
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Saptarshi Bhattacharya | + 1570 word(s) | 1570 | 2021-06-10 06:21:09 | | | |
| 2 | Lindsay Dong | -70 word(s) | 1500 | 2021-07-23 05:39:40 | | | | |
| 3 | Lindsay Dong | -70 word(s) | 1500 | 2021-07-23 05:43:10 | | | | |
| 4 | Saptarshi Bhattacharya | Meta information modification | 1500 | 2021-07-24 03:16:44 | | |
Video Upload Options
Hepatocrinology is defined as the bidirectional, complex relationship between hepatic and endocrine physiology and dysfunctions. The scope of hepatocrinology includes conditions of varied etiology (metabolic, infectious, autoimmune, and invasive) that we term as hepato-endocrine syndromes.
1. Introduction
The subject ‘hepatocrinology’ is the field of medicine that studies the bidirectional relationship between hepatic and endocrine physiology, as well as dysfunction. The hepato-insular axis is a part of hepatocrine physiology [1]. Endocrine manifestations of liver insufficiency (cirrhosis) and malignancy, and hepatic complications of various endocrine disorders are included. The possible hepatotropic effect of endocrine drugs, pleiotropic endocrine consequences of medicines used in the management of liver disease, and potential exaptation of endocrine agents for use in hepatology form part of this science.
2. The Liver as an Endocrine Organ
The liver secretes various hormones, which mediate glucose metabolism, blood pressure, growth, and hemorheological homeostasis. These include insulin-like growth factor (IGF)-1, betatrophin, and irisin, all of which mediate insulin sensitivity [2][3]. Angiotensinogen, produced by the liver, is the bedrock of the renin-angiotensin-aldosterone system, which contributes to blood pressure maintenance [4]. Hepcidin and thrombopoietin contribute to the regulation of iron metabolism and platelet production, respectively [5][6]. The hepato-insular axis is a well-researched contributor to glucose metabolism and has been described variously as the entero-insular or adipo-hepato-insular axis [1]. There are several other hormones or their precursors that are synthesized by the liver. Some of the important products are summarized in Table 1 and detailed below.
| Action | Hormones | Reference |
|---|---|---|
| Hormone synthesis | IGF-1 | Bach [2] |
| Angiotensinogen | Matsuaska [4] | |
| Thrombopoietin | Hitchcock [6] | |
| Hepcidin | Ruchala [5] | |
| Betatrophin | Raghow [3] | |
| Proprotein convertase subtilsin-kexin type 9 | Yadav [7] | |
| Hormone action modulation | IGF binding protein 1 to 6 | Allard [8] |
| Sex hormone-binding globulin | Selby [9] | |
| Thyroid hormone-binding globulin | Schussler [10] | |
| Transthyretin | Palha [11] | |
| Corticosteroid binding globulin | Breuner [12] | |
| Vitamin D binding protein | Bouillon [13] |
3. Sexual Dimorphism in Liver Disorders
Many liver diseases show differential gender distribution. NAFLD is more common in men during the reproductive age group, but is more frequent in women after menopause, indicating a possible protective role of estrogen [14]. HCC occurs more commonly in men, while the risk of autoimmune liver diseases such as primary biliary cirrhosis and autoimmune hepatitis is more common in women [15]. Apart from sex hormones, differences in xenobiotics, immune function, genetic alterations, and receptor expression are presumed to drive the dichotomy [16].
4. Endocrine Manifestations of Hepatic Disease
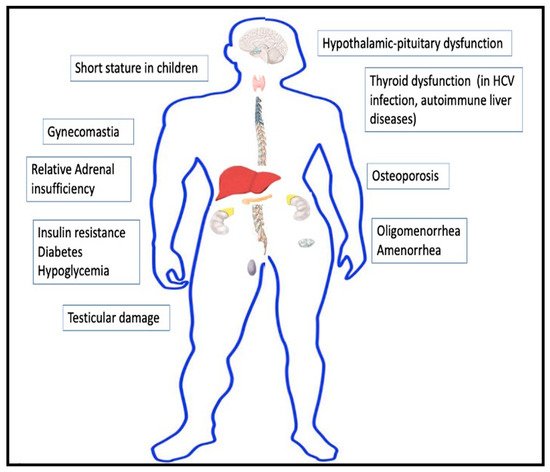
The liver modulates the functioning of the endocrine system directly or indirectly in multiple ways. Liver dysfunction is thus predictably associated with various endocrine disorders. The significant anomalies have been detailed below and depicted in Figure 1.
5. Hepatic Manifestations of Endocrine Disease
Endocrine and metabolic diseases are a common cause of hepatic dysfunction. The common endocrine causes of liver dysfunction have been depicted in Table 2. NAFLD resulting from metabolic disorders such as diabetes, obesity, and dyslipidemia has emerged as one of the leading causes of chronic liver disease over the past two decades. Several other hormonal disturbances affect the functioning of the liver directly or indirectly.
| Hepatic Manifestation | Endocrine Disorders | References |
|---|---|---|
| Non-alcoholic fatty liver disease | Insulin resistance, diabetes, obesity, and dyslipidemia | Watt [17] |
| Hepatic steatosis or steato-hepatitis | Cushing’s syndrome, acromegaly, Graves’ disease and other causes of thyrotoxicosis, polycystic ovary syndrome, male hypogonadism, and pheochromocytoma | Lonardo [18] |
| Hepatic metastasis | Adrenal cancer, pancreatic cancer, ovarian and testicular neoplasm, and malignant pheochromocytoma | Ridder [19] |
| Neonatal cholestasis | Congenital combined pituitary hormone deficiency, congenital hypothyroidism, and HNF1B-MODY (previously MODY-5) | Chan [20], Korkmaz [21] |
| Acute hepatic congestion (with jaundice) | Myxedema coma | Villalba [22] |
| Cholestasis | Thyrotoxicosis | Abebe [23] |
| Congestive hepatomegaly | Thyrotoxic heart failure | Piantanida [24] |
| Mauriac syndrome | Poorly controlled diabetes mellitus | Subedi [25] |
6. Sexual Dimorphism in Liver Disorders
Many liver diseases show differential gender distribution. NAFLD is more common in men during the reproductive age group, but is more frequent in women after menopause, indicating a possible protective role of estrogen [14]. HCC occurs more commonly in men, while the risk of autoimmune liver diseases such as primary biliary cirrhosis and autoimmune hepatitis is more common in women [15]. Women also show higher vulnerability to alcohol-related liver diseases [26]. Apart from sex hormones, differences in xenobiotics, immune function, genetic alterations, and receptor expression are presumed to drive the dichotomy [16].
7. Liver Function Biochemical Markers as Predictors of Endocrine Dysfunction
In several studies, liver enzymes have correlated with the development of incident diabetes [27]. γ-glutamyltransferase (GGT) has been proposed as a marker of oxidative stress and is associated with the future risk of diabetes. GGT levels have also been considered an indicator of hepatic fat deposition, which is related to insulin resistance [28]. In several reports, GGT and alanine aminotransferase in early pregnancy predicted the future occurrence of gestational diabetes mellitus [29][30]. Table 3 summarizes the liver enzymes which have been linked to the future development of metabolic disorders.
| Abnormality in Liver Function | Significance | References |
|---|---|---|
| Raised GGT | Probable role in the prediction of future risk of diabetes | Kaneko [27] |
| Elevated ALT | Probable role in the prediction of future risk of diabetes | Kaneko [27] |
| Elevated ALT and GGT in early pregnancy | Correlates with development of gestational diabetes mellitus | Lee [29], Zhao [30] |
| Elevated liver enzymes | Possible marker of insulin resistance and metabolic syndrome | Marchesini [31] |
8. Hepato-Endocrine Syndromes
We have used the term “hepato-endocrine syndromes” to describe disorders with a common etiology that manifest as combined hepatic and endocrine dysfunction. The various hepato-endocrine syndromes are enumerated in Table 4. Disorders of iron and copper metabolism such as hemochromatosis and Wilson’s disease are notable examples of this syndrome [32][33]. Polyglandular autoimmune syndromes type 1 and type 2 can develop autoimmune hepatitis and primary biliary cirrhosis, respectively, as their hepatic manifestations [34]. Hepatitis C virus infection can be associated with thyroiditis and hypothyroidism [35].
| Disease | Hepatic Manifestation | Endocrine Dysfunctions |
| Metabolic disorders | ||
| Hemochromatosis [32] | Hepatic fibrosis, cirrhosis, and hepatocellular carcinoma | Diabetes, hypopituitarism, secondary hypogonadism, and secondary hypothyroidism |
| Wilson’s disease [33] | Transaminitis, steatosis, acute hepatitis and acute liver failure (with an associated Coombs-negative hemolytic anemia), chronic hepatitis, and cirrhosis | Fanconi syndrome, distal renal tubular acidosis, nephrolithiasis, gigantism, hypoparathyroidism, pancreatitis, impotence, infertility, and repeated spontaneous abortions |
| Glycogen storage disorders: Glycogen storage disease I (von Gierke disease)—90% of cases [36] |
Glucose-6-phosphatase deficiency in liver and muscle, hepatomegaly, and hepatic adenomas | Hypoglycemia, lactic acidosis, hypertriglyceridemia, and hyperuricemia; short stature, and delayed puberty |
| Autoimmune disorders | ||
| Polyglandular autoimmune syndrome 1 [34] | Autoimmune hepatitis | Hypoparathyroidism and autoimmune adrenal insufficiency (along with chronic mucocutaneous candidiasis) |
| Polyglandular autoimmune syndrome 2 [34] | Primary biliary cirrhosis | Addison’s disease plus either an autoimmune thyroid disease or type 1 diabetes mellitus associated with hypogonadism, and other endocrinopathies |
| Infections | ||
| Hepatitis C infection [35] | Chronic hepatitis C, cirrhosis, and hepatocellular carcinoma | Thyroid autoimmunity, hypothyroidism, and higher prevalence of thyroid cancer |
| Hepatitis B infection [37] | Chronic hepatitis B, cirrhosis, and hepatocellular carcinoma | Increased risk of diabetes mellitus |
| Malignancy | ||
| Paraneoplastic endocrine syndromes [38] | Hepatocellular carcinoma | Hypoglycemia, hypercholesterolemia, and hypercalcemia |
9. Hepatic Effect of Endocrine Drugs
The endocrine drugs can have harmful as well as beneficial effects on the liver. Both anabolic steroids and estrogens can cause cholestasis, hepatic adenoma, focal nodular hyperplasia, and other hepatic disorders [39][40]. Acute liver failure has been reported with diverse agents such as propylthiouracil (used for hyperthyroidism) and high doses of methylprednisolone [41][42]. Orlistat, a commonly used therapy for weight loss, has also been described to cause subacute and acute liver failure [43].
10. Endocrine Effects of Drugs Used in Hepatology
Spironolactone, commonly used for the management of ascites in patients with cirrhosis, is an anti-androgen which has beneficial effects in PCOS in women, but causes painful gynecomastia in males [44][45]. Interferon-alpha used for management of hepatitis C infection can result in thyroid dysfunction [46]. Beta-blockers have often been associated with erectile dysfunction [47]. Table 5 depicts the common drug interactions in hepatocrinology.
| Hepatic Effects of Endocrine Drugs | |
| Drugs | Adverse Effects |
| Anabolic androgenic steroid [39] | Hepatic adenoma, hepatocellular carcinoma, cholestasis, and peliosis hepatis. |
| Estrogen/oral contraceptive pills [40] | Intrahepatic canalicular cholestasis, hepatic adenomas, focal nodular hyperplasia, hemangioma or hamartoma, peliosis hepatis, and Budd Chiari syndrome |
| Tamoxifen [48] | NAFLD |
| Propylthiouracil, methimazole, carbimazole [41] | Hepatitis, cholestasis, and acute liver failure |
| Corticosteroids [42] | Hepatic enlargement, steatosis, glycogenosis. NAFLD, exacerbate chronic viral hepatitis, and high doses of intravenous methylprednisolone—acute liver failure (sometimes fatal) |
| Vasopressin receptor antagonist [49] | Transaminitis and acute liver failure |
| Orlistat [43] | Cholelithiasis, cholestatic hepatitis, and acute and subacute liver failure |
| Drugs | Beneficial effects |
| Pioglitazone [50] | Beneficial effect on NAFLD |
| GLP-1RA [50] | Possible beneficial effect on NAFLD |
| SGLT-2 inhibitors [50] | Possible beneficial effect on NAFLD |
| Saroglitazar [50] | Possible beneficial effect on NAFLD |
| Corticosteroids [51] | Treatment of autoimmune hepatitis and prevention of rejection of liver transplant |
| Somatostatin analogs (octreotide and others) [52] | Treatment of variceal bleeding (decreases portal blood flow) |
| Vasopressin analogs (terlipressin) [52] | Treatment of variceal bleeding (decreases portal blood flow) |
| Endocrine Effects of Drugs Used in Hepatology | |
| Drugs | Adverse effects |
| Spironolactone [45] | Gynaecomastia, and hypogonadism in men |
| Beta-blockers [47] | Erectile dysfunction |
| Interferon-alpha [46] | Hypothyroidism, autoimmune (Hashimoto’s) thyroiditis, destructive thyroiditis, and Graves’ disease |
| Drugs | Beneficial effects |
| Ursodeoxycholic acid [53] | Possible beneficial effect in metabolic syndrome |
| Spironolactone [44] | Treatment of PCOS |
References
- Wewer Albrechtsen, N.J.; Pedersen, J.; Galsgaard, K.D.; Winther-Sørensen, M.; Suppli, M.P.; Janah, L.; Gromada, J.; Vilstrup, H.; Knop, F.K.; Holst, J.J. The Liver-α-Cell Axis and Type 2 Diabetes. Endocr. Rev. 2019, 40, 1353–1366.
- Bach, L.A. IGF-binding proteins. J. Mol. Endocrinol. 2018, 61, T11–T28.
- Raghow, R. Betatrophin: A liver-derived hormone for the pancreatic β-cell proliferation. World J. Diabetes 2013, 4, 234–237.
- Matsusaka, T.; Niimura, F.; Shimizu, A.; Pastan, I.; Saito, A.; Kobori, H.; Nishiyama, A.; Ichikawa, I. Liver Angiotensinogen Is the Primary Source of Renal Angiotensin II. J. Am. Soc. Nephrol. 2012, 23, 1181–1189.
- Ruchala, P.; Nemeth, E. The pathophysiology and pharmacology of hepcidin. Trends Pharmacol. Sci. 2014, 35, 155–161.
- Hitchcock, I.S.; Kaushansky, K. Thrombopoietin from beginning to end. Br. J. Haematol. 2014, 165, 259–268.
- Yadav, K.; Sharma, M.; Ferdinand, K. Proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors: Present perspectives and future horizons. Nutr. Metab. Cardiovasc. Dis. 2016, 26, 853–862.
- Allard, J.B.; Duan, C. IGF-Binding Proteins: Why Do They Exist and Why Are There So Many? Front. Endocrinol. 2018, 9, 117.
- Selby, C. Sex Hormone Binding Globulin: Origin, Function and Clinical Significance. Ann. Clin. Biochem. Int. J. Lab. Med. 1990, 27, 532–541.
- Schussler, G.C. The Thyroxine-Binding Proteins. Thyroid 2000, 10, 141–149.
- Palha, J.A. Transthyretin as a Thyroid Hormone Carrier: Function Revisited. Clin. Chem. Lab. Med. 2002, 40, 1292–1300.
- Breuner, C.W.; Beyl, H.E.; Malisch, J.L. Corticosteroid-binding globulins: Lessons from biomedical research. Mol. Cell. Endocrinol. 2020, 514, 110857.
- Bouillon, R.; Schuit, F.; Antonio, L.; Rastinejad, F. Vitamin D Binding Protein: A Historic Overview. Front. Endocrinol. 2020, 10, 910.
- Lonardo, A.; Nascimbeni, F.; Ballestri, S.; Fairweather, D.; Win, S.; Than, T.A.; Abdelmalek, M.F.; Suzuki, A. Sex Differences in Nonalcoholic Fatty Liver Disease: State of the Art and Identification of Research Gaps. Hepatology 2019, 70, 1457–1469.
- Kur, P.; Kolasa-Wołosiuk, A.; Misiakiewicz-Has, K.; Wiszniewska, B. Sex Hormone-Dependent Physiology and Diseases of Liver. Int. J. Environ. Res. Public Health 2020, 17, 2620.
- Biswas, S.; Ghose, S. Divergent impact of gender in advancement of liver injuries, diseases, and carcinogenesis. Front. Biosci. Sch. Ed. 2018, 10, 65–100.
- Watt, M.J.; Miotto, P.M.; De Nardo, W.; Montgomery, M. The Liver as an Endocrine Organ—Linking NAFLD and Insulin Resistance. Endocr. Rev. 2019, 40, 1367–1393.
- Lonardo, A.; Mantovani, A.; Lugari, S.; Targher, G. NAFLD in Some Common Endocrine Diseases: Prevalence, Pathophysiology, and Principles of Diagnosis and Management. Int. J. Mol. Sci. 2019, 20, 2841.
- de Ridder, J.; de Wilt, J.H.W.; Simmer, F.; Overbeek, L.; Lemmens, V.; Nagtegaal, I. Incidence and origin of histologically confirmed liver metastases: An explorative case-study of 23,154 patients. Oncotarget 2016, 7, 55368–55376.
- Chan, U.; Chan, W.-T.; Ting, W.-H.; Ho, C.-S.; Liu, H.-C.; Lee, H.-C. Cholestasis caused by panhypopituitarism and acquired cytomegalovirus infection in a 2-month-old male infant: A case report. Medicine 2017, 96, e6757.
- Korkmaz, L.; Akın, M.A.; Güneş, T.; Daar, G.; Baştuğ, O.; Yıkılmaz, A.; Kurtoğlu, S. Unusual Course of Congenital Hypothyroidism and Route of the L-Thyroxine Treatment in a Preterm Newborn. J. Clin. Res. Pediatric Endocrinol. 2014, 6, 177–179.
- Villalba, N.L.; Zulfiqar, A.-A.; Saint-Mezard, V.; Alonso, M.B.; Kechida, M.; Zamorano, N.F.; Ortega, S.S. Myxedema coma: Four patients diagnosed at the Internal Medicine Department of the Dr. Negrin University Hospital in Spain. Pan Afr. Med. J. 2019, 34, 7.
- Abebe, A.; Eck, L.M.; Holyoak, M. Severe cholestatic jaundice associated with Graves’ disease. Clin. Case Rep. 2018, 6, 2240–2245.
- Piantanida, E.; Ippolito, S.; Gallo, D.; Masiello, E.; Premoli, P.; Cusini, C.; Rosetti, S.; Sabatino, J.; Segato, S.; Trimarchi, F.; et al. The interplay between thyroid and liver: Implications for clinical practice. J. Endocrinol. Investig. 2020, 43, 885–899.
- Subedi, A.; Kumar, V.C.S.; Sharma, A.; Hoilat, G.; John, S. Persistent lactic acidosis in the Mauriac syndrome in type 1 diabetes mellitus. Bayl. Univ. Med Cent. Proc. 2021, 34, 382–383.
- Agabio, R.; Pisanu, C.; Gessa, G.L.; Franconi, F. Sex Differences in Alcohol Use Disorder. Curr. Med. Chem. 2017, 24, 2661–2670.
- Kaneko, K.; Yatsuya, H.; Li, Y.; Uemura, M.; Chiang, C.; Hirakawa, Y.; Ota, A.; Tamakoshi, K.; Aoyama, A. Association of gamma-glutamyl transferase and alanine aminotransferase with type 2 diabetes mellitus incidence in middle-aged Japanese men: 12-year follow up. J. Diabetes Investig. 2018, 10, 837–845.
- Koenig, G.; Seneff, S. Gamma-Glutamyltransferase: A Predictive Biomarker of Cellular Antioxidant Inadequacy and Disease Risk. Dis. Markers 2015, 2015, 1–18.
- Lee, S.M.; Park, J.S.; Han, Y.J.; Kim, W.; Bang, S.H.; Kim, B.J.; Park, C.-W.; Kim, M.Y. Elevated Alanine Aminotransferase in Early Pregnancy and Subsequent Development of Gestational Diabetes and Preeclampsia. J. Korean Med Sci. 2020, 35, e198.
- Zhao, W.; Zhang, L.; Zhang, G.; Varkaneh, H.K.; Rahmani, J.; Clark, C.; Ryan, P.M.; Abdulazeem, H.; Salehisahlabadi, A. The association of plasma levels of liver enzymes and risk of gestational diabetes mellitus: A systematic review and dose–response meta-analysis of observational studies. Acta Diabetol. 2019, 57, 635–644.
- Marchesini, G.; Avagnina, S.; Barantani, E.G.; Ciccarone, A.M.; Corica, F.; Dall’Aglio, E.; Grave, R.D.; Morpurgo, P.S.; Tomasi, F.; Vitacolonna, E. Aminotransferase and gamma-glutamyltranspeptidase levels in obesity are associated with insulin resistance and the metabolic syndrome. J. Endocrinol. Investig. 2005, 28, 333–339.
- Crownover, B.K.; Covey, C.J. Hereditary hemochromatosis. Am. Fam. Physician 2013, 87, 183–190.
- Mulligan, C.; Bronstein, J.M. Wilson Disease: An Overview and Approach to Management. Neurol. Clin. 2020, 38, 417–432.
- Kahaly, G.J.; Frommer, L. Polyglandular autoimmune syndromes. J. Endocrinol. Investig. 2018, 41, 91–98.
- Tran, H.A.; Jones, T.L.; Ianna, E.A.; Foy, A.; Reeves, G.E.M. Thyroid disease in chronic hepatitis C infection treated with combination interferon-α and ribavirin: Management strategies and future perspective. Endocr. Pract. Off. J. Am. Coll. Endocrinol. Am. Assoc. Clin. Endocrinol. 2013, 19, 292–300.
- Ellingwood, S.S.; Cheng, A. Biochemical and clinical aspects of glycogen storage diseases. J. Endocrinol. 2018, 238, R131–R141.
- Hong, Y.S.; Chang, Y.; Ryu, S.; Cainzos-Achirica, M.; Kwon, M.-J.; Zhang, Y.; Choi, Y.; Ahn, J.; Rampal, S.; Zhao, D.; et al. Hepatitis B and C virus infection and diabetes mellitus: A cohort study. Sci. Rep. 2017, 7, 1–7.
- Qu, Q.; Wang, S.; Chen, S.; Zhou, L.; Rui, J.-A. Prognostic role and significance of paraneoplastic syndromes in hepatocellular carcinoma. Am. Surg. 2014, 80, 191–196.
- Niedfeldt, M.W. Anabolic Steroid Effect on the Liver. Curr. Sports Med. Rep. 2018, 17, 97–102.
- Ponnatapura, J.; Kielar, A.; Burke, L.M.; Lockhart, M.E.; Abualruz, A.-R.; Tappouni, R.; Lalwani, N. Hepatic complications of oral contraceptive pills and estrogen on MRI: Controversies and update-Adenoma and beyond. Magn. Reson. Imaging 2019, 60, 110–121.
- Akmal, A.; Kung, J. Propylthiouracil, and methimazole, and carbimazole-related hepatotoxicity. Expert Opin. Drug Saf. 2014, 13, 1397–1406.
- Zoubek, M.E.; Pinazo-Bandera, J.; Ortega-Alonso, A.; Hernández, N.; Crespo, J.; Contreras, F.; Medina-Cáliz, I.; Sanabria-Cabrera, J.; Sanjuan-Jiménez, R.; González-Jiménez, A.; et al. Liver injury after methylprednisolone pulses: A disputable cause of hepatotoxicity. A case series and literature review. United Eur. Gastroenterol. J. 2019, 7, 825–837.
- Filippatos, T.D.; Derdemezis, C.S.; Gazi, I.F.; Nakou, E.S.; Mikhailidis, D.P.; Elisaf, M.S. Orlistat-associated adverse effects and drug interactions: A critical review. Drug Saf. 2008, 31, 53–65.
- Witchel, S.F.; Oberfield, S.E.; Peña, A.S. Polycystic Ovary Syndrome: Pathophysiology, Presentation, and Treatment with Emphasis on Adolescent Girls. J. Endocr. Soc. 2019, 3, 1545–1573.
- Lainscak, M.; Pelliccia, F.; Rosano, G.; Vitale, C.; Schiariti, M.S.M.; Greco, C.; Speziale, G.; Gaudio, C. Safety profile of mineralocorticoid receptor antagonists: Spironolactone and eplerenone. Int. J. Cardiol. 2015, 200, 25–29.
- Jadali, Z. Autoimmune thyroid disorders in hepatitis C virus infection: Effect of interferon therapy. Indian J. Endocrinol. Metab. 2013, 17, 69–75.
- Sharp, R.P.; Gales, B.J. Nebivolol versus other beta blockers in patients with hypertension and erectile dysfunction. Ther. Adv. Urol. 2017, 9, 59–63.
- Chang, H.-T.; Pan, H.-J.; Lee, C.-H. Prevention of Tamoxifen-related Nonalcoholic Fatty Liver Disease in Breast Cancer Patients. Clin. Breast Cancer 2018, 18, e677–e685.
- Wu, Y.; Beland, F.; Chen, S.; Liu, F.; Guo, L.; Fang, J.-L. Mechanisms of tolvaptan-induced toxicity in HepG2 cells. Biochem. Pharmacol. 2015, 95, 324–336.
- Sumida, Y.; Yoneda, M. Current and future pharmacological therapies for NAFLD/NASH. J. Gastroenterol. 2018, 53, 362–376.
- Terziroli Beretta-Piccoli, B.; Mieli-Vergani, G.; Vergani, D. Autoimmune hepatitis: Standard treatment and systematic review of alternative treatments. World J. Gastroenterol. 2017, 23, 6030–6048.
- Bunchorntavakul, C.; Reddy, K.R. Pharmacologic Management of Portal Hypertension. Clin. Liver Dis. 2019, 23, 713–736.
- Di Ciaula, A.; Wang, D.Q.-H.; Portincasa, P. Cholesterol cholelithiasis: Part of a systemic metabolic disease, prone to primary prevention. Expert Rev. Gastroenterol. Hepatol. 2019, 13, 157–171.





