Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Alexander Zimmerer | + 1236 word(s) | 1236 | 2021-10-12 05:09:23 | | | |
| 2 | Jason Zhu | -1 word(s) | 1235 | 2021-10-14 04:19:02 | | | | |
| 3 | Jason Zhu | -68 word(s) | 1167 | 2021-10-28 11:41:23 | | | | |
| 4 | Jason Zhu | + 3 word(s) | 1170 | 2021-10-29 11:48:17 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Zimmerer, A. Activity after Total Hip Arthroplasty. Encyclopedia. Available online: https://encyclopedia.pub/entry/15007 (accessed on 07 February 2026).
Zimmerer A. Activity after Total Hip Arthroplasty. Encyclopedia. Available at: https://encyclopedia.pub/entry/15007. Accessed February 07, 2026.
Zimmerer, Alexander. "Activity after Total Hip Arthroplasty" Encyclopedia, https://encyclopedia.pub/entry/15007 (accessed February 07, 2026).
Zimmerer, A. (2021, October 13). Activity after Total Hip Arthroplasty. In Encyclopedia. https://encyclopedia.pub/entry/15007
Zimmerer, Alexander. "Activity after Total Hip Arthroplasty." Encyclopedia. Web. 13 October, 2021.
Copy Citation
A large proportion of patients under 40 years of age who underwent Total Hip Arthroplasty (THA) increased their physical activity. Eighty-six percent of the patients were highly active, with a UCLA score ≥ 7. Furthermore, the reported MCID, SCB, and PASS for mHHS were achieved by more than 80% of patients
sports activity
young patients
THA
MCID
PASS
SCB
1. Background
The management of degenerative hip diseases in young patients remains a challenge. Current conditions, such as femoroacetabular impingement syndrome (FAIS), developmental dysplasia of the hip (DDH), and trauma are extensively recognized as sources of pain and functional limitations in active individuals that precede the development of hip osteoarthritis [1][2][3][4][5][6][7]. In the past several years, there has been a rapid increase in the development of surgical techniques to preserve native hip joints, with the appreciation that most hip problems in young adults are associated with altered hip morphology [1][8]. Despite the improvement of both open and arthroscopic hip-preservation procedures, these procedures may not provide adequate symptom relief in the case of severe osteoarthritic changes, and total hip arthroplasty (THA) may be required [8][9][10]. These cases are often especially challenging due to deformity, muscle wasting, and scarring from previous surgeries [11][12]. THA offers young patients the opportunity to achieve excellent pain relief levels and enhanced function. However, young patients undergoing THA often have high expectations concerning their postoperative level of activity [10][13][14]. A systematic review on the functional outcomes after THA among patients under 30 years has been conducted [10]. However, there is a lack of data answering questions about functional outcomes and sports activity levels after THA in young patients.
2. Demographics
Thirty-six patients (40 hips) were included in the analysis. The mean age was 31.5 ± 5 (19–39) years, the mean body index (BMI) was 27.1 ± 5.3 (17.3–43.8) kg/m2, the mean duration of surgery was 73.5 ± 25.5 (45–141) minutes, the mean duration of the symptoms prior to surgery was 4.8 ± 4.4 (0.5–23) years, and the mean follow-up was 3.9 ± 1.3 (2–9.5) years. Surgery was performed on 23 men and 13 women. The diagnoses leading to arthroplasty were secondary osteoarthrosis due to FAIS in 6 hips, DDH in 19 hips, trauma in 10 hips, and avascular necrosis of the femoral head (AVN) in 5 hips. Twenty THAs were performed on the right side, and twenty were performed on the left side (Table 1).
Table 1. Patient demographic data.
| Value | |
|---|---|
| Total no. of patients | 36 |
| Laterality, n (%) | |
| Right | 20 (50%) |
| Left | 20 (50%) |
| Sex, n (%) | |
| Female | 13 (36%) |
| Male | 23 (64%) |
| Age, years | 31.5 ± 5 (19–39) |
| Body mass index, kg/m2 | 27.1 ± 5.3 (17.3–43.8) |
| Follow-up, years | 3.9 ± 1.3 (2–9.5) |
| Preoperative-diagnoses, n (%) | |
| FAIS | 6 (15%) |
| DDH | 19 (47.5%) |
| Trauma | 10 (25%) |
| Avascular necrosis of the femoral head | 5 (12.5%) |
At the latest follow-up, there was no revision surgery. However, two patients presented a leg length difference of 1 cm.
3. Sports and Recreational Activity
Complete questionnaire data regarding recreational activity were available for 36 patients. After surgery, 33 of 36 patients (92%) were active in at least one recreational activity, compared to 16 of 36 (44%) before the onset of first symptoms. Most of the patients who were inactive started new sports and recreational activities postoperatively. Patients engaged in an average of four different sport disciplines at the last follow-up, which differed significantly from the number of sport disciplines practiced before the onset of the first symptoms (1.8 disciplines; p < 0.0001). This increase was confirmed in the individual analyses of men and women. In the comparison between men and women within the groups, there was no difference in the practiced sports disciplines before onset of the first symptoms and after THA (prior: 2.1 to 1.4; p = 0.103; after: 4.3 to 3.7; p = 0.525) (Figure 2).
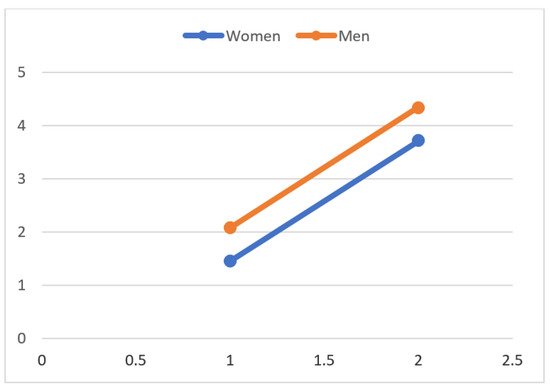
Figure 2. The number of sport disciplines practiced before onset of the first symptoms and after cementless THA. Women increased from 1.4 to 3.7 (p < 0.0001), and men increased from 2.1 to 4.4 practiced disciplines (p < 0.0001). The values are shown as mean values.
Sixty-seven percent of the patients initiated sports and recreational activities within three months after surgery, 17% between 3 and 6 months after surgery, and 17% six months after surgery. Overall, there was a significant increase in the types of sports performed (Table 2 and Table 3). These activities are consistent with the Hip Society member’s consensus guidelines and the American Association of Hip and Knee Surgeons, who have determined which sports are listed as low-, middle-, or high-impact activities, and do not manifest patient goals and expectations [15].
Table 2. Sports disciplines before onset of the first symptoms and after THA.
| Discipline | Prior to THA, n (%) | After THA, n (%) | p-Value |
|---|---|---|---|
| Long Walks | 8 (22.2%) | 27 (75%) | <0.0001 |
| Biking | 12 (33.3%) | 29 (80.6%) | <0.0001 |
| Hiking | 5 (13.9%) | 21 (58.3%) | <0.0001 |
| Nordic-Walking | 1 (2.8%) | 6 (16.7%) | 0.063 |
| Fitness Training | 6 (16.7%) | 23 (63.9%) | <0.0001 |
| Alpine skiing | 4 (11.1%) | 6 (16.7%) | 0.500 |
| Jogging | 2 (5.6%) | 8 (22.2%) | 0.031 |
| Soccer | 2 (5.6%) | 2 (5.6%) | 0.500 |
| Handball | 2 (5.6%) | 2 (5.6%) | 0.500 |
| Volleyball | 1 (2.8%) | 3 (8.3%) | 0.250 |
| Golf | 1 (2.8%) | 1 (2.8%) | 0.500 |
Table 3. Sports disciplines before onset of the first symptoms and after THA.
| Discipline | Women | Men | ||||
|---|---|---|---|---|---|---|
| Prior to THA, n (%) | After THA, n (%) | p-Value | Prior to THA, n (%) | After THA, n (%) | p-Value | |
| Long Walks | 3 (8.3%) | 12 (33.3%) | 0.004 | 5 (13.9%) | 15 (41.7%) | 0.002 |
| Biking | 4 (11.1%) | 11 (30.6%) | 0.016 | 8 (22.2%) | 18 (50%) | 0.002 |
| Hiking | 1 (2.8%) | 5 (13.9%) | 0.125 | 4 (11.1%) | 16 (44.4%) | <0.0001 |
| Nordic-Walking | 0 | 3 (8.3%) | 0.250 | 1 (2.8%) | 3 (8.3%) | 0.500 |
| Fitness Training | 0 | 10 (27.8%) | 0.002 | 6 (16.7%) | 13 (36.11%) | 0.016 |
| Alpine skiing | 0 | 0 | 1.000 | 4 (11.1%) | 6 (16.67%) | 0.500 |
| Jogging | 1 (2.8%) | 2 (5.6%) | 1.000 | 1 (2.8%) | 6 (16.67%) | 0.063 |
| Soccer | 0 | 0 | 1.000 | 0 | 2 (5.6%) | 0.500 |
| Handball | 1 (2.8%) | 1 (2.8%) | 1.000 | 1 (2.8%) | 1 (2.8%) | 0.500 |
| Volleyball | 0 | 1 (2.8%) | 1.000 | 1 (2.8%) | 2 (5.6%) | 0.500 |
| Golf | 0 | 0 | 1.000 | 1 (2.8%) | 1 (2.8%) | 0.500 |
4. Return to Sports
The frequency (sports sessions per week) increased significantly from the level before the onset of the first symptoms to the last follow-up: patients were active one day per week before the onset of the first symptoms and three times per week after THA (p < 0.0001). In the analysis of the subgroups, male and female patients participated in sports at the same frequency (three times per week) as the last follow-up (p = 0.869) (Figure 3).
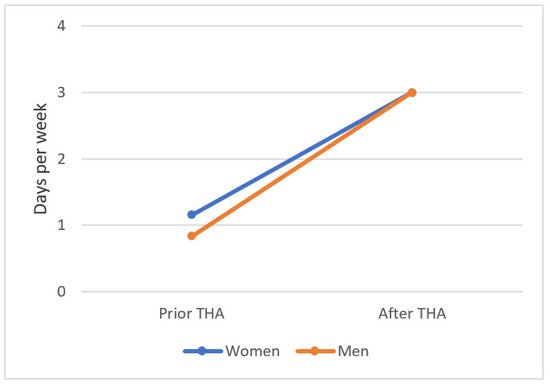
Figure 3. The number of sports sessions per week before onset of the first symptoms and after cementless THA. Women increased from 1 to 3 (p = 0.002), and men increased from 0.8 to 3 days per week (p < 0.0001). The values are shown as the mean values.
The minimum session length per week increased from 23 ± 31.6 (0–120) minutes before onset of the first symptoms to 82 ± 40.8 (0–150) min at the last follow-up (p < 0.0001). Before onset of the first symptoms, women exercised 18.4 ± 33.1 min, and men exercised 25.4 ± 31.2 min per session. Postoperatively, there was a significant increase in the number of minutes per session practiced; women exercised 85.4 ± 34.3 min, and men exercised 80.2 ± 47.3 min (p < 0.0001). There was no postoperative significant difference in session length per week between male and female patients (p = 0.716) (Figure 4).
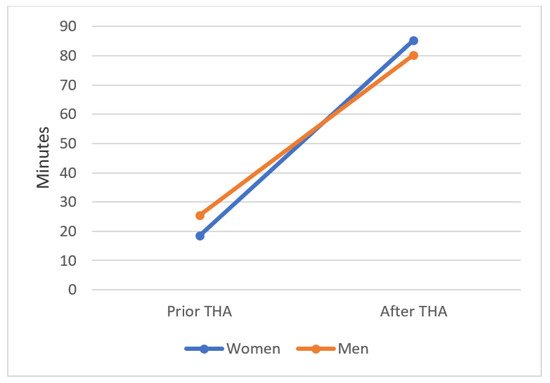
Figure 4. Session length per week of each sport before onset of the first symptoms and after cementless THA. Women increased from 18.4 to 85.4 min, and men increased from 25.4 to 80.2 min. The session length increased significantly. Values are shown as the mean values. p < 0.0001.
Eighty-five percent of the patients reported an enhancement in sports and recreational activity due to THA.
2.4. Outcome Scores
Paired t-test analysis of preoperative and postoperative reported outcomes demonstrated statistically significant improvements in mHHS (34.1 ± 18.6 vs. 92.6 ± 12.3; p < 0.0001), UCLA (3.2 ± 1.9 vs. 7.6 ± 1.5; p < 0.0001), and VAS (8 ± 1.7 vs. 1 ± 1.7; p < 0.0001) scores. Postoperatively, 31 patients (86%) reported a UCLA score ≥7, corresponding to being highly active in sport activities (Table 4).
Table 4. Pre- and postoperative patient-reported outcomes.
| Score | Preoperative | Postoperative | p-Value |
|---|---|---|---|
| mHHS | 34.1 ± 18.6 (3.3–81.4) | 92.6 ± 12.3 (41.8–100) | <0.0001 |
| UCLA | 3.2 ± 1.9 (1–8) | 7.6 ± 1.5 (3–10) | <0.0001 |
| VAS | 8 ± 1.7 (3–10) | 1 ± 1.7 (0–7) | <0.0001 |
5. Achievement of MCID, SCB, and PASS
The MCID threshold scores of mHHS was 20. Postoperatively, a total of 32 patients (89%) achieved MCID for the mHHS. The SCB threshold scores of mHHS was 52.8. Postoperatively, a total of 21 patients (58%) achieved SCB for the mHHS. The PASS threshold scores were 85. Postoperatively, a total of 28 patients (78%) achieved PASS for the mHHS.
6. Conclusions
A large number of patients 40 years or younger who underwent THA returned to sports, and their sporting ability increased significantly. Eighty-six percent of the patients were highly active with a UCLA score ≥7. Furthermore, the reported MCID, SCB, and PASS for mHHS were achieved by more than 80% of our patients.
References
- Beck, M.; Kalhor, M.; Leunig, M.; Ganz, R. Hip morphology influences the pattern of damage to the acetabular cartilage: Femoroacetabular impingement as a cause of early osteoarthritis of the hip. J. Bone Joint Surg. Br. 2005, 87, 1012–1018.
- Aigner, T.; Rose, J.; Martin, J.; Buckwalter, J. Aging Theories of Primary Osteoarthritis: From Epidemiology to Molecular Biology. Rejuvenation Res. 2004, 7, 134–145.
- Bullough, P.G. The geometry of diarthrodial joints, its physiologic maintenance, and the possible significance of age-related changes in geometry-to-load distribution and the development of osteoarthritis. Clin. Orthop. Relat. Res. 1981, 156, 61–66.
- Ganz, R.; Leunig, M.; Leunig-Ganz, K.; Harris, W.H. The etiology of osteoarthritis of the hip: An integrated mechanical concept. Clin. Orthop. Relat. Res. 2008, 466, 264–272.
- Parvizi, J.; Leunig, M.; Ganz, R. Femoroacetabular Impingement. J. Am. Acad. Orthop. Surg. 2007, 15, 561–570.
- Steppacher, S.D.; Tannast, M.; Ganz, R.; Siebenrock, K.A. Mean 20-year Followup of Bernese Periacetabular Osteotomy. Clin. Orthop. Relat. Res. 2008, 466, 1633–1644.
- Zgoda, M.; Paczek, L.; Bartłomiejczyk, I.; Siemińska, J.; Chmielewski, D.; Górecki, A. Age-related decrease in the activity of collagenase in the femoral head in patients with hip osteoarthritis. Clin. Rheumatol. 2007, 26, 240–241.
- Peters, C.L. Mild to Moderate Hip OA: Joint Preservation or Total Hip Arthroplasty? J. Arthroplast. 2015, 30, 1109–1112.
- Eskelinen, A.; Remes, V.; Helenius, I.; Pulkkinen, P.; Nevalainen, J.; Paavolainen, P. Uncemented total hip arthroplasty for primary osteoarthritis in young patients: A mid-to long-term follow-up study from the Finnish Arthroplasty Register. Acta Orthop. 2006, 77, 57–70.
- Walker, R.P.; Gee, M.; Wong, F.; Shah, Z.; George, M.; Bankes, M.J.; Ajuied, A. Functional Outcomes of Total Hip Arthroplasty in Patients Aged 30 Years or Less: A Systematic Review and Meta-Analysis. HIP Int. 2016, 26, 424–431.
- Clohisy, J.C.; Beaulé, P.E.; O’malley, A.; Safran, M.R.; Schoenecker, P. Hip Disease in the Young Adult: Current Concepts of Etiology and Surgical Treatment. J. Bone Jt. Surg.-Am. Vol. 2008, 90, 2267–2281.
- Polkowski, G.G.; Callaghan, J.J.; Mont, M.A.; Clohisy, J.C. Total Hip Arthroplasty in the Very Young Patient. J. Am. Acad. Orthop. Surg. 2012, 20, 487–497.
- Mardani-Kivi, M.; Karimi-Mobarakeh, M.; Asadi, K.; Hashemi-Motlagh, K.; Saheb-Ekhtiari, K. Evaluation of clinical outcomes of cementless total hip arthroplasty in patients under 30 years of age. Eur. J. Orthop. Surg. Traumatol. 2012, 23, 785–790.
- Clohisy, J.C.; Oryhon, J.M.; Seyler, T.M.; Wells, C.W.; Liu, S.S.; Callaghan, J.J.; Mont, M.A. Function and Fixation of Total Hip Arthroplasty in Patients 25 Years of Age or Younger. Clin. Orthop. Relat. Res. 2010, 468, 3207–3213.
- Klein, G.R.; Levine, B.R.; Hozack, W.J.; Strauss, E.J.; D’Antonio, J.A.; Macaulay, W.; Di Cesare, P.E. Return to athletic activity after total hip arthroplasty. Consensus guidelines based on a survey of the Hip Society and American Association of Hip and Knee Surgeons. J. Arthroplast. 2007, 22, 171–175.
More
Information
Subjects:
Allergy; Health Care Sciences & Services
Contributor
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
936
Revisions:
4 times
(View History)
Update Date:
23 Nov 2021
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




