
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Mark I. Johnson | + 1579 word(s) | 1579 | 2021-04-22 13:49:06 | | | |
| 2 | Lindsay Dong | Meta information modification | 1579 | 2021-04-23 11:47:51 | | | | |
| 3 | Lindsay Dong | Meta information modification | 1579 | 2021-04-23 11:50:15 | | | | |
| 4 | Lindsay Dong | -105 word(s) | 1474 | 2021-04-23 11:55:08 | | | | |
| 5 | Lindsay Dong | -105 word(s) | 1474 | 2021-04-23 11:55:44 | | |
Video Upload Options
Transcutaneous electrical nerve stimulation (TENS) refers to the use of a portable device that generates pulsed electrical currents that are delivered across the intact surface of the skin via conducting electrodes to stimulate peripheral nerves.
1. Introduction
Transcutaneous electrical nerve stimulation (TENS) is a technique whereby pulsed electrical currents are administered through the intact surface of the skin with the intention of alleviating pain, akin to ‘electrically rubbing pain away’(Figure 1). TENS is primarily used for symptomatic relief of a variety of types of pain irrespective of origin (i.e., nociceptive, neuropathic and nociplastic) or setting (i.e., inpatient, outpatient and palliative). TENS is also used to manage faecal and urinary incontinence, constipation, nausea and vomiting, xerostomia, peripheral ischaemia and Reynaud’s syndrome, dementia, stroke (neuromuscular condition and neglect), oedema, wound healing, tissue regeneration (e.g., nerve, soft tissue, skin, and bone), reduction of tissue necrosis, sleep, fatigue, depression, and coma (for review, see [1]).
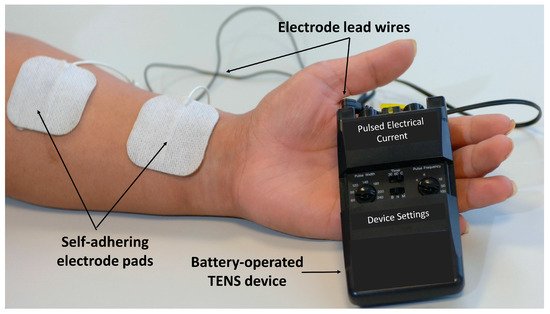
Figure 1. TENS equipment.
The safety profile of TENS compares favourably against medication. Adverse events associated with TENS are minor and include erythema and itchiness beneath or around the electrodes, and a vasovagal response in some individuals, manifesting as nausea and dizziness. Contraindications are few. When used to alleviate pain, TENS is usually administered to produce a strong comfortable sensation (electrical paraesthesiae) within, or close to, the site of pain (i.e., conventional TENS or sensory TENS, Figure 2). The sensory experience during TENS should be a pleasant ‘tingling’ or pleasant ‘pins and needles’ sensation and this should act to ‘soothe’ pain in a manner akin to ‘rubbing pain away’.
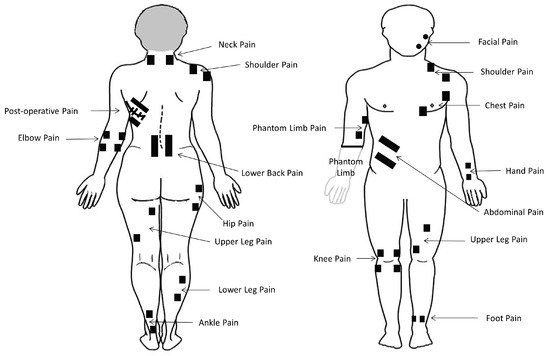
Figure 2. Common electrode positions for TENS. Black squares represent electrode pads.
Self-administering TENS empowers patients to take control of their pain management and removes the need for patients to be supervised or to have to travel to the clinic for treatment. TENS should be considered similar to heat therapies (e.g., hot packs and warm water bottles) or cold therapies (e.g., cold packs). (Figure 3).
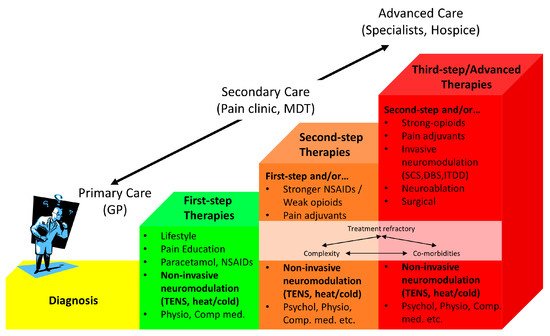
Figure 3. Stepped care model for pain treatment. Based on von Korff et al.[2]. Non-invasive neuromodulation techniques such as TENS are considered as adjuncts or as standalone treatment options at all steps of the care pathway. GP; General Practitioner: MDT; Multidisciplinary team: Psychol.; Psychology: Physio.; Physiotherapy: Comp. med.; Complementary medicine: NSAIDs; Non-Steroidal Anti-Inflammatory Drugs: SCS; Spinal Cord Stimulation: DBS; Deep Brain Stimulation: ITDD; Intrathecal Drug Delivery.
2. Principles and Practice of TENS
2.2. Physiological Principles of TENS
2.2.1. Electrical and Physiological Coupling
TENS is a technique-based intervention to selectively activate peripheral nerve fibres to elicit physiological neuromodulation. The electrical characteristics of currents produced by the TENS device influence which population of nerve fibres is activated (Figure 4). The amplitude of pulsed current is the critical characteristic to influence which axons are stimulated. For conventional TENS, the amplitude of current is titrated to stimulate low threshold large-diameter, non-nociceptive nerve fibres (e.g., mechanoreceptive A-beta fibres) without concurrent activation of higher threshold small-diameter nociceptive nerve fibres (A-delta and C fibres, Figure 5). The frequency (rate) of pulsed currents determines the rate of neuronal impulses and is limited by the absolute and relative refractory periods for the axon.
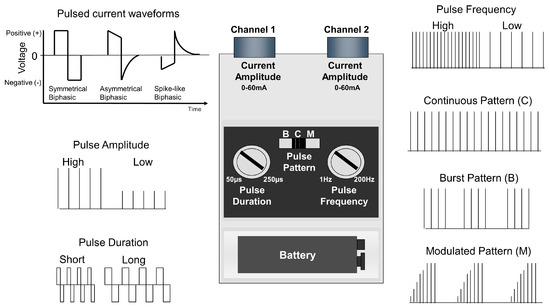
Figure 4. Output characteristics of a standard TENS device. Vertical lines represent a single pulse of current.
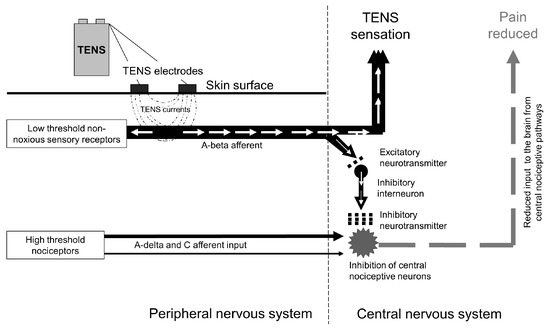
Figure 5. Selective activation of afferents using conventional TENS. The amplitude of currents is titrated to selectively activate low threshold nerve fibres (A-beta) generating nerve impulses (white arrows) that excite inhibitory interneurons in the central nervous system resulting in reductions in central nociceptive cell excitability and activity.
2.2.2. Physiological Mechanisms of Analgesic Action
TENS modulates nociceptive input at peripheral (‘peripheral impulse blockade’), segmental (‘spinal gating’) and extrasegmental (‘descending inhibition’) sites. Stimulation of low threshold large-diameter non-noxious cutaneous afferents reduces activity and excitability in sensitised or non-sensitised central nociceptive transmission cells, in segments of somatic receptive fields related to the location of the electrodes (Figure 5). Delivery of higher amplitude currents stimulates high threshold cutaneous (A-delta) afferents within deeper tissue and produces long-term depression of central nociceptor cell activity persisting up to 2 h post-stimulatio.
3. Long-Standing Uncertainty: Efficacy and Effectiveness
3.1. Context: TENS and Evidence-Based Medicine
Decisions to offer treatments to patients involves the integration of clinical experience and patient values, with the best available research information about efficacy and effectiveness. Clinical experience suggests that TENS may provide short-term relief of pain during or immediately after treatment for any type of acute or chronic pain. However, clinical experience alone cannot distinguish effects attributed to the active ingredient of a treatment from non-specific effects associated with the act of administering a treatment including patient expectation of a treatment having effects, natural fluctuations in symptoms, reporting bias to please the practitioner, and contamination from concurrent treatment.
3.2. Current Status of Evidence on the Clinical Efficacy of TENS
Guidelines from the Australian and New Zealand College of Anaesthetists and Faculty of Pain Medicine, recommend TENS for acute pain, including pain after thoracic surgery. The earliest systematic reviews on TENS for chronic pain were published in the late 1990s and were generally inconclusive [for review see [3]].
3.3. Everlasting Doubt about Efficacy and Effectiveness
It is shameful that the vast amount of research spanning nearly half a century has failed to resolve the issue of TENS efficacy, resulting in longstanding uncertainty about whether TENS should be offered to patients in public health systems or covered by private healthcare insurance (e.g., within the National Health Service in the U.K., or by the Center for Medicare Services in the USA, respectively). In fact, there have been long-standing unresolved debates about the analgesic efficacy of many non-pharmacological treatments including; complementary therapies (e.g., acupuncture), electrophysical agents (e.g., therapeutic ultrasound) and manual therapies (e.g., massage techniques). Hence, a critical appraisal of factors contributing to long-standing uncertainty about the efficacy of TENS will be generalizable to other non-pharmacological analgesic treatments.
4. Resolving the Impasse
To overcome the ‘efficacy-impasse’ there needs to be improvements in the quality of RCTs and a re-appraisal of approaches to systematic review. There are two solutions:
-
A large multicentered randomized controlled trial that enables participants to tailor TENS treatment according to their needs, including skills to optimise response and troubleshoot issues. Ideally, data should be gathered in a ‘real-world setting’ providing an ecologically valid insight to the value or otherwise of TENS in clinical practice. Enriched enrolment with randomized withdrawal studies are ideally suited for such needs.
-
A comprehensive meta-analysis that estimates the magnitude of during treatment effects irrespective of the type of pain, and includes an evaluation of precision, consistency and certainty of the effect size estimate based on study quality and risk of bias.
5. Being Unable to Determine Efficacy
NICE judged these findings to be insufficient evidence to support a recommendation to offer TENS for chronic primary pain, concluding that “Limited evidence for TENS showed no clinically important difference compared with sham TENS and usual care across several outcomes at less than 3 months, and no longer term evidence was identified.” [4]. This judgement appears to be based on long-term outcomes rather than in the moment relief of pain at rest or on movement. Thus, one high quality RCT with 100 participants per trial arm is not considered ‘sufficient’ evidence for NICE to recommend TENS, and it is unlikely that additional large RCTs will be produced in the near future.
Nowadays, electrodes are available that are woven into garments and interfaced with smart phone technology for more precise targeting of currents without the need to reposition electrodes. TENS usage data can be uploaded to the Cloud and machine learning software used to create personalized TENS treatment schedules. Analysis of large data sets of usage and outcomes from real-world settings may be a relatively cost-effective means of gathering ecologically valid data from new patients to resolve doubts about the utility and potential efficacy of TENS. Therefore, it is unlikely that uncertainty about efficacy will discourage patients from purchasing their own TENS equipment or discourage practitioners from indicating TENS in the future (Figure 6).
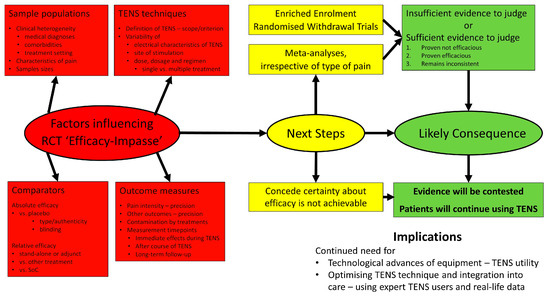
Figure 6. Summary of the factors contributing to the ‘efficacy-impasse’, next steps to resolve the impasse, and possible outcomes, consequences and implications going forward.
6. Summary
Inconsistent and imprecise effect size estimates found by RCTs result from the use of inadequate sample sizes, heterogeneous populations, muddled measurements of outcome, inappropriate TENS technique, dosage and regimen, and difficulties blinding placebo interventions. However, it may be necessary to concede that it is impossible to generate sufficient evidence about efficacy because operational challenges are insurmountable. This situation is not unique to TENS. There is longstanding uncertainty about analgesic efficacy for most nonpharmacological technique-based analgesic interventions including acupuncture, electrophysical agents (heat, cold, ultrasound, pulsed-shortwave, low-level laser) and a wide variety of manual therapies. Consequently, practice remains based on local policy and dogma. Perhaps clinicians, policy makers, funders and researchers need to reconsider the value of persisting with the production and publication of so many RCTs that fail to answer questions about efficacy.
References
- Johnson, M.I.. Transcutaneous Electrical Nerve Stimulation (TENS). Research to Support Clinical Practice; Johnson, MI, Eds.; Oxford University Press: Oxford, 2014; pp. 1-261.
- Von Korff, M.; Moore, J.C.; Stepped care for back pain: Activating approaches for primary care. Ann. Intern. Med 2001, 134, 911-917.
- Johnson, M.I.; Transcutaneous electrical nerve stimulation: Review of effectiveness. Nursing Standard 2014, 28, 44-53.
- National Institute for Health and Care Excellence. Chronic Pain (Primary and Secondary) in over 16s: Assessment of all Chronic Pain and Management of Chronic Primary Pain (NG193); National Institute for Health and Care Excellence (NICE): London, UK, 2021; pp. 1–36.




