
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Grazia Maugeri | + 1359 word(s) | 1359 | 2021-02-24 09:56:41 | | | |
| 2 | Lily Guo | Meta information modification | 1359 | 2021-02-25 05:29:23 | | | | |
| 3 | Lily Guo | Meta information modification | 1359 | 2021-03-10 10:14:31 | | |
Video Upload Options
The novel coronavirus disease 2019 (COVID-19) has been responsible for a global pandemic involving massive increases in the daily numbers of cases and deaths. Due to the emergency caused by the pandemic, huge efforts have been made to develop COVID-19 vaccines, the first of which were released in December 2020. Effective vaccines for COVID-19 are needed to protect the population, especially healthcare professionals and fragile individuals, such as older people or chronic-disease-affected patients. Physical exercise training generally has health benefits and assists in the prevention of several chronic diseases.
1. Introduction
The social effects caused by the global spread and pandemic of SARS-CoV-2 is having unimaginable consequences that the world has never faced in past decades. After the WHO declared SARS-CoV-2 a health emergency, the world responded quickly to “flatten the curve” or limit the spread of the virus by banning travel and closing non-essential businesses and educational institutions, as well stopping all kinds of large gatherings. In this first phase of the pandemic, around half of the world’s population was under full or partial lockdown to limit the spread of the deadly virus[1]. The unprecedented restrictions prompted by the raging SARS CoV-2 pandemic halted a wide variety of economic activities throughout the world. Day by day, the need for essential healthcare equipment increased in parallel with the increase of infected patients and death tolls. More than 100 countries closed their borders and worldwide air travel demand plummeted just after the announcement of the pandemic by the WHO. This severely impacted the world’s supply chain and international trade[2]. Economists agreed that there would be an enormous negative impact on global economic development due to COVID-19, which would possibly plunge the world economy into a deep recession [3]. Therefore, after this initial lockdown period, a second phase started, involving the partial reopening of the economy. However, increasing cases and limited numbers of intensive care beds have caused public health authorities in Europe to re-impose temporary lockdowns.
Global health authorities have been informed by epidemic and infectious disease specialists, who have faced the present health emergency by taking cues from past epidemics. However, we now know that the story of COVID-19 cannot be compared to past epidemics. Besides the high direct mortality for such a contagious acute disease, COVID-19 has placed extreme pressure on healthcare systems, altering access to health services of patients living with other pathologies, such as non-communicable diseases (NCDs). Moreover, such NCDs (e.g., diabetes mellitus, hypertension, cerebrovascular disease, coronary artery disease, chronic obstructive pulmonary disease) have been shown to predict poor prognosis in patients with COVID-19. SARS-CoV-2 and NCDs are clustering within social groups according to patterns of socioeconomic inequality that are deeply embedded in our societies. Limiting the harm caused by SARS-CoV-2 will demand that far greater attention is paid to NCDs and socioeconomic inequality than has previously been done. The aggregation of these diseases against a background of social and economic disparity aggravates the adverse effects of each separate disease. COVID-19 is not a pandemic or simple comorbidity—it is a syndemic[4]. Addressing COVID-19 means addressing hypertension, obesity, malnutrition, diabetes, cardiovascular and chronic respiratory diseases, cancer, and psychological and neurodegenerative disorders. Paying more attention to NCDs and socioeconomic inequality should be a strategic plan for both rich and poor nations in order to limit the harm caused by SARS-CoV-2.
The worldwide spread of SARS-CoV-2 infection has caused governments of various countries to take swift and unprecedented protective measures, including placing cities in lockdown and closing places where large gatherings would occur. Quarantine has radically changed the daily habits of the entire population, requiring people to practice “social distancing”. For example, in Italy, the Italian Ministry of Education (MIUR) decided to invest huge resources in special desks to promote higher interpersonal distance in classrooms to avoid the risk of infection[5]. Although such strategies have contained the COVID-19 outbreak, the prolonged self-isolation has deeply affected active lifestyles, leading healthy individuals and athletes to states of physical inactivity, with related consequences of hypomobility and inactivity-associated disorders, such as a reduction in maximal oxygen consumption (VO2max), endurance capacity, loss of muscle strength and mass, overweight, and decrease joint lubrification[6][7][8][9]. Just a few days of a sedentary lifestyle are sufficient to induce fiber denervation, insulin resistance, and low-grade systemic inflammation [10].
The positive effects of regular physical activity on general health are well known in the field of modern medicine. Physical activity counteracts cardiovascular vulnerability, inflammation, muscle atrophy, bone and cartilage loss or degeneration, and the reduction of aerobic capacity [11][12]. Physical exercise is also closely related to cognitive function and neurodegenerative disorders by inducing cellular and molecular processes underlying neurogenesis and synaptogenesis cascade, which enhance learning, memory, and brain plasticity[13][14]. These effects are extremely important, especially in light of new evidence showing brain damage among the consequences of COVID-19, including delirium, stroke, and brain inflammation. Moreover, adapted physical activity ameliorates one’s self-esteem and provides a sense of well-being by reducing the development of mental disorders[15]. In light of this evidence, the purpose of this narrative mini-review is to summarize the beneficial effects of the adapted physical activity performed before-, during-, and post-infection of COVID-19. To this end, four databases were used: PubMed, Scopus, Web of Science, and Google Scholar. The last search was conducted on 30 December 2020. The following keywords and combinations thereof were used: “exercise”, “physical activity”, “adapted physical activity”, “physical exercise”, “SARS-CoV-2”, “SARS CoV-2 pandemic”, “COVID-19 pandemic”. The initial study selection was performed via title and abstract screening. Duplicates were removed. The full texts of the selected articles were carefully read and analyzed in order to extract the appropriate data from each text.
2. Adapted Physical Activity Program during COVID-19 Infection
Considering the clinical characteristics of COVID-19, infected patients, who are compelled to rest in bed, are not able to perform normal activities of daily life or perform regular physical activity. Nevertheless, considering the multiple positive effects caused by exercise, adapted physical activity in all phases of recovery of patients (Figure 1) represents an important strategy to attenuate the decline in cognition function and to improve physical and psychological well-being in individuals affected by COVID-19. When treating patients—and given the intensive medical management involved for some COVID-19 patients, including prolonged protective lung ventilation, immobility, sedation, and treatment with neuromuscular blocking agents—in the acute phase it is possible to adopt only passive types of exercise performed by physiotherapists or kinesiologists, such as whole-body vibration (WBV) exercise and passive range-of-motion (pROM) exercises. In the post-acute phase, however, physiotherapists or kinesiologists can organize bed-based exercise programs (e.g., flexion and extension of the limbs and trunk) and assist patients to mobilize independently to stand-up and perform normal daily functions according to the Barthel index, such as washing, eating, and so on. Other adapted physical activities, comprising passive, active-assisted, active, or resisted joint range-of-motion exercises, are fundamental to restore and improve respiratory and cardiocirculatory functions, joint integrity, range-of-motion, muscle strength, and mental condition. During the day, hospitalized patients should perform the exercises alone by following a guided self-assessment for people with an acquired disability, which should be administered by physiotherapists or kinesiologists. This progressive approach as well as the known effects of general well-being can help keep patients busy and attenuate feelings of depression due to complete immobility. Regaining self-mobility can result in the patient acquiring better self-esteem and a strong response to depression.
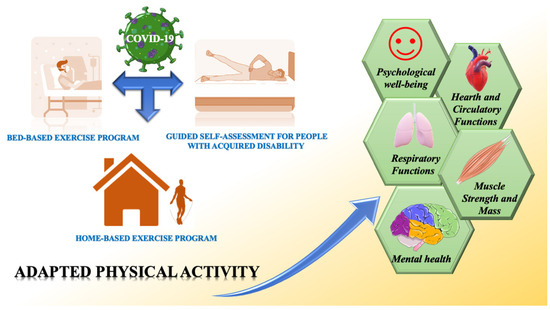
Figure 1. Health benefits from regular adapted physical activity in COVID-19-affected patients.
Pneumonia, a severe complication of the virus, has been shown to induce cognitive decline due to sustained hypoxia[16][17]. Moreover, pneumonia patients were found to possess high levels of pro-inflammatory cytokines, leading to neuroinflammation and neurodegeneration [40]. Therefore, the positive influence of physical activity on cognitive performance is fundamental to accelerate the subsequent full recovery of COVID-19 patients. In fact, different studies have demonstrated that physical exercise enhances the neuronal activity and hippocampal neurogenesis essential for cognition[18][19]. Furthermore, adapted physical activity for COVID-19 patients represents a key psychological support. Exercise stimulates the cholinergic, dopaminergic, and serotonergic systems, enhancing mood by reducing depression, anxiety, and panic attacks[6][20]. In light of these positive effects on mental and psychological health, adapted or tailor-made exercises in COVID-19-affected individuals should be considered.
References
- Koh, D. COVID-19 lockdowns throughout the world. Occup. Med. 2020, 70, kqaa073, doi:10.1093/occmed/kqaa073.
- Mishra, M.K. The World after COVID-19 and Its Impact on Global Economy. 2020. Available online: https://www.econstor.eu/handle/10419/215931 (accessed on 26 January 2021).
- Fernandes, N. Economic Effects of Coronavirus Outbreak (Covid-19) on the World Economy; SSRN: Rochester, NY, USA, 2020.
- Horton, R. Offline: COVID-19 is not a pandemic. Lancet 2020, 396, 874, doi:10.1016/S0140-6736(20)32000-6.
- Bergamin, M.; Musumeci, G. The utility of Anti-Covid-19 desks in Italy, doubts and criticism. J. Funct. Morphol. Kinesiol. 2021, 6, 2, doi:10.3390/jfmk6010002.
- Ravalli, S.; Musumeci, G. Coronavirus outbreak in Italy. Physiological benefits of home-based exercise during pandemic. J. Funct. Morphol. Kinesiol. 2020, 5, 31, doi:10.3390/jfmk5020031.
- Giustino, V.; Parroco, A.M.; Gennaro, A.; Musumeci, G.; Palma, A.; Battaglia, G. Physical activity levels and related energy expenditure during covid-19 quarantine among the sicilian active population: A cross-sectional online survey study. Sustainability 2020, 12, 4356, doi:10.3390/su12114356.
- Methnani, J.; Amor, D.; Yousfi, N.; Bouslama, A.; Omezzine, A.; Bouhlel, E. Sedentary behavior, exercise and COVID-19: Immune and metabolic implications in obesity and its comorbidities. J. Sports Med. Phys. Fit. 2020, doi:10.23736/S0022-4707.20.11898-X.
- Paoli, A.; Musumeci, G. Elite athletes and covid-19 lockdown: Future health concerns for an entire sector. J. Funct. Morphol. Kinesiol. 2020, 5, 30, doi:10.3390/jfmk5020030.
- Narici, M.; De Vito, G.; Franchi, M.; Paoli, A.; Moro, T.; Marcolin, G.; Grassi, B.; Baldassarre, G.; Zuccarelli, L.; Biolo, G.; et al. Impact of sedentarism due to the COVID-19 home confinement on neuromuscular, cardiovascular and metabolic health: Physiological and pathophysiological implications and recommendations for physical and nutritional countermeasures. Eur. J. Sport Sci. 2020, 12, 1–22, doi:10.1080/17461391.2020.1761076.
- Castrogiovanni, P.; Di Rosa, M.; Ravalli, S.; Castorina, A.; Guglielmino, C.; Imbesi, R.; Vecchio, M.; Drago, F.; Szychlinska, M.A.; Musumeci, G. Moderate physical activity as a prevention method for knee osteoarthritis and the role of synoviocytes as biological key. Int. J. Mol. Sci. 2019, 20, 511, doi:10.3390/ijms20030511.
- Szychlinska, M.A.; Castrogiovanni, P.; Trovato, F.M.; Nsir, H.; Zarrouk, M.; Lo Furno, D.; Di Rosa, M.; Imbesi, R.; Musumeci, G. Physical activity and Mediterranean diet based on olive tree phenolic compounds from two different geographical areas have protective effects on early osteoarthritis, muscle atrophy and hepatic steatosis. Eur. J. Nutr. 2019, 58, 565–581, doi:10.1007/s00394-018-1632-2.
- Maugeri, G.; D’agata, V. Effects of physical activity in amyotrophic lateral sclerosis. J. Funct. Morphol. Kinesiol. 2020, 5, 29, doi:10.3390/jfmk5020029.
- van Praag, H.; Christie, B.R.; Sejnowski, T.J.; Gage, F.H. Running enhances neurogenesis, learning, and long-term potentiation in mice. Proc. Natl. Acad. Sci. USA 1999, 96, 13427–13431, doi:10.1073/pnas.96.23.13427.
- van Minnen, A.; Hendriks, L.; Olff, M. When do trauma experts choose exposure therapy for PTSD patients? A controlled study of therapist and patient factors. Behav. Res. Ther. 2010, 48, 312–320.
- McCoy, J.G.; McKenna, J.T.; Connolly, N.P.; Poeta, D.L.; Ling, L.; McCarley, R.W.; Strecker, R.E. One week of exposure to intermittent hypoxia impairs attentional set-shifting in rats. Behav. Brain Res. 2010, 210, 123–126. 10.1016/j.bbr.2010.01.043.
- Nunnari, G.; Sanfilippo, C.; Castrogiovanni, P.; Imbesi, R.; Volti, G.L.; Barbagallo, I.; Musumeci, G.; Di Rosa, M. Network perturbation analysis in human bronchial epithelial cells following SARS-CoV2 infection. Exp. Cell Res. 2020, 395,112204, doi:10.1016/j.yexcr.2020.112204.
- Vivar, C.; Potter, M.C.; van Praag, H. All about running: Synaptic plasticity, growth factors and adult hippocampal neurogenesis. Curr. Top Behav. Neurosci. 2013, 15, 189–210.
- Ryan, S.M.; Nolan, Y.M. Neuroinflammation negatively affects adult hippocampal neurogenesis and cognition: Can exercise compensate? Neurosci. Biobehav. Rev. 2016, 61, 121–131, doi:10.1016/j.neubiorev.2015.12.004.
- Maugeri, G.; Castrogiovanni, P.; Battaglia, G.; Pippi, R.; D’Agata, V.; Palma, A.; Di Rosa, M.; Musumeci, G. The impact of physical activity on psychological health during Covid-19 pandemic in Italy. Heliyon 2020, 6, e04315, doi:10.1016/j.heliyon.2020.e04315.




