharyngeal microbiota composition, which can increase the chance of respiratory infections [49]. A similar study in China concluded that air pollution can lead to oropharyngeal microbiota dysbiosis. The microbial population may differ as per the air pollutants’ concentration. For instance, in most polluted regions, bacteria belonging to Fusobacteria and Bacteroidetes were significantly lower while others, such as Proteobacteria, Firmicutes, and Actinobacteria, were found to be higher in participants [50].
A recent experiment analyzed the nature and characteristics of pharyngeal bacteria among chronic pharyngitis patients using 16S rDNA-based detection technology. The study concluded that the community and quantity of symbiotic pharyngeal bacteria decreased while the number of opportunistic bacteria increased in chronic pharyngitis patients [51]. Pharyngeal microbiota’s abundance and specificity have also been associated with age-related macular degeneration [52].
The pharynx microbiota’s potential role between gut and lung crosstalk is being investigated. A clinical study on neonates’ pharynx and intestine microbiotas showed a significant difference between intestinal and pharynx microbial species and composition. However, some species such as Streptococcus were common in both [53].
6. Air Pollution and Altered Respiratory Microbiota
The respiratory system is a complex system that facilitates oxygen and carbon dioxide exchange. Nostrils of the lungs and alveoli of the human respiratory system are inhabited by specific bacteria, which are known as the common microbiota of the respiratory tract and work as a gatekeeper to prevent the colonization of pathogens. Respiratory microbiota also maintains respiratory physiology and immunity. Despite the respiratory microbiota’s important role in mediating human health response to inhaled irritants, the respiratory microbiome and inhaled pollutants’ association have remained less explored [54].
Healthy lung microbiota usually belongs to Firmicutes and Bacteroidetes. Alteration of the respiratory microbiome is associated with inflammation and chronic lung diseases. Polluted air introduces a mixture of air pollutants such as PM2.5, PM10, O3, NO2, CO, SO2, polycyclic aromatic hydrocarbons, and pathogens into the respiratory system. The effect of polluted air is bidirectional, as air pollutants such as PM2.5 penetrate deeply into lung cells and damage epithelial integrity, which further facilitates the entrance of harmful microbes and toxic metabolites into the epithelial layer and triggers systemic immune activation, which causes alteration or dysbiosis of the lung microbiota. Air pollutants also provoke the production of reactive oxygen species (ROS), which directly kills and reduces the resident microbiota [55].
A study on 40 children showed that exposure to automobile air pollution in childhood and adolescence may be associated with significant changes in the lower respiratory microbiota, which may lead to asthma. Alteration and dysbiosis of the respiratory microbiota can increase the chance of lower and upper respiratory tract infections. In particular, lower respiratory infection such as pneumonia is responsible for considerable morbidity and mortality among children under 5 years globally [56]. A cross-sectional study on healthy adults in Malawi showed that higher exposure to particulate air pollutants caused an abundance of the potentially pathogenic bacteria Streptococcus and Neisseria in their lungs [57]. Therefore, air pollution can affect the respiratory microbiota and induce dysbiosis, which is associated with several respiratory diseases [58].
References
- Xue, Y.; Chu, J.; Li, Y.; Kong, X. The influence of air pollution on respiratory microbiome: A link to respiratory disease. Toxicol. Lett. 2020, 334, 14–20.
- Castillo, D.J.; Rifkin, R.F.; Cowan, D.A.; Potgieter, M. The healthy human blood microbiome: Fact or fiction? Front. Cell Infect. Microbiol. 2019, 9, 148.
- Patel, H.; Yadav, V.K.; Yadav, K.K.; Choudhary, N.; Kalasariya, H.; Alam, M.M.; Gacem, A.; Amanullah, M.; Ibrahium, H.A.; Park, J.-W.; et al. A Recent and Systemic Approach Towards Microbial Biodegradation of Dyes from Textile Industries. Water 2022, 14, 3163.
- Sender, R.; Fuchs, S.; Milo, R. Revised Estimates for the Number of Human and Bacteria Cells in the Body. PLoS Biol. 2016, 14, e1002533.
- Link, C.D. Is There a Brain Microbiome? Neurosci. Insights 2021, 16, 26331055211018708.
- Nardone, G.; Compare, D. The human gastric microbiota: Is it time to rethink the pathogenesis of stomach diseases? United Eur. Gastroenterol. J. 2015, 3, 255–260.
- Gomes, J.Á.P.; Frizon, L.; Demeda, V.F. Ocular surface microbiome in health and disease. Asia-Pac. J. Ophthalmol. 2020, 9, 505–511.
- Thursby, E.; Juge, N. Introduction to the human gut microbiota. Biochem. J. 2017, 474, 1823–1836.
- Karimi, B.; Meyer, C.; Gilbert, D.; Bernard, N. Air pollution below WHO levels decreases by 40% the links of terrestrial microbial networks. Environ. Chem. Lett. 2016, 14, 467–475.
- Ghio, A.J. Particle exposures and infections. Infection 2014, 42, 459–467.
- Zhu, Y.; Xie, J.; Huang, F.; Cao, L. Association between short-term exposure to air pollution and COVID-19 infection: Evidence from China. Sci. Total Environ. 2020, 727, 138704.
- Coker, E.S.; Cavalli, L.; Fabrizi, E.; Guastella, G.; Lippo, E.; Parisi, M.L.; Vergalli, S. The Effects of Air Pollution on COVID-19 Related Mortality in Northern Italy. Environ. Res. Econ. 2020, 76, 611–634.
- Tsai, S.S.; Chiu, H.F.; Yang, C.Y. Ambient air pollution and hospital admissions for peptic ulcers in Taipei: A time-stratified case-crossover study. Int. J. Environ. Res. Public Health 2019, 16, 1916.
- WHO. Air Quality and Health: Health Impact; WHO: Geneva, Switzerland, 2022.
- WHO. Air Pollution; WHO: Geneva, Switzerland, 2022.
- EPA. Criteria Air Pollutants; EPA: Washington, DC, USA, 2022.
- Mousavi, S.E.; Delgado-Saborit, J.M.; Adivi, A.; Pauwels, S.; Godderis, L. Air pollution and endocrine disruptors induce human microbiome imbalances: A systematic review of recent evidence and possible biological mechanisms. Sci. Total Environ. 2022, 816, 151654.
- Jin, Y.; Wu, S.; Zeng, Z.; Fu, Z. Effects of environmental pollutants on gut microbiota. Environ. Pollut. 2017, 222, 1–9.
- Vignal, C.; Guilloteau, E.; Gower-Rousseau, C.; Body-Malapel, M. Review article: Epidemiological and animal evidence for the role of air pollution in intestinal diseases. Sci. Total Environ. 2021, 757, 143718.
- Carding, S.; Verbeke, K.; Vipond, D.T.; Corfe, B.M.; Owen, L.J. Dysbiosis of the gut microbiota in disease. Microb. Ecol. Health Dis. 2015, 26, 26191.
- Bailey, M.J.; Naik, N.N.; Wild, L.E.; Patterson, W.B.; Alderete, T.L. Exposure to air pollutants and the gut microbiota: A potential link between exposure, obesity, and type 2 diabetes. Gut Microbes 2020, 11, 1188–1202.
- Li, J.-J.; Lu, Z.-L.; Kou, W.-R.; Chen, Z.; Wu, Y.-F.; Yu, X.-H.; Zhao, Y.C. Long-Term Effects of Xuezhikang on Blood Pressure in Hypertensive Patients with Previous Myocardial Infarction: Data from the Chinese Coronary Secondary Prevention Study (CCSPS). Clin. Exp. Hypertens. 2010, 32, 491–498.
- Zhou, Y.; Zhao, X.; Zhang, M.; Feng, J. Gut microbiota dysbiosis exaggerates ammonia-induced tracheal injury Via TLR4 signaling pathway. Ecotoxicol. Environ. Saf. 2022, 246, 114206.
- Salim, S.Y.; Kaplan, G.G.; Madsen, K.L. Air pollution effects on the gut microbiota. Gut Microbes 2014, 5, 215–219.
- Forsythe, P.; Bienenstock, J.; Kunze, W.A. Vagal Pathways for Microbiome-Brain-Gut Axis Communication. In Microbial Endocrinology: The Microbiota-Gut-Brain Axis in Health and Disease; Lyte, M., Cryan, J.F., Eds.; Springer: New York, NY, USA, 2014; pp. 115–133.
- Rahman, M.M.; Islam, F.; Or-Rashid, M.H.; Al Mamun, A.; Rahaman, M.S.; Islam, M.M.; Cavalu, S. The Gut Microbiota (Microbiome) in Cardiovascular Disease and Its Therapeutic Regulation. Front. Cell Infect. Microbiol. 2022, 12, 903570.
- Singh, S.; Sharma, P.; Pal, N.; Kumawat, M.; Shubham, S.; Sarma, D.K.; Nagpal, R. Impact of Environmental Pollutants on Gut Microbiome and Mental Health via the Gut–Brain Axis. Microorganisms 2022, 10, 1457.
- Giambò, F.; Costa, C.; Teodoro, M.; Fenga, C. Role-Playing Between Environmental Pollutants and Human Gut Microbiota: A Complex Bidirectional Interaction. Front. Med. 2022, 9, 810397.
- Weiss, G.A.; Hennet, T. Mechanisms and consequences of intestinal dysbiosis. Cell. Mol. Life Sci. 2017, 74, 2959–2977.
- Vallès, Y.; Francino, M.P. Air Pollution, Early Life Microbiome, and Development. Curr. Environ. Health Rep. 2018, 5, 512–521.
- Lemon, K.P. Human nasal microbiota. Curr. Biol. 2020, 30, R1118–R1119.
- Gisler, A.; Korten, I.; de Hoogh, K.; Vienneau, D.; Frey, U.; Decrue, F.; BILD Study Group. Associations of air pollution and greenness with the nasal microbiota of healthy infants: A longitudinal study. Environ. Res. 2021, 202, 111633.
- Modi, S.; Inwati, G.K.; Gacem, A.; Saquib Abullais, S.; Prajapati, R.; Yadav, V.K.; Jeon, B.H. Nanostructured Antibiotics and Their Emerging Medicinal Applications: An Overview of Nanoantibiotics. Antibiotics 2022, 11, 708.
- Thangaleela, S.; Sundaram Sivamaruthi, B.; Kesika, P.; Bharathi, M.; Chaiyasut, C. Nasal Microbiota, Olfactory Health, Neurological Disorders and Aging—A Review. Microorganisms 2022, 10, 1405.
- Pal, G.; Ramirez, V.; Engen, P.A.; Naqib, A.; Forsyth, C.B.; Green, S.J.; Keshavarzian, A. Deep nasal sinus cavity microbiota dysbiosis in Parkinson’s disease. NPJ Park. Dis. 2021, 7, 1–10.
- Mariani, J.; Favero, C.; Spinazzè, A.; Cavallo, D.M.; Carugno, M.; Motta, V.; Bollati, V. Short-term particulate matter exposure influences nasal microbiota in a population of healthy subjects. Environ. Res. 2018, 162, 119–126.
- Yadav, V.K.; Malik, P.; Tirth, V.; Khan, S.H.; Yadav, K.K.; Islam, S.; Jeon, B.H. Health and Environmental Risks of Incense Smoke: Mechanistic Insights and Cumulative Evidence. J. Inflamm. Res. 2022, 15, 2665.
- Lynge Pedersen, A.M.; Belstrøm, D. The role of natural salivary defences in maintaining a healthy oral microbiota. J. Dent. 2019, 80, S3–S12.
- Sedghi, L.; DiMassa, V.; Harrington, A.; Lynch, S.V.; Kapila, Y.L. The oral microbiome: Role of key organisms and complex networks in oral health and disease. Periodontol. 2000 2021, 87, 107–131.
- Zhou, Z.; Zheng, D.; Wu, H.; Li, R.; Xu, S.; Kang, Y.; Qiao, J. Epidemiology of infertility in China: A population-based study. BJOG Int. J. Obstet. Gynaecol. 2018, 125, 432–441.
- Martin, S.; Foulon, A.; El Hage, W.; Dufour-Rainfray, D.; Denis, F. Is There a Link between Oropharyngeal Microbiome and Schizophrenia? A Narrative Review. Int. J. Mol. Sci. 2022, 23, 846.
- Marsh, P.D.; Do, T.; Beighton, D.; Devine, D.A. Influence of saliva on the oral microbiota. Periodontol. 2000 2016, 70, 80–92.
- Mohammed, H.; Varoni, E.M.; Cochis, A.; Cordaro, M.; Gallenzi, P.; Patini, R.; Rocchetti, V. Oral dysbiosis in pancreatic cancer and liver cirrhosis: A review of the literature. Biomedicines 2018, 6, 115.
- Sarkar, P.; Malik, S.; Laha, S.; Das, S.; Bunk, S.; Ray, J.G.; Saha, A. Dysbiosis of Oral Microbiota During Oral Squamous Cell Carcinoma Development. Front. Oncol. 2021, 11, 614448.
- Sureda, A.; Daglia, M.; Argüelles Castilla, S.; Sanadgol, N.; Fazel Nabavi, S.; Khan, H.; Nabavi, S.M. Oral microbiota and Alzheimer’s disease: Do all roads lead to Rome? Pharmacol. Res. 2020, 151, 104582.
- Ma, S.; Zhang, F.; Zhou, F.; Li, H.; Ge, W.; Gan, R.; Huang, Z. Metagenomic analysis reveals oropharyngeal microbiota alterations in patients with COVID-19. Signal Transduct. Target. Ther. 2021, 6, 1–11.
- Gasmi Benahmed, A.; Gasmi, A.; Doşa, A.; Chirumbolo, S.; Mujawdiya, P.K.; Aaseth, J.; Bjørklund, G. Association between the gut and oral microbiome with obesity. Anaerobe 2021, 70, 102248.
- Gao, Z.; Kang, Y.; Yu, J.; Ren, L. Human Pharyngeal Microbiome May Play a Protective Role in Respiratory Tract Infections. Genom. Proteom. Bioinform. 2014, 12, 144–150.
- Qin, T.; Zhang, F.; Zhou, H.; Ren, H.; Du, Y.; Liang, S.; Xu, J. High-Level PM2.5/PM10 exposure is associated with alterations in the human pharyngeal microbiota composition. Front. Microbiol. 2019, 10, 54.
- Li, X.; Sun, Y.; An, Y.; Wang, R.; Lin, H.; Liu, M.; Xiao, C. Air pollution during the winter period and respiratory tract microbial imbalance in a healthy young population in Northeastern China. Environ. Pollut. 2019, 246, 972–979.
- Shen, Y.; Liu, C.; Luo, J.; Wang, J.; Zhang, D. 16SrDNA-Based Detection Technology in Patients with Chronic Pharyngitis to Analyze the Distribution Characteristics of Pharyngeal Bacteria. J. Healthc. Eng. 2022, 2022, 5186991.
- Xin Pei Ho, E.; Ming Gemmy Cheung, C.; Sim, S.; Wenhan Chu, C.; Wilm, A.; Bitong Lin, C.; Hibberd, M. Human pharyngeal microbiota in age-related macular degeneration. PLoS ONE 2018, 13, e0201768.
- Yang, S.; Qiao, L.; Shi, J.; Xie, L.; Liu, Y.; Xiong, Y.; Liu, H. Clinical Study of Correlation for the Intestinal and Pharyngeal Microbiota in the Premature Neonates. Front. Pediatr. 2021, 9, 632573.
- Adar, S.D.; Huffnagle, G.B.; Curtis, J.L. The respiratory microbiome: An underappreciated player in the human response to inhaled pollutants? Ann. Epidemiol. 2016, 26, 355–359.
- Hamidou Soumana, I.; Carlsten, C. Air pollution and the respiratory microbiome. J. Allergy Clin. Immunol. 2021, 148, 67–69.
- Niemeier-Walsh, C.; Ryan, P.H.; Meller, J.; Ollberding, N.J.; Adhikari, A.; Reponen, T. Exposure to traffic-related air pollution and bacterial diversity in the lower respiratory tract of children. PLoS ONE 2021, 16, e0244341.
- Rylance, J.; Kankwatira, A.; Nelson, D.E.; Toh, E.; Day, R.B.; Lin, H.; Gordon, S.B. Household air pollution and the lung microbiome of healthy adults in Malawi: A cross-sectional study. BMC Microbiol. 2016, 16, 182.
- Thapa, A.; Kaushik, R.; Arora, S.; Jaglan, S.; Jaswal, V.; Yadav, V.K.; Singh, M.; Bains, A.; Chawla, P.; Khan, A.; et al. Biological Activity of Picrorhiza kurroa: A Source of Potential Antimicrobial Compounds against Yersinia enterocolitica. Int. J. Mol. Sci. 2022, 23, 14090.
More
Information
Subjects:
Biotechnology & Applied Microbiology
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.3K
Revisions:
3 times
(View History)
Update Date:
06 Dec 2022
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




