
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Shandeigh N Berry | -- | 1334 | 2022-07-26 21:45:33 | | | |
| 2 | Conner Chen | + 5 word(s) | 1339 | 2022-07-27 03:46:23 | | |
Video Upload Options
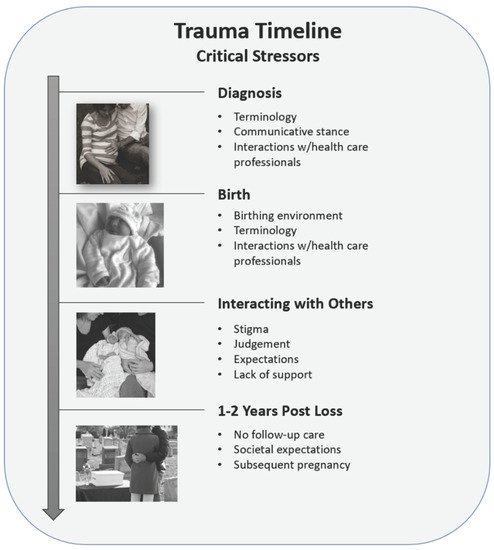
Perinatal loss, the loss of a fetus or neonate between conception and 28 days after birth, is a worldwide phenomenon impacting millions of individuals annually. Whether due to miscarriage, stillbirth, life-limiting fetal diagnoses, or neonatal death, up to 60% of bereaved parents exhibit symptoms of depression, anxiety, and posttraumatic stress disorder.
1. Trauma of the Diagnosis
2. Trauma of the Delivery and Birth
3. Trauma of Interacting with Others
4. Trauma following the Loss Experience
5. Implications for Practice
Health care professionals have the responsibility of facilitating a healthy transition from “healthy pregnancy” to “non-viable pregnancy”. Such a responsibility is admittedly a herculean task. It is necessary to recognize perinatal loss as a traumatic event. In recognizing the trauma of perinatal loss, health care professionals can begin to address parents’ unique biopsychosocial needs throughout the perinatal loss experience. Utilization of a trauma-informed care (TIC) framework equips health care professionals with the specialized tools necessary to mitigate the risk of further traumatizing grieving parents. Within the TIC framework, health care professionals may improve parents’ experiences by acknowledging the loss of both parents; normalizing both parents’ emotional responses; facilitating memory making, rituals, and ceremonies; and providing follow-up care for at least one year following the loss.
Pregnancies subsequent to perinatal loss are often wrought with anxiety and PTSD. Identifying pregnant persons with a history of gestational loss is necessary to recognize those who require additional psychological and emotional support throughout the pregnancy. Developing automated flagging systems in electronic health records may facilitate early identification and resource allocation to those with prior gestational loss. Providing early interventions and emotional support may decrease the anxiety and trauma of pregnancy subsequent to gestational loss.
References
- Berry, S.N.; Severtsen, B.; Davis, A.; Nelson, L.; Hutti, M.H.; Oneal, G. The impact of anencephaly on parents: A mixed-methods study. Death Stud. 2021, 1–10.
- Gillis, C.; Wheatley, V.; Jones, A.; Roland, B.; Gill, M.; Marlett, N.; Shklarov, S. Stillbirth, still life: A qualitative patient-led study on parents’ unsilenced stories of stillbirth. Bereave. Care 2020, 39, 124–132.
- Chavez, M.S.; Handley, V.; Jones, R.L.; Eddy, B.; Poll, V. Men’s Experiences of Miscarriage: A Passive Phenomenological Analysis of Online Data. J. Loss Trauma 2019, 24, 664–677.
- Denney-Koelsch, E.; Cote-Arsenault, D. Life-limiting fetal conditions and pregnancy continuation: Parental decision-making processes. BMJ Support. Palliat. Care 2021, 1–7.
- Kurz, M.R. When Death Precedes Birth: The Embodied Experiences of Women with a History of Miscarriage or Stillbirth—A Phenomenological Study Using Artistic Inquiry. Am. J. Dance Ther. 2020, 42, 194–222.
- Guclu, O.; Senormanci, G.; Tuten, A.; Gok, K.; Senormanci, O. Perinatal Grief and Related Factors After Termination of Pregnancy for Fetal Anomaly: One-Year Follow-up Study. Arch. Neuropsychiatry 2021, 58, 221–227.
- Smith, L.K.; Dickens, J.; Atik, R.B.; Bevan, C.; Fisher, J.; Hinton, L. Parents’ experiences of care following the loss of a baby at the margins between miscarriage, stillbirth and neonatal death: A UK qualitative study. BJOG Int. J. Obstet. Gynaecol. 2020, 127, 868–874.
- Markin, R.D. “Ghosts” in the womb: A mentalizing approach to understanding and treating prenatal attachment disturbances during pregnancies after loss. Psychotherapy. 2018, 55, 275–288.
- Ironside, P.M. New Pedagogies for Teaching Thinking: The Lived Experiences of Students and Teachers Enacting Narrative Pedagogy. J. Nurs. Educ. 2003, 42, 509–516.
- Ordóñez, E.F.; Díaz, C.R.; Gil, I.M.M.; Manzanares, M.T.L. Post-traumatic stress disorder after subsequent birth to a gestational loss: An observational study. Salud Ment. 2020, 43, 129–136.
- Richards, J.; Graham, R.; Embleton, N.D.; Campbell, C.; Rankin, J. Mothers’ perspectives on the perinatal loss of a co-twin: A qualitative study. BMC Pregnancy Childbirth 2015, 15, 143.
- Jones, K.; Robb, M.; Murphy, S.; Davies, A. New understandings of fathers’ experiences of grief and loss following stillbirth and neonatal death: A scoping review. Midwifery 2019, 79, 102531.
- Westby, C.L.; Erlandsen, A.R.; Nilsen, S.A.; Visted, E.; Thimm, J.C. Depression, anxiety, PTSD, and OCD after stillbirth: A systematic review. BMC Pregnancy Childbirth 2021, 21, 782.
- Martin, C.J.H.; Patterson, J.; Paterson, C.; Welsh, N.; Dougall, N.; Karatzias, T.; Williams, B. ICD-11 complex Post Traumatic Stress Disorder (CPTSD) in parents with perinatal bereavement: Implications for treatment and care. Midwifery 2021, 96, 102947.
- Krosch, D.J.; Shakespeare-Finch, J. Grief, traumatic stress, and posttraumatic growth in women who have experienced pregnancy loss. Psychol. Trauma Theory Res. Pract. Policy 2017, 9, 425–433.




