
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Giovanni Ciccarelli | + 4126 word(s) | 4126 | 2022-01-04 07:44:55 | | | |
| 2 | Bruce Ren | Meta information modification | 4126 | 2022-01-18 01:54:06 | | |
Video Upload Options
Advancements in clinical management, pharmacological therapy and interventional procedures have strongly improved the survival rate for cardiovascular diseases (CVDs). Nevertheless, the patients affected by CVDs are more often elderly and present several comorbidities such as atrial fibrillation, valvular heart disease, heart failure, and chronic coronary syndrome. Standard treatments are frequently not available for “frail patients”, in particular due to high surgical risk or drug interaction. In the past decades, novel less-invasive procedures such as transcatheter aortic valve implantation (TAVI), MitraClip or left atrial appendage occlusion have been proposed to treat CVD patients who are not candidates for standard procedures. These procedures have been confirmed to be effective and safe compared to conventional surgery, and symptomatic thromboembolic stroke represents a rare complication. However, while the peri-procedural risk of symptomatic stroke is low, several studies highlight the presence of a high number of silent ischemic brain lesions occurring mainly in areas with a low clinical impact. The silent brain damage could cause neuropsychological deficits or worse, a preexisting dementia, suggesting the need to systematically evaluate the impact of these procedures on neurological function.
1. Introduction
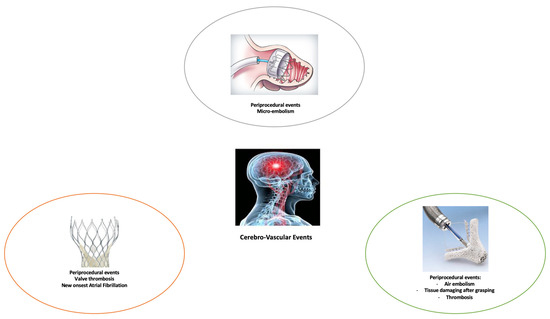
2. Percutaneous Transcatheter Procedures and Risk of Cerebral Ischemia and Stroke
2.1. Transcatheter Aortic Valve Replacement (TAVR)
2.2. Mitral Valve Repair and Replacement
2.3. Differences in New Cerebral Lesions after TEER vs. TAVR Procedures
2.4. Left Atrial Appendage Occlusion
References
- Korn-Lubetzki, I.; Farkash, R.; Pachino, R.M.; Almagor, Y.; Tzivoni, D.; Meerkin, D. Incidence and risk factors of cerebrovascular events following cardiac catheterization. J. Am. Heart Assoc. 2013, 2, e000413.
- Segal, A.Z.; Abernethy, W.B.; Palacios, I.F.; BeLue, R.; Rordorf, G. Stroke as a complication of cardiac catheterization: Risk factors and clinical features. Neurology 2001, 56, 975–977.
- Fuchs, S.; Stabile, E.; Kinnaird, T.D.; Mintz, G.S.; Gruberg, L.; Canos, D.A.; Pinnow, E.E.; Kornowski, R.; Suddath, W.O.; Satler, L.F. Stroke complicating percutaneous coronary interventions: Incidence, predictors, and prognostic implications. Circulation 2002, 106, 86–91.
- Cho, S.M.; Deshpande, A.; Pasupuleti, V.; Hernandez, A.V.; Uchino, K. Radiographic and clinical brain infarcts in cardiac and diagnostic procedures a systematic review and meta-analysis. Stroke 2017, 48, 2753–2759.
- Bittl, J.A.; Caplan, L.R. Stroke after percutaneous coronary interventions. J. Am. Coll. Cardiol. 2004, 43, 1168–1169.
- Dukkipati, S.; O’Neill, W.W.; Harjai, K.J.; Sanders, W.P.; Deo, D.; Boura, J.A.; Bartholomew, B.A.; Yerkey, M.W.; Sadeghi, H.M.; Kahn, J.K. Characteristics of cerebrovascular accidents after percutaneous coronary interventions. J. Am. Coll. Cardiol. 2004, 43, 1161–1167.
- Keeley, E.C.; Grines, C.L. Scraping of aortic debris by coronary guiding catheters: A prospective evaluation of 1000 cases. J. Am. Coll. Cardiol. 1998, 32, 1861–1865.
- Eggebrecht, H.; Oldenburg, O.; Dirsch, O.; Haude, M.; Baumgart, D.; Welge, D.; Herrmann, J.; Arnold, G.; Schmid, K.W.; Erbel, R. Potential embolization by atherosclerotic debris dislodged from aortic wall during cardiac catheterization: Histologic and clinical findings in 7621 patients. Catheter. Cardiovasc. Interv. 2000, 49, 389–394.
- Nusca, A.; Bressi, E.; Colaiori, I.; Miglionico, M.; Di Sciascio, G. Antiplatelet therapy in valvular and structural heart disease interventions. Cardiovasc. Diagn. Ther. 2018, 8, 578–593.
- Schmidt, T.; Akdag, O.; Wohlmuth, P.; Thielsen, T.; Schewel, D.; Schewel, J.; Alessandrini, H.; Kreidel, F.; Bader, R.; Romero, M.; et al. Histological Findings and Predictors of Cerebral Debris from Transcatheter Aortic Valve Replacement: The ALSTER Experience. J. Am. Heart Assoc. 2016, 5.
- Pagnesi, M.; Regazzoli, D.; Ancona, M.B.; Mangieri, A.; Lanzillo, G.; Giannini, F.; Buzzatti, N.; Prendergast, B.D.; Kodali, S.; Lansky, A.J.; et al. Cerebral Embolic Risk during Transcatheter Mitral Valve Interventions: An Unaddressed and Unmet Clinical Need? JACC Cardiovasc. Interv. 2018, 11, 517–528.
- Vermeer, S.E.; Longstreth, W.T.; Koudstaal, P.J. Silent brain infarcts: A systematic review. Lancet Neurol. 2007, 6, 611–619.
- Barber, P.A.; Hach, S.; Tippett, L.J.; Ross, L.; Merry, A.F.; Milsom, P. Cerebral ischemic lesions on diffusion-weighted imaging are associated with neurocognitive decline after cardiac surgery. Stroke 2008, 39, 1427–1433.
- Vermeer, S.E.; Prins, N.D.; den Heijer, T.; Hofman, A.; Koudstaal, P.J.; Breteler, M.M.B. Silent Brain Infarcts and the Risk of Dementia and Cognitive Decline. N. Engl. J. Med. 2003, 348, 1215–1222.
- Kahlert, P.; Al-Rashid, F.; Döttger, P.; Mori, K.; Plicht, B.; Wendt, D.; Bergmann, L.; Kottenberg, E.; Schlamann, M.; Mummel, P.; et al. Cerebral embolization during transcatheter aortic valve implantation: A transcranial doppler study. Circulation 2012, 126, 1245–1255.
- Ghanem, A.; Müller, A.; Nähle, C.P.; Kocurek, J.; Werner, N.; Hammerstingl, C.; Schild, H.H.; Schwab, J.O.; Mellert, F.; Fimmers, R.; et al. Risk and Fate of Cerebral Embolism after Transfemoral Aortic Valve Implantation. A Prospective Pilot Study with Diffusion-Weighted Magnetic Resonance Imaging. J. Am. Coll. Cardiol. 2010, 55, 1427–1432.
- Baumgartner, H.; Falk, V.; Bax, J.J.; De Bonis, M.; Hamm, C.; Holm, P.J.; Iung, B.; Lancellotti, P.; Lansac, E.; Muñoz, D.R.; et al. 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur. Heart J. 2017, 38, 2739–2786.
- Otto, C.M.; Nishimura, R.A.; Bonow, R.O.; Carabello, B.A.; Erwin, J.P.; Gentile, F.; Jneid, H.; Krieger, E.V.; Mack, M.; McLeod, C.; et al. 2020 ACC/AHA Guideline for the Management of Patients with Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2021, 143.
- Bhatia, N.; Basra, S.S.; Skolnick, A.H.; Wenger, N.K. Aortic valve disease in the older adult. J. Geriatr. Cardiol. 2016, 13, 941–944.
- Leon, M.B.; Smith, C.R.; Mack, M.; Miller, D.C.; Moses, J.W.; Svensson, L.G.; Tuzcu, E.M.; Webb, J.G.; Fontana, G.P.; Makkar, R.R.; et al. Transcatheter Aortic-Valve Implantation for Aortic Stenosis in Patients Who Cannot Undergo Surgery. N. Engl. J. Med. 2010, 363, 1597–1607.
- Leon, M.B.; Smith, C.R.; Mack, M.J.; Makkar, R.R.; Svensson, L.G.; Kodali, S.K.; Thourani, V.H.; Tuzcu, E.M.; Miller, D.C.; Herrmann, H.C.; et al. Transcatheter or Surgical Aortic-Valve Replacement in Intermediate-Risk Patients. N. Engl. J. Med. 2016, 374, 1609–1620.
- Armijo, G.; Nombela-Franco, L.; Tirado-Conte, G. Cerebrovascular Events after Transcatheter Aortic Valve Implantation. Front. Cardiovasc. Med. 2018, 5.
- Kappetein, A.P.; Head, S.J.; Généreux, P.; Piazza, N.; Van Mieghem, N.M.; Blackstone, E.H.; Brott, T.G.; Cohen, D.J.; Cutlip, D.E.; Van Es, G.A.; et al. Updated standardized endpoint definitions for transcatheter aortic valve implantation: The Valve Academic Research Consortium-2 consensus document. J. Thorac. Cardiovasc. Surg. 2013, 145, 6–23.
- Smith, C.R.; Leon, M.B.; Mack, M.J.; Miller, D.C.; Moses, J.W.; Svensson, L.G.; Tuzcu, E.M.; Webb, J.G.; Fontana, G.P.; Mak-kar, R.R.; et al. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N. Engl. J. Med. 2011, 364, 2187–2198.
- Mack, M.J.; Leon, M.B.; Thourani, V.H.; Makkar, R.; Kodali, S.K.; Russo, M.; Kapadia, S.R.; Malaisrie, S.C.; Cohen, D.J.; Pibarot, P.; et al. Transcatheter Aortic-Valve Replacement with a Balloon-Expandable Valve in Low-Risk Patients. N. Engl. J. Med. 2019, 380, 1695–1705.
- Eggebrecht, H.; Schmermund, A.; Voigtländer, T.; Kahlert, P.; Erbel, R.; Mehta, R.H. Risk of stroke after transcatheter aortic valve implantation (TAVI): A meta-analysis of 10,037 published patients. EuroIntervention 2012, 8, 129–138.
- Krasopoulos, G.; Falconieri, F.; Benedetto, U.; Newton, J.; Sayeed, R.; Kharbanda, R.; Banning, A. European real world trans-catheter aortic valve implantation: Systematic review and meta-analysis of European national registries. J. Cardiothorac. Surg. 2016, 11, 159.
- Muralidharan, A.; Thiagarajan, K.; Van Ham, R.; Gleason, T.G.; Mulukutla, S.; Schindler, J.T.; Jeevanantham, V.; Thirumala, P.D. Meta-Analysis of Perioperative Stroke and Mortality in Transcatheter Aortic Valve Implantation. Am. J. Cardiol. 2016, 118, 1031–1045.
- Holmes, D.R.; Nishimura, R.A.; Grover, F.L.; Brindis, R.G.; Carroll, J.D.; Edwards, F.H.; Peterson, E.D.; Rumsfeld, J.S.; Sha-hian, D.M.; Thourani, V.H.; et al. Annual Outcomes with Transcatheter Valve Therapy from the STS/ACC TVT Registry. J. Am. Coll. Cardiol. 2015, 66, 2813–2823.
- Woldendorp, K.; Indja, B.; Bannon, P.G.; Fanning, J.P.; Plunkett, B.T.; Grieve, S.M. Silent brain infarcts and early cognitive outcomes after transcatheter aortic valve implantation: A systematic review and meta-analysis. Eur. Heart J. 2021, 42, 1004–1015.
- Indja, B.; Woldendorp, K.; Vallely, M.P.; Grieve, S.M. Silent Brain Infarcts Following Cardiac Procedures: A Systematic Review and Meta-Analysis. J. Am. Heart Assoc. 2019, 8, e010920.
- Riley, K.J.; Kao, L.W.; Low, Y.H.; Card, S.; Manalo, G.; Fleming, J.P.; Essandoh, M.K.; Dalia, A.A.; Qu, J.Z. Neurologic Dysfunction and Neuroprotection in Transcatheter Aortic Valve Implantation. J. Cardiothorac. Vasc. Anesth. 2021.
- Van Mieghem, N.M.; Schipper, M.E.I.; Ladich, E.; Faqiri, E.; Van Der Boon, R.; Randjgari, A.; Schultz, C.; Moelker, A.; Van Geuns, R.J.; Otsuka, F.; et al. Histopathology of embolic debris captured during transcatheter aortic valve replacement. Circulation 2013, 127, 2194–2201.
- Davlouros, P.A.; Mplani, V.C.; Koniari, I.; Tsigkas, G.; Hahalis, G. Transcatheter aortic valve replacement and stroke: A comprehensive review. J. Geriatr. Cardiol. 2018, 15, 95–104.
- Grabert, S.; Lange, R.; Bleiziffer, S. Incidence and causes of silent and symptomatic stroke following surgical and transcatheter aortic valve replacement: A comprehensive review. Interact. Cardiovasc. Thorac. Surg. 2016, 23, 469–476.
- Nombela-Franco, L.; Webb, J.G.; De Jaegere, P.P.; Toggweiler, S.; Nuis, R.J.; Dager, A.E.; Amat-Santos, I.J.; Cheung, A.; Ye, J.; Binder, R.K.; et al. Timing, predictive factors, and prognostic value of cerebrovascular events in a large cohort of patients undergoing transcatheter aortic valve implantation. Circulation 2012, 126, 3041–3053.
- Chakravarty, T.; Søndergaard, L.; Friedman, J.; De Backer, O.; Berman, D.; Kofoed, K.F.; Jilaihawi, H.; Shiota, T.; Abramowitz, Y.; Jørgensen, T.H.; et al. Subclinical leaflet thrombosis in surgical and transcatheter bioprosthetic aortic valves: An observational study. Lancet 2017, 389, 2383–2392.
- Van Belle, E.; Hengstenberg, C.; Lefevre, T.; Kupatt, C.; Debry, N.; Husser, O.; Pontana, F.; Kuchcinski, G.; Deliargyris, E.N.; Mehran, R.; et al. Cerebral Embolism During Transcatheter Aortic Valve Replacement: The BRAVO-3 MRI Study. J. Am. Coll. Cardiol. 2016, 68, 589–599.
- Mokin, M.; Zivadinov, R.; Dwyer, M.G.; Lazar, R.M.; Hopkins, L.N.; Siddiqui, A.H. Transcatheter aortic valve replacement: Perioperative stroke and beyond. Expert. Rev. Neurother. 2017, 17, 327–334.
- Nkomo, V.T.; Gardin, J.M.; Skelton, T.N.; Gottdiener, J.S.; Scott, C.G.; Enriquez-Sarano, M. Burden of valvular heart diseases: A population-based study. Lancet 2006, 368, 1005–1011.
- Feldman, T.; Foster, E.; Glower, D.D.; Kar, S.; Rinaldi, M.J.; Fail, P.S.; Smalling, R.W.; Siegel, R.; Rose, G.A.; Engeron, E.; et al. Percutaneous Repair or Surgery for Mitral Regurgitation. N. Engl. J. Med. 2011, 364, 1395–1406.
- Iung, B.; Armoiry, X.; Vahanian, A.; Boutitie, F.; Mewton, N.; Trochu, J.N.; Lefèvre, T.; Messika-Zeitoun, D.; Guerin, P.; Cormier, B.; et al. Percutaneous repair or medical treatment for secondary mitral regurgitation: Outcomes at 2 years. Eur. J. Heart Fail. 2019, 21, 1619–1627.
- Stone, G.W.; Lindenfeld, J.; Abraham, W.T.; Kar, S.; Lim, D.S.; Mishell, J.M.; Whisenant, B.; Grayburn, P.A.; Rinaldi, M.; Ka-padia, S.R.; et al. Transcatheter Mitral-Valve Repair in Patients with Heart Failure. N. Engl. J. Med. 2018, 379, 2307–2318.
- Da Silva, P.B.; Sousa, J.P.; Oliveiros, B.; Donato, H.; Costa, M.; Gonçalves, L.; Teixeira, R. Stroke after transcatheter edge-to-edge mitral valve repair: A systematic review and meta-analysis. EuroIntervention 2020, 14, 1401–1408.
- Puls, M.; Lubos, E.; Boekstegers, P.; Von Bardeleben, R.S.; Ouarrak, T.; Butter, C.; Zuern, C.S.; Bekeredjian, R.; Sievert, H.; Nickenig, G.; et al. One-year outcomes and predictors of mortality after MitraClip therapy in contemporary clinical practice: Results from the German transcatheter mitral valve interventions registry. Eur. Heart J. 2016, 37, 703–712.
- Nickenig, G.; Estevez-Loureiro, R.; Franzen, O.; Tamburino, C.; Vanderheyden, M.; Lüscher, T.F.; Moat, N.; Price, S.; Dall’Ara, G.; Winter, R.; et al. Percutaneous mitral valve edge-to-edge Repair: In-hospital results and 1-year follow-up of 628 patients of the 2011–2012 pilot European Sentinel Registry. J. Am. Coll. Cardiol. 2014, 64, 875–884.
- Grasso, C.; Capodanno, D.; Scandura, S.; Cannata, S.; Immè, S.; Mangiafico, S.; Pistritto, A.; Ministeri, M.; Barbanti, M.; Caggegi, A.; et al. One- and twelve-month safety and efficacy outcomes of patients undergoing edge-to-edge percutaneous mitral valve repair (from the grasp registry). Am. J. Cardiol. 2013, 111, 1482–1487.
- Feldman, T.; Kar, S.; Elmariah, S.; Smart, S.C.; Trento, A.; Siegel, R.J.; Apruzzese, P.; Fail, P.; Rinaldi, M.J.; Smalling, R.W.; et al. Randomized Comparison of Percutaneous Repair and Surgery for Mitral Regurgitation 5-Year Results of EVEREST II. J. Am. Coll. Cardiol. 2015, 66, 2844–2854.
- Bekeredjian, R.; Mereles, D.; Pleger, S.; Krumsdorf, U.; Katus, H.A.; Rottbauer, W. Large atrial thrombus formation after MitraClipTM implantation: Is anticoagulation mandatory? J. Heart Valve Dis. 2011, 20, 146–148.
- Orban, M.; Braun, D.; Sonne, C.; Orban, M.; Thaler, R.; Grebmer, C.; Lesevic, H.; Schömig, A.; Mehilli, J.; Massberg, S.; et al. Dangerous liaison: Successful percutaneous edge-to-edge mitral valve repair in patients with end-stage systolic heart failure can cause left ventricular thrombus formation. EuroIntervention 2014, 10, 253–259.
- Blazek, S.; Lurz, P.; Mangner, N.; Fuernau, G.; Seeburger, J.; Luecke, C.; Gutberlet, M.; Ender, J.; Desch, S.; Eitel, I.; et al. Incidence, characteristics and functional implications of cerebral embolic lesions after the MitraClip procedure. EuroIntervention 2015, 10, 1195–1203.
- Frerker, C.; Schlüter, M.; Sanchez, O.D.; Reith, S.; Romero, M.E.; Ladich, E.; Schröder, J.; Schmidt, T.; Kreidel, F.; Joner, M.; et al. Cerebral Protection during MitraClip Implantation Initial Experience at 2 Centers. JACC Cardiovasc. Interv. 2016, 9, 171–179.
- Van Mieghem, N.M.; Van Gils, L. Cerebral Embolic Protection in Catheter-Based Mitral Interventions Research or Clinical Tool? JACC Cardiovasc. Interv. 2016, 9, 180–182.
- Maleki, K.; Mohammadi, R.; Hart, D.; Cotiga, D.; Farhat, N.; Steinberg, J.S. Intracardiac ultrasound detection of thrombus on transseptal sheath: Incidence, treatment, and prevention. J. Cardiovasc. Electrophysiol. 2005, 16, 561–565.
- Allan, R.W.; Alnuaimat, H.; Edwards, W.D.; Tazelaar, H.D. Embolization of hydrophilic catheter coating to the lungs: Report of a case mimicking granulomatous vasculitis. Am. J. Clin. Pathol. 2009, 132, 794–797.
- Babcock, D.E.; Hergenrother, R.W.; Craig, D.A.; Kolodgie, F.D.; Virmani, R. In vivo distribution of particulate matter from coated angioplasty balloon catheters. Biomaterials 2013, 34, 3196–3205.
- El-Najjar, V.; Robinson, M. Autopsy demonstration of intramyocardial polymer gel emboli associated with a giant-cell reaction following cardiac catheterization: A case report. Cardiovasc. Pathol. 2012, 21, 59–61.
- Braemswig, T.B.; Kusserow, M.M.D.; Kruppa, J.; Reinthaler, M.; Erdur, H.; Fritsch, M.; Curio, J.; Leistner, D.M.; Audebert, H.J.; Endres, M.; et al. Cerebral embolisation during transcatheter edge-to-edge repair of the mitral valve with the MitraClip system: A prospective, observational study. EuroIntervention 2021.
- Bapat, V.; Rajagopal, V.; Meduri, C.; Farivar, R.S.; Walton, A.; Duffy, S.J.; Gooley, R.; Almeida, A.; Reardon, M.J.; Kleiman, N.S.; et al. Early Experience with New Transcatheter Mitral Valve Replacement. J. Am. Coll. Cardiol. 2018, 71, 12–21.
- Webb, J.G.; Murdoch, D.J.; Boone, R.H.; Moss, R.; Attinger-Toller, A.; Blanke, P.; Cheung, A.; Hensey, M.; Leipsic, J.; Ong, K.; et al. Percutaneous Transcatheter Mitral Valve Replacement: First-in-Human Experience with a New Transseptal System. J. Am. Coll Cardiol. 2019, 73, 1239–1246.
- Muller, D.W.M.; Farivar, R.S.; Jansz, P.; Bae, R.; Walters, D.; Clarke, A.; Grayburn, P.A.; Stoler, R.C.; Dahle, G.; Rein, K.A.; et al. Transcatheter Mitral Valve Replacement for Patients with Symptomatic Mitral Regurgitation: A Global Feasibility Trial. J. Am. Coll. Cardiol. 2017, 69, 381–391.
- Goode, D.; Dhaliwal, R.; Mohammadi, H. Transcatheter Mitral Valve Replacement: State of the Art. Cardiovasc. Eng. Technol. 2020, 11, 229–253.
- Rodriguez, C.J.; Bartz, T.M.; Longstreth, W.T.; Kizer, J.R.; Barasch, E.; Lloyd-Jones, D.M.; Gottdiener, J.S. Association of annular calcification and aortic valve sclerosis with brain findings on magnetic resonance imaging in community dwelling older adults: The cardiovascular health study. J. Am. Coll. Cardiol. 2011, 57, 2172–2180.
- Benjamin, E.J.; Plehn, J.F.; D’Agostino, R.B.; Belanger, A.J.; Comai, K.; Fuller, D.L.; Wolf, P.A.; Levy, D. Mitral Annular Calcification and the Risk of Stroke in an Elderly Cohort. N. Engl. J. Med. 1992, 327, 374–379.
- Kahlert, P.; Knipp, S.C.; Schlamann, M.; Thielmann, M.; Al-Rashid, F.; Weber, M.; Johansson, U.; Wendt, D.; Jakob, H.G.; Forsting, M.; et al. Silent and apparent cerebral ischemia after percutaneous transfemoral aortic valve implantation: A diffusion-weighted magnetic resonance imaging study. Circulation 2010, 121, 870–878.
- Wessels, T.; Röttger, C.; Jauss, M.; Kaps, M.; Traupe, H.; Stol, E. Identification of embolic stroke patterns by diffusion-weighted MRI in clinically defined lacunar stroke syndromes. Stroke 2005, 36, 757–761.
- Van Mieghem, N.M.; El Faquir, N.; Rahhab, Z.; Rodríguez-Olivares, R.; Wilschut, J.; Ouhlous, M.; Galema, T.W.; Geleijnse, M.L.; Kappetein, A.P.; Schipper, M.E.I.; et al. Incidence and predictors of debris embolizing to the brain during transcatheter aortic valve implantation. JACC Cardiovasc. Interv. 2015, 8, 718–724.
- Benjamin, E.J.; Muntner, P.; Alonso, A.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Das, S.R.; et al. Heart Disease and Stroke Statistics-2019 Update: A Report from the American Heart Association. Circulation 2019, 139, e56–e528.
- Hindricks, G.; Potpara, T.; Dagres, N.; Arbelo, E.; Bax, J.J.; Blomström-Lundqvist, C.; Boriani, G.; Castella, M.; Dan, G.A.; Dilaveris, P.E.; et al. 2020 ESC Guidelines for the diagnosis andmanagement of atrial fibrillation developed incollaboration with the European Association ofCardio-Thoracic Surgery (EACTS). Eur. Heart J. 2021, 42, 373–498.
- Madhavan, M.; Graff-Radford, J.; Piccini, J.P.; Gersh, B.J. Cognitive dysfunction in atrial fibrillation. Nat. Rev. Cardiol. 2018, 15, 744–756.
- Blackshear, J.L.; Odell, J.A. Appendage obliteration to reduce stroke in cardiac surgical patients with atrial fibrillation. Ann. Thorac. Surg. 1996, 61, 755–759.
- Lip, G.Y.H.; Collet, J.P.; Caterina, R.; De Fauchier, L.; Lane, D.A.; Larsen, T.B.; Marin, F.; Morais, J.; Narasimhan, C.; Ol-shansky, B.; et al. Antithrombotic therapy in atrial fibrillation associated with valvular heart disease: A joint consensus document from the European Heart Rhythm Association (EHRA) and European Society of Cardiology Working Group on Thrombosis, endorsed by the ESC Working. Europace 2017, 19, 1757–1758.
- Di Biase, L.; Santangeli, P.; Anselmino, M.; Mohanty, P.; Salvetti, I.; Gili, S.; Horton, R.; Sanchez, J.E.; Bai, R.; Mohanty, S.; et al. Does the left atrial appendage morphology correlate with the risk of stroke in patients with atrial fibrillation? Results from a multicenter study. J. Am. Coll. Cardiol. 2012, 60, 531–538.
- Naydenov, S.; Runev, N.; Manov, E. Are three weeks of oral anticoagulation sufficient for safe cardioversion in atrial fibrillation? Medicina 2021, 57, 554.
- Macle, L.; Cairns, J.; Leblanc, K.; Tsang, T.; Skanes, A.; Cox, J.L.; Healey, J.S.; Bell, A.; Pilote, L.; Andrade, J.G.; et al. 2016 Focused Update of the Canadian Cardiovascular Society Guidelines for the Management of Atrial Fibrillation. Can. J. Cardiol. 2016, 32, 1170–1185.
- Giugliano, R.P.; Ruff, C.T.; Braunwald, E.; Murphy, S.A.; Wiviott, S.D.; Halperin, J.L.; Waldo, A.L.; Ezekowitz, M.D.; Weitz, J.I.; Špinar, J.; et al. Edoxaban versus warfarin in patients with atrial fibrillation. N. Engl. J. Med. 2013, 369, 2093–2104.
- Granger, C.B.; Alexander, J.H.; McMurray, J.J.V.; Lopes, R.D.; Hylek, E.M.; Hanna, M.; Al-Khalidi, H.R.; Ansell, J.; Atar, D.; Avezum, A.; et al. Apixaban versus warfarin in patients with atrial fibrillation. N. Engl. J. Med. 2011, 365, 981–992.
- Patel, M.R.; Mahaffey, K.W.; Garg, J.; Pan, G.; Singer, D.E.; Hacke, W.; Breithardt, G.; Halperin, J.L.; Hankey, G.J.; Piccini, J.P.; et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N. Engl. J. Med. 2011, 365, 883–891.
- Connolly, S.J.; Ezekowitz, M.D.; Yusuf, S.; Eikelboom, J.; Oldgren, J.; Parekh, A.; Pogue, J.; Reilly, P.A.; Themeles, E.; Varrone, J.; et al. Dabigatran versus warfarin in patients with atrial fibrillation. N. Engl. J. Med. 2009, 361, 1139–1151.
- Schellinger, P.D.; Tsivgoulis, G.; Steiner, T.; Köhrmann, M. Percutaneous Left Atrial Appendage Occlusion for the Prevention of Stroke in Patients with Atrial Fibrillation: Review and Critical Appraisal. J. Stroke 2018, 20, 281–291.
- Safavi-Naeini, P.; Rasekh, A. Closure of Left Atrial Appendage to Prevent Stroke: Devices and Status. Tex. Heart Inst. J. 2018, 45, 172–174.
- Holmes, D.R.J.; Kar, S.; Price, M.J.; Whisenant, B.; Sievert, H.; Doshi, S.K.; Huber, K.; Reddy, V.Y. Prospective randomized evaluation of the Watchman Left Atrial Appendage Closure device in patients with atrial fibrillation versus long-term warfarin therapy: The PREVAIL trial. J. Am. Coll. Cardiol. 2014, 64, 1–12.
- Landmesser, U.; Tondo, C.; Camm, J.; Diener, H.C.; Paul, V.; Schmidt, B.; Settergren, M.; Teiger, E.; Nielsen-Kudsk, J.E.; Hildick-Smith, D. Left atrial appendage occlusion with the AMPLATZER Amulet device: One-year follow-up from the prospective global Amulet observational registry. EuroIntervention J. Eur. Collab. Work. Group Interv. Cardiol. Eur. Soc. Cardiol. 2018, 14, e590–e597.
- Thakkar, J.; Vasdeki, D.; Tzikas, A.; Meier, B.; Saw, J. Incidence, Prevention, and Management of Periprocedural Complications of Left Atrial Appendage Occlusion. Interv. Cardiol. Clin. 2018, 7, 243–252.
- Reddy, V.Y.; Doshi, S.K.; Sievert, H.; Buchbinder, M.; Neuzil, P.; Huber, K.; Halperin, J.L.; Holmes, D. Percutaneous left atrial appendage closure for stroke prophylaxis in patients with atrial fibrillation: 2.3-Year Follow-up of the PROTECT AF (Watchman Left Atrial Appendage System for Embolic Protection in Patients with Atrial Fibrillation) Trial. Circulation 2013, 127, 720–729.
- Reddy, V.Y.; Gibson, D.N.; Kar, S.; O’Neill, W.; Doshi, S.K.; Horton, R.P.; Buchbinder, M.; Gordon, N.T.; Holmes, D.R. Post-Approval, U.S. Experience with Left Atrial Appendage Closure for Stroke Prevention in Atrial Fibrillation. J. Am. Coll. Cardiol. 2017, 69, 253–261.
- Reddy, V.Y.; Holmes, D.; Doshi, S.K.; Neuzil, P.; Kar, S. Safety of percutaneous left atrial appendage closure: Results from the Watchman Left Atrial Appendage System for Embolic Protection in Patients with AF (PROTECT AF) clinical trial and the Continued Access Registry. Circulation 2011, 123, 417–424.
- Holmes, D.R.; Reddy, V.Y.; Turi, Z.G.; Doshi, S.K.; Sievert, H.; Buchbinder, M.; Mullin, C.M.; Sick, P. Percutaneous closure of the left atrial appendage versus warfarin therapy for prevention of stroke in patients with atrial fibrillation: A randomised non-inferiority trial. Lancet (Lond. Engl.) 2009, 374, 534–542.
- Majunke, N.; Eplinius, F.; Gutberlet, M.; Moebius-Winkler, S.; Daehnert, I.; Grothoff, M.; Schürer, S.; Mangner, N.; Lurz, P.; Erbs, S.; et al. Frequency and clinical course of cerebral embolism in patients undergoing transcatheter left atrial appendage closure. EuroIntervention J. Eur. Collab. Work. Group Interv. Cardiol. Eur. Soc. Cardiol. 2017, 13, 124–130.
- Boersma, L.V.A.; Schmidt, B.; Betts, T.R.; Sievert, H.; Tamburino, C.; Teiger, E.; Pokushalov, E.; Kische, S.; Schmitz, T.; Stein, K.M.; et al. Implant success and safety of left atrial appendage closure with the WATCHMAN device: Peri-procedural outcomes from the EWOLUTION registry. Eur. Heart J. 2016, 37, 2465–2474.
- Hildick-Smith, D.; Landmesser, U.; Camm, A.J.; Diener, H.C.; Paul, V.; Schmidt, B.; Settergren, M.; Teiger, E.; Nielsen-Kudsk, J.E.; Tondo, C. Left atrial appendage occlusion with the AmplatzerTM AmuletTM device: Full results of the prospective global observational study. Eur. Heart J. 2020, 41, 2894–2901.
- Laible, M.; Möhlenbruch, M.; Horstmann, S.; Pfaff, J.; Geis, N.A.; Pleger, S.; Schüler, S.; Rizos, T.; Bendszus, M.; Veltkamp, R. Peri-procedural silent cerebral infarcts after left atrial appendage occlusion. Eur. J. Neurol. 2017, 24, 53–57.
- Lakkireddy, D.; Afzal, M.R.; Lee, R.J.; Nagaraj, H.; Tschopp, D.; Gidney, B.; Ellis, C.; Altman, E.; Lee, B.; Kar, S.; et al. Short and long-term outcomes of percutaneous left atrial appendage suture ligation: Results from a US multicenter evaluation. Heart Rhythm. 2016, 13, 1030–1036.
- Bartus, K.; Han, F.T.; Bednarek, J.; Myc, J.; Kapelak, B.; Sadowski, J.; Lelakowski, J.; Bartus, S.; Yakubov, S.J.; Lee, R.J. Percutaneous left atrial appendage suture ligation using the LARIAT device in patients with atrial fibrillation: Initial clinical experience. J. Am. Coll. Cardiol. 2013, 62, 108–118.
- Price, M.J.; Gibson, D.N.; Yakubov, S.J.; Schultz, J.C.; Di Biase, L.; Natale, A.; Burkhardt, J.D.; Pershad, A.; Byrne, T.J.; Gid-ney, B.; et al. Early safety and efficacy of percutaneous left atrial appendage suture ligation: Results from the U.S. transcatheter LAA ligation consortium. J. Am. Coll. Cardiol. 2014, 64, 565–572.




