Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Silvana Mirella Aliberti | -- | 2868 | 2022-07-27 11:31:51 | | | |
| 2 | Jason Zhu | Meta information modification | 2868 | 2022-07-28 04:17:11 | | | | |
| 3 | Jason Zhu | -40 word(s) | 2828 | 2022-07-29 03:59:43 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Stefano, M.D.; Aliberti, S.M.; Ruggiero, A. Tribocorrosion in Dental Implants. Encyclopedia. Available online: https://encyclopedia.pub/entry/25579 (accessed on 08 February 2026).
Stefano MD, Aliberti SM, Ruggiero A. Tribocorrosion in Dental Implants. Encyclopedia. Available at: https://encyclopedia.pub/entry/25579. Accessed February 08, 2026.
Stefano, Marco De, Silvana Mirella Aliberti, Alessandro Ruggiero. "Tribocorrosion in Dental Implants" Encyclopedia, https://encyclopedia.pub/entry/25579 (accessed February 08, 2026).
Stefano, M.D., Aliberti, S.M., & Ruggiero, A. (2022, July 27). Tribocorrosion in Dental Implants. In Encyclopedia. https://encyclopedia.pub/entry/25579
Stefano, Marco De, et al. "Tribocorrosion in Dental Implants." Encyclopedia. Web. 27 July, 2022.
Copy Citation
Tribocorrosion is a current and very discussed theme in tribology and medicine for its impact on industrial applications. The phenomena are mainly oriented to the biological environment and, in particular, to medical devices such as hip prostheses, dental implants, knee joints, etc. The term tribocorrosion underlines the simultaneous action of wear and corrosion in a tribocouple. It has a non-negligible effect on the total loss of contact materials and the potential failure of the bio-couplings.
Dental Implant
Structure
Tribocorrosion
1. Dental Implant
Tribocorrosive effects assume a key role in artificial dental implants and therefore deserve to be studied within the experimental and theoretical approaches outlined in the previous sections. Dental implant surgery (arches, implants, plates) is a widespread technique, which has achieved an almost 90% success rate in terms of stability of the prosthesis, bone loss and presence of bacteria [1]. Thus, it is an ordinary procedure with high reliability, which is missing teeth and supporting oral tissues have traditionally been replaced with removable or fixed prostheses that allow the restoration of chewing function, phonetics and aesthetics, improving the quality of life of many patients and increasing demand for them in recent years. On the other hand, they are subjected to failure or dangerous events that could compromise the proper functioning of the prosthesis. Their research is therefore necessary, especially considering that the dental environment has its own characteristics and peculiarities that profoundly affect tribocorrosion, often making the analysis very difficult to perform.
2. Implant Structure
The implant is formed of a fixture that is a cylindrical screw, acting as an artificial root in contact with the bone; the crown or dental prosthesis, corresponding to the upper zone, represents the visible area of the total implant and the abutment, which connects the last two. In addition, the implant can provide, to fix beyond the components, a junction screw or can be cemented. The former is, currently, preferred because of the likely destruction of the cement layer and colonization of bacteria and because of less stress distribution to the implant [2]. Moreover, it can be monophasic or biphasic according to the number of operations realized as follows: for the first, all the implants will be installed in one operation, whereas for the second, the fixture and the remaining parts are collocated in different periods of time. The choice depends on the patient as well as on the distribution of the deformations [3]. Regarding the geometry, instead, the implants can assume the following many configurations:
In Figure 1, a biphasic implant with a head diameter of 4.4 mm and a length of 13 mm with the presence of a cutted zone is shown. The cutting area is an interesting zone because the incision has the function of facilitating the formation of the bone and reinforcing its stability. The surface topography [4] and the specific dimensions of the thread, as well as its type (buttress, reverse buttress, V-shape, sinusoidal, square), play a key role, as well as the upper diameter and the total length of the implant, in the contact conditions and stress/strain field [5]. The last impact on the life span of a prosthesis is as follows: the magnitude of the transmitted forces and the resulted contact pressures should be investigated in the different areas of the implant and in the surrounding bone and comparing the values with the ones coming from the adopted failure criteria. More precisely, the value of the forces should be not too high to avoid a potential overload and the rupture of implant/bone, and not too low according to the cited above Wolff law. Indeed, the bone remodels in response to the external load as follows: it means that if the forces are not big enough, stress shielding will occur with the reduction of bone density, causing issues such as inhibition of bone development, inflammation, or, in the worst case, the failure of the prosthesis [6]. Regarding, instead, the topographical properties, numerous studies confirmed the relationship between Ra (arithmetical roughness) and osseointegration as follows: an ideal range for the implantable surfaces was found to be between 1 and 2 µm [7][8]. Hence, a not completely smooth surface could be preferred, as follows: treatments such as acid etching, shot blasting and plasma spraying are all valid processes impacting the topography of the surface [9]. On the contrary, greater roughness determines a lower real contact area [10] and consequently higher pressures in localized zones. In addition, the probability of bacterial adhesion is higher [11] than that which can develop a biofilm, i.e., a complex structure of microbiological cells enclosed essentially in a polysaccharide matrix [12], with variable chemical nature.
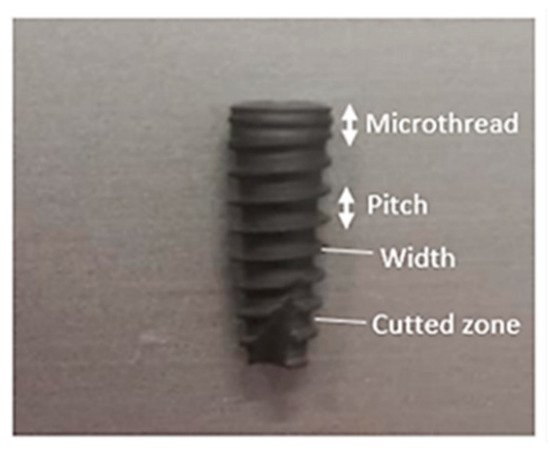
Figure 1. Example of a dental implant with cutted zone.
3. Dental Tribocorrosion
Although tribocorrosion is a relatively recent research field, many scientists have carried out different tests from experimental, numerical and clinical points of view. In the dental case, many mechanical and chemical variables should be considered, such as the contact load, the frequency, the environment’s chemical composition and pH, the contact surfaces topography and properties and the influence of eventual external microorganisms [13].
3.1. The Effect of the Regime of Sliding
Firstly, dental tribocorrosion occurs because of the continuous exchange of load, for example during mastication and the corrosion due to the oral environment causes teeth to wear. The tribochemical-involved are very complex and not fully understood and modeled, even if some interesting investigations are found in the scientific literature. Barril et al. [15] in 2002, by using an experimental procedure focused on fretting corrosion; they were interested in the main affecting variables, both electrochemical and mechanical, such as potential, normal force, frequency and so on the wear phenomena acting in the analyzed tribosystems. The interesting aspect of their research was the study of these properties according to specific fretting regimes as well as the kind of wear established (for instance, the presence of a third body referred to as localized current peaks). They found that the dependence on the slip amplitude was crucial since it affects the potential formation of an oxide protective layer as follows: a large slip amplitude (>10 µm) is obviously associated with an increased chemical reactivity and, in addition, the coefficient of friction and wear are correlated especially with applied potential. This approach highlights an innovative point of view, i.e., to analyze the change in the tribological response of materials to different fretting regimes and external conditions.
3.2. The Influence of the Solution Chemical Composition
Two years later, Contu et al. [16] focused their attention during an abrasion test, analyzing the potential and repassivation occurrence of pure titanium and Ti6Al4V alloy in a bovine calf serum with variable pH. The aim was to investigate the different behaviors of materials, which are very common in dentistry, for a precise solution type. The results showed similar electrochemical behavior between the materials, but the commercially pure titanium exhibited a faster propensity to repassivation. In any case, it is important to underline that each experiment strongly influences the chemical composition of the working solution, affecting the tribocorrosive behavior of the studied coupling. A clear example in dentistry is the saliva, which is chemically variable according to human habits (food assumed, smoking, etc.). In 2005, Ribeiro et al. [17] were interested in recreating the oral area with artificial saliva combined with some additives (citric acid, organic inhibitors) and analyzing the tribocorrosion behavior. The tests were performed for more than 10.000 cycles and in environmental conditions very close to the oral cavity, where the implants are constantly submitted to mechanical stress. The different additives and solutions influenced the material loss (the citric acid was the worst), confirming the great influence of the chemical composition of the solution on wear phenomena. On the contrary, Vieira et al. in 2006 [18], by electromechanical tests on pure titanium in artificial saliva solutions, varied in compositions thanks to specific inhibitors, found the opposite, as follows: the tribolayers with citric acid or anodic inhibitor became more stable with a lower coefficient of friction and lower current. This underlines the absence of a unique trend in the results, caused by the many variables involved, which requires a more intensive experimental investigation. Moreover, pH is another relevant variable and it is known that it is generally in the range of 6.2–7.4 (neutral solution), different from patient to patient and from different zones of the oral cavity but, in any case, strongly influencing the tribocorrosion occurrence. In fact, Mathew et al. in 2012 [19] evaluated the combined effect of corrosion and mechanical wear for the following three pH values: between 3–6 and 9, finding that the worst, because of the incomplete formation of a protective passive layer, is exactly the second. This result is almost surprising since the worst conditions did not occur when the solution was acidic (under 2 pH), but when it was neutral, which is the typical value of the mouth. The direct consequence is the high probability of tribocorrosion occurrence in the oral cavity. Together with pH, the fluoride concentration derived from common toothpaste can also have a negative effect on tribocorrosion resistance, as confirmed by Golvano et al. [20] and on the active dissolution of titanium alloys, as confirmed by Licausi et al. [21]. This demonstrates the aggressivity of the external area to biological objects such as the dental prosthesis. In Golvano et al. work, a near-β Ti13Nb13Zr alloy was investigated in place of the common pure titanium or Ti6Al4V alloy. The choice depends on the diffusion of toxic elements of these samples and therefore the necessity of the development new titanium samples as β and near-β titanium alloys, whose strength-to-weight ratio and excellent biocompatibility determined their diffusion in the orthodontic field. Nevertheless, their wear behavior is not so excellent and not away from the titanium samples. Lastly, Teixeira et al. [22] detected the change in solution viscosity, which is an important factor from both a mechanical point of view, for the lubrication regime imposed and chemical, for the corrosion reactions, derived from the effect of particular biomolecules such as albumin, urea and mucin in artificial saliva, as well as the tribocorrosion response of the samples, with the result that the presence of the mucin leads to the lowest wear coefficients.
3.3. The Impact of Specific Surface Treatments
An alternative approach could be driven by contact surface treatment. Regarding this, Alves et al. in 2013 [23] stated that, by applying an anodizing treatment on titanium surfaces, a homogenous oxide film capable of protecting the sample was formed. From a chemical point of view, the anodizing was performed in an electrolyte containing β-glycerophosphate and calcium acetate. The latter, in terms of concentration, was evaluated as relevant for tribocorrosion behavior because of microstructural changes. The porous structure, obtained after the treatment, not only resulted in lower mechanical damage but also can be crucial for better osteointegration allowing, the bone to build inside the pores. In any case, to achieve complete acceptability, the modified implants should be inserted into real systems where, more likely, other aspects like bacterial attack (Streptococcus Mutans) or cellular response, adhesion and proliferation, should be also considered. Alves, in another research published in 2015 [24], confirmed the beneficial effects of calcium and phosphorus Ti-oxide films again for wear contrast and osteoblast interactions. The same was formulated by Geringer et al. [25] regarding the acid etching technique adopted for improving sample properties, by Vilhena et al. [26] for the Selective Laser Melting Technique, which showed lower passive current density and by Mindivian et al. [27] about the pulsed Plasma Nitriding Process and its direct consequences on the lower coefficient of friction, higher OCP and lower wear volume loss. It is almost clear that a direct correlation between sample treatment and wear effects does not occur as follows: Some conditions impact chemical wear, in correspondence to lower current values, others on mechanical wear and on the friction of the tribosystem. Moreover, the type of wear established (abrasion, adhesion, fretting, three-body) is also crucial for correct tribocorrosion estimation. Overall, the surface preparation, in terms of topography, roughness and coatings, becomes crucial for a long-life implant, precluding postoperative complications and expenses [28] since tribocorrosion was considered one of the most possible failure causes [29] since the long-term production of toxic ions and local/global inflammation in the oral cavity cumulate their impact on the implant and the surrounding bone, causing, in the worst cases, the failure.
3.4. The Tribocorrosion: A Multivariable Phenomenon
Many investigations [30] tried to depict wear maps, describing them as a very useful tool to provide a reference for wear predictions in dental implants. Wang et al. [31] in 2018 analyzed the trend of volume loss with load and noticed that the material loss increased in the presence of corrosion proportionally to the load applied. This can be easily demonstrated by considering the relation between load and potential as follows: the higher the load, the lower the potential and the greater the corrosion wear. As well as the former, the potential also impacts the propagation of wear, as analyzed by Borras et al. in 2019 as follows [32]: for low passive conditions, the wear was low, whereas for high passive conditions it was the opposite, as expected, since the latter compromises the protection of the oxide layer. An interesting outcome is the capacity of the compacted wear debris, at open circuit conditions, of supporting the external load, reducing in this way the total wear of the coupling. Another key variable is the masticatory frequency, as analyzed by Alfaro et al. [33] in 2019; they found that it has a relationship with oxide layer stability, understanding that the lower frequencies (1–2 Hz) allow for greater repassivation, in contrast to the higher ones at 4 Hz, where the passive film resulted in interruption. The effect is the drastic drop of potential toward negative values. The results can be easily explained by considering that, for high frequencies, the available time for repassivation is shorter and, probably, not sufficient. In reference to the dental environment, where the load and the frequencies of mastication or bruxism are variable and the loads multidirectional, these results become relevant for implant longevity. Regarding the choice of the material instead, Mehkri et al. [34] tried, in 2021, to compare the very common grade 2 or 4 or 5 titanium implants with Zirconia Toughened Alumina and Yttria Stabilized Zirconia. The tests pointed out that the latter behaves better against wear and, therefore, can be considered a valid alternative accounting for the that titanium implants, which have the drawback of dangerous ion diffusion [35]. Another study, always in 2021 and referred to as the material choice, conducted by Ramachandran et al. [36], focalized on the ideal combination of titanium and zirconium as Ti + 5% Zr, which exhibited improved corrosion and wear resistance behavior. This does not happen for 10–15% of zirconium, where the tribocorrosion response was worst. The reason comes from the function performed by Zr as follows: it increases the hardness of the alloy, but a higher value causes microstructural changes characterized by an irregular topography, which does not permit the formation of a uniform oxide layer. Therefore, each aspect should be kept in mind when a new sample is realized. The same comparison was performed by Sikora et al. [37] with the following equal outcomes: the best performing were the Zr/Ti ones, i.e., zirconium for the abutment and titanium for the implant. Interesting is also the potential application of TiO2 nanotubes (NTs), adopted for the improvement of osteointegration and reduction of infection released. Regarding this, Rossi et al., study [38] showed an enhanced tribocorrosion performance (in terms of adhesion strength and hardness) due to the growth of a nano-thick oxide film. Certainly, other particular elements [39] can also be chosen (as a coating, for example), such as niobium-based thin films, which, combined with carbon (NiC), provide optimal protective efficiency (anti-wear and anti-corrosion) and osteogenic potential (bioactivity in terms of cellular attachment, mineralization and differentiation) as stated by Xu et al.
3.5. The Future Tendencies
Most of these studies were performed by experimental techniques, but other approaches are also adopted similar to the numerical ones, regarding, for instance, the changes in bone according to specified loads [40] or clinical regarding bone loss evaluation [41] in a long-term evaluation by radiographic image. Interesting and innovative is the method suggested by Barao et al. [42] for the use of the acoustic emission technique, a non-destructive and non-intrusive approach, instead of the classical test rig, providing results with the same efficiency and accuracy. Moreover, the procedures and the models explained above should be coupled with instruments such as SEM [43] (Scanning electron microscope) or confocal microscopy. Indeed, they guarantee a deeper investigation regarding the topography and the chemical structure of the implant. For example, by SEM it is possible to evaluate the potential osteointegration of an implant removed (different zones of bone anchorage) or the element composition of the oxide layer (partial or complete passivation) and other important analyses. More specific studies are carried out on the surface wear [44][45][46][47][48] in order to estimate the wear type, chemical elements and composites formed after the tribocorrosion impact. In particular, the comparison between natural teeth and artificial samples could be resulted very interesting for validating a specific material. What was discussed underlines the abundance of aspects which can be developed, experimentally, numerically and especially clinically, representing, in this way, the new future tendencies.
References
- Albrektsson, T.; Zarb, G.; Worthington, P.; Eriksson, A.R. Available online: https://pubmed.ncbi.nlm.nih.gov/3527955/ (accessed on 1 April 2022).
- Lee, J.-H.; Jang, H.Y.; Lee, S.Y. Finite Element Analysis of Dental Implants with Zirconia Crown Restorations: Conventional Cement-Retained vs. Cementless Screw-Retained. Materials 2021, 14, 2666.
- Paracchini, F.I.L.; Angelis, F.D.; Cielo, A.; Orefici, A.; Spitaleri, D.; Santacroce, L.; Gheno, E.; Palermo, A. Biomechanical behaviour of a jawbone loaded with a prosthetic system supported by monophasic and biphasic implants. Oral Implantol. 2016, 9, 65–70.
- Affatato, S.; Ruggiero, A. Surface analysis on revised hip implants with stem taper for wear and failure incidence evaluation: A first investigation. Measurement 2019, 145, 38–44.
- Mahajan, S.; Patil, S. Application of finite element analysis to optimizing dental implant. Int. Res. J. Eng. Technol. (IRJET) 2016, 3, 850–856.
- Lane, J.M.; Mait, J.E.; Unnanuntana, A.; Hirsch, B.P.; Shaffer, A.D.; Shonuga, O.A. Materials in Fracture Fixation. Compr. Biomater. 2011, 6, 219–235.
- James, G.A.; Boegli, L.; Hancock, J.; Bowersock, L.; Parker, A.; Kinney, B.M. Bacterial Adhesion and Biofilm Formation on Textured Breast Implant Shell Materials. Aesthetic Plast. Surg. 2019, 43, 490–497.
- Wennerberg, A.; Albrektsson, T. Effects of titanium surface topography on bone integration: A systematic review. Clin. Oral Implant. Res. 2009, 20, 172–184.
- Astarita, A.; Rubino, F.; Carlone, P.; Ruggiero, A.; Leone, C.; Genna, S.; Merola, M.; Squillace, A. On the Improvement of AA2024 Wear Properties through the Deposition of a Cold-Sprayed Titanium Coating. Metals 2016, 6, 185.
- Žugelj, B.B.; Kalin, M. In-situ Observations of a Multi-Asperity Real Contact Area on a Submicron Scale. J. Mech. Eng. 2017, 63, 351–362.
- Rocha, L.A.; Oliveira, F.; Cruz, H.V.; Sukotjo, C.; Mathew, M.T. bio-tribocorrosion in dental applications. In Bio-Tribocorrosion in Biomaterials and Medical Implants; Woodhead Publishing Limited: Sawston, UK, 2013; pp. 223–249.
- Almaguer-Flores, A. Biofilms in the oral environment. In Bio-Tribocorrosion in Biomaterials and Medical Implants; Woodhead Publishing Limited: Sawston, UK, 2013; pp. 169–186.
- Cruz, H.V.; Souza, J.C.M.; Henriques, M.; Rocha, L.A. Tribocorrosion and Bio-Tribocorrosion in the Oral Environment: The Case of Dental Implants. In Biomedical Tribology; Davim, J.P., Ed.; Nova Science Publishers: New York, NY, USA, 2011.
- Lanza, A.; Ruggiero, A.; Sbordone, L. Tribology and Dentistry: A Commentary. Lubricants 2019, 7, 52.
- Barril, S.; Debaud, N.; Mischler, S.; Landolt, D. A tribo-electrochemical apparatus for in vitro investigation of fretting–corrosion of metallic implant materials. Wear 2002, 252, 744–754.
- Contu, F.; Elsener, B.; Böhni, H. A study of the potentials achieved during mechanical abrasion and the repassivation rate of titanium and Ti6Al4V in inorganic buffer solutions and bovine serum. Electrochim. Acta 2004, 50, 33–41.
- Ribeiro, A.R.L.; Rocha, L.A.; Ariza, E.; Gomes, J.R.; Celis, J.-P. Tribocorrosion behaviour of titanium grade 2 in alternative linear regime of sliding in artificial saliva solutions. In Proceedings of the European Corrosion Congress (EUROCORR ’05), Lisbon, Portugal, 4–8 September 2005; pp. 1–10.
- Vieira, A.; Ribeiro, A.; Rocha, L.; Celis, J. Influence of pH and corrosion inhibitors on the tribocorrosion of titanium in artificial saliva. Wear 2006, 261, 994–1001.
- Mathew, M.T.; Abbey, S.; Hallab, N.J.; Hall, D.J.; Sukotjo, C.; Wimmer, M.A. Influence of pH on the tribocorrosion behavior of CpTi in the oral environment: Synergistic interactions of wear and corrosion. J. Biomed. Mater. Res. Part B Appl. Biomater. 2012, 100B, 1662–1671.
- Golvano, I.; Garcia, I.; Conde, A.; Tato, W.; Aginagalde, A. Influence of fluoride content and pH on corrosion and tribocorrosion behaviour of Ti13Nb13Zr alloy in oral environment. J. Mech. Behav. Biomed. Mater. 2015, 49, 186–196.
- Licausi, M.P.; Muñoz, A.I.; Borrás, V.A. Tribocorrosion mechanisms of Ti6Al4V biomedical alloys in artificial saliva with different pHs. J. Phys. D Appl. Phys. 2013, 46, 404003.
- Teixeira, H.; Branco, A.C.; Rodrigues, I.; Silva, D.; Cardoso, S.; Colaço, R.; Serro, A.P.; Figueiredo-Pina, C.G. Effect of albumin, urea, lysozyme and mucin on the triboactivity of Ti6Al4V/zirconia pair used in dental implants. J. Mech. Behav. Biomed. Mater. 2021, 118, 104451.
- Alves, A.C.; Oliveira, F.; Wenger, F.; Ponthiaux, P.; Celis, J.-P.; Rocha, L.A. Tribocorrosion behaviour of anodic treated titanium surfaces intended for dental implants. J. Phys. D Appl. Phys. 2013, 46, 404001.
- Alves, S.A.; Bayón, R.; De Viteri, V.S.; Garcia, M.P.; Igartua, A.; Fernandes, M.H.; Rocha, L.A. Tribocorrosion Behavior of Calcium- and Phosphorous-Enriched Titanium Oxide Films and Study of Osteoblast Interactions for Dental Implants. J. Bio-Tribo-Corros. 2015, 1, 23.
- Geringer, J.; Demanget, N.; Pellier, J. From acid etching treatments to tribocorrosive properties of dental implants: Do some experimental results on surface treatments have an influence on the tribocorrosion behaviour of dental implants? J. Phys. D Appl. Phys. 2013, 46, 404005.
- Vilhena, L.M.; Shumayal, A.; Ramalho, A.; Ferreira, J.A.M. Tribocorrosion Behaviour of Ti6Al4V Produced by Selective Laser Melting for Dental Implants. Lubricants 2020, 8, 22.
- Mindivan, F.; Mindivan, H. Microstructure and Tribocorrosion Properties of Pulsed Plasma Nitrided Cast CoCr Alloy for Dental Implant Applications. Acta Phys. Pol. A 2018, 134, 192–195.
- Kunrath, M.F.; Muradás, T.C.; Penha, N.; Campos, M.M. Innovative surfaces and alloys for dental implants: What about biointerface-safety concerns? Dent. Mater. 2021, 37, 1447–1462.
- Revathi, A.; Borrás, A.D.; Muñoz, A.I.; Richard, C.; Manivasagam, G. Degradation mechanisms and future challenges of titanium and its alloys for dental implant applications in oral environment. Mater. Sci. Eng. C 2017, 76, 1354–1368.
- Holmes, D.; Sharifi, S.; Stack, M.M. Tribo-corrosion of steel in artificial saliva. Tribol. Int. 2014, 75, 80–86.
- Wang, Z.; Zhou, Y.; Wang, H.; Li, Y.; Huang, W. Tribocorrosion behavior of Ti-30Zr alloy for dental implants. Mater. Lett. 2018, 218, 190–192.
- Borrás, A.D.; Buch, A.R.; Cardete, A.R.; Navarro-Laboulais, J.; Muñoz, A.I. Chemo-mechanical effects on the tribocorrosion behavior of titanium/ceramic dental implant pairs in artificial saliva. Wear 2019, 426–427, 162–170.
- Alfaro, M.F.; Rossman, P.K.; Marques, I.D.S.V.; Dube, A.; Takoudis, C.; Shokuhfar, T.; Mathew, M.T.; Sukotjo, C. Interface Damage in Titanium Dental Implant Due to Tribocorrosion: The Role of Mastication Frequencies. J. Bio-Tribo-Corros. 2019, 5, 81.
- Mehkri, S.; Abishek, N.; Sumanth, K.S.; Rekha, N. Study of the Tribocorrosion occurring at the implant and implant alloy Interface: Dental implant materials. Mater. Today Proc. 2021, 44, 157–165.
- Noronha Oliveira, M.; Schunemann, W.V.H.; Mathew, M.T.; Henriques, B.; Magini, R.S.; Teughels, W.; Souza, J.C.M. Can degradation products released from dental implants affect peri-implant tissues? J. Periodontal Res. 2018, 53, 1–11.
- Ramachandran, R.A.; Barão, V.A.R.; Matos, A.O.; Cordeiro, J.M.; Grandini, C.R.; Sukotjo, C.; Mathew, M.T. Suitability of Ti–Zr Alloy for Dental Implants: Tribocorrosion Investigation. J. Bio-Tribo-Corros. 2021, 7, 152.
- Sikora, C.L.; Alfaro, M.F.; Yuan, J.C.-C.; Barao, V.A.; Sukotjo, C.; Mathew, M.T. Wear and Corrosion Interactions at the Titanium/Zirconia Interface: Dental Implant Application. J. Prosthodont. 2018, 27, 842–852.
- Alves, S.A.; Rossi, A.; Ribeiro, A.; Toptan, F.; Pinto, A.; Shokuhfar, T.; Celis, J.-P.; Rocha, L. Improved tribocorrosion performance of bio-functionalized TiO2 nanotubes under two-cycle sliding actions in artificial saliva. J. Mech. Behav. Biomed. Mater. 2018, 80, 143–154.
- Xu, Z.; Yate, L.; Qiu, Y.; Aperador, W.; Coy, E.; Jiang, B.; Moya, S.; Wang, G.; Pan, H. Potential of niobium-based thin films as a protective and osteogenic coating for dental implants: The role of the nonmetal elements. Mater. Sci. Eng. C 2019, 96, 166–175.
- Sotto-Maior, B.S.; Mercuri, E.G.F.; Senna, P.M.; Assis, N.M.S.P.; Francischone, C.E.; Cury, A.A.D.B. Evaluation of bone remodeling around single dental implants of different lengths: A mechanobiological numerical simulation and validation using clinical data. Comput. Methods Biomech. Biomed. Eng. 2016, 19, 699–706.
- Lee, D.-W.; Choi, Y.-S.; Park, K.H.; Kim, C.-S.; Moon, I.-S. Effect of microthread on the maintenance of marginal bone level: A 3-year prospective study. Clin. Oral Implant. Res. 2007, 18, 465–470.
- Barão, V.A.; Ramachandran, R.A.; Matos, A.O.; Badhe, R.V.; Grandini, C.R.; Sukotjo, C.; Ozevin, D.; Mathew, M. Prediction of tribocorrosion processes in titanium-based dental implants using acoustic emission technique: Initial outcome. Mater. Sci. Eng. C 2021, 123, 112000.
- Barros, C.D.d.R.; Rocha, J.C.; Bastos, I.N.; Gomes, J.A.d.C.P. Tribocorrosion Resistance of Dental Implant Alloys—Assessment of cp-Ti, Ti6Al4V, and NiCr in Neutral and Acidified Saliva. J. Bio-Tribo-Corros. 2021, 7, 73.
- Ruggiero, A.; D’Amato, R.; Sbordone, L.; Haro, F.B.; Lanza, A. Experimental Comparison on Dental BioTribological Pairs Zirconia/Zirconia and Zirconia/Natural Tooth by Using a Reciprocating Tribometer. J. Med. Syst. 2019, 43, 97.
- Ruggiero, A.; Zhang, H. Editorial: Biotribology and Biotribocorrosion Properties of Implantable Biomaterials. Front. Mech. Eng. 2020, 6, 17.
- Ruggiero, A.; Sicilia, A. Lubrication modeling and wear calculation in artificial hip joint during the gait. Tribol. Int. 2020, 142, 105993.
- Ruggiero, A.; Sicilia, A.; Affatato, S. In silico total hip replacement wear testing in the framework of ISO 14242-3 accounting for mixed elasto-hydrodynamic lubrication effects. Wear 2020, 460, 203420.
- Ruggiero, A.; Sicilia, A. A mixed elasto-hydrodynamic lubrication model for wear calculation in artificial hip joints. Lubricants 2020, 8, 72.
More
Information
Subjects:
Health Care Sciences & Services
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
959
Revisions:
3 times
(View History)
Update Date:
29 Jul 2022
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




