Personalized cognitive-behavioural therapy for obesity (CBT-OB) CBT-OB is an innovative treatment designed to help patients maintain long-term weight loss by addressing some limitations of traditional behavioural treatment of obesity (BT-OB), namely the poor personalization of the intervention and the prevalent focus on helping the patients to reach behavioural change (i.e., eating and exercise habits) rather than a cognitive change oriented to long-term weight control. As such, CBT-OB includes the main procedures of traditional BT-OB, but includes new strategies and procedures, introduced according to the individual patient’s needs, to address specific cognitive processes that previous research has found be associated with treatment discontinuation, weight loss and weight maintenance. Moreover, it can be delivered in a stepped-care approach, including three levels of care (i.e., outpatient, day-hospital, and residential) to treat patients with severe and disabling obesity.
1. Introduction
Personalized cognitive behavioural therapy for obesity (CBT-OB) is a new treatment designed to help patients with obesity to achieve and maintain a healthy weight loss through personalized combinations of strategies and procedures from traditional behavioural therapy for obesity (BT-OB) with others addressing some specific “cognitive processes” that the evidence suggests can influence attrition, weight loss and weight-loss maintenance. Personalized CBT-OB was devised by Dalle Grave and colleagues in Verona (Italy)[1][2], and it has been adapted to be delivered at outpatient, day-hospital and residential settings.
2. The Theory
The traditional treatments of obesity mainly aim to address the biological and behavioural factors hindering weight loss and maintenance, with very little attention to the cognitive processes that may be at play[3]. Failure to address a patients’ ability to adhere to lifestyle modification over time may therefore be one of the reasons why biological and behavioural treatments have limited effectiveness in promoting long-term weight loss[4]. Support to this theory comes by recent studies showing that there are several cognitive factors associated with treatment attrition, weight loss and weight maintenance (see Table 1).
Personalized CBT-OB has been designed with the aim to address some limitations of traditional behavioural treatment of obesity (BT-OB) namely the poor personalization of the intervention and the prevalent focus on helping the patients to reach behavioural change (i.e., eating and exercise habits) rather than a cognitive change oriented to long-term weight control.
|
Table 1. Cognitive factors associated with treatment discontinuation, amount of weight lost and weight-loss maintenance
Cognitive factors associated with treatment discontinuation:
- Higher expected 1-year BMI loss at baseline
- Primary goal for weight loss based on appearance at baseline
- Acceptable or disappointing weight with respect to personal expectations
- Dissatisfaction with weight loss obtained through treatment
Cognitive factors associated with amount of weight lost:
- Increase in dietary restraint and reduction in disinhibition
- Higher expected weight loss at baseline
Cognitive factors associated with weight-loss maintenance:
- Satisfaction with the results achieved
- Weight-loss satisfaction
- Confidence in the ability to lose additional weight without professional help
- Greater weight-loss satisfaction from week 15 or 19 of the weight-loss phase (a decline is associated with weight regain)
|
Goals, general strategies and procedures of personalized CBT-OB
The main goals of personalized CBT-OB are to help patients to (i) reach, accept and maintain a healthy amount of weight loss (i.e., 5–10% of their starting body weight); (ii) adopt and maintain a lifestyle conducive to weight control; and (iii) develop a stable “weight-control mind-set”.
CBT-OB therapists adopt, like other forms of CBT, a therapeutic style designed to develop and nurture a collaborative working relationship with the patients (collaborative empiricism). In addition to some of the procedures adopted by BT-OB (i.e., self-monitoring, goal setting, stimulus control, contingency management, behavioural substitution, skills for increasing social support, problem-solving and relapse prevention), CBT-OB includes specific cognitive strategies and procedures, some of which have been adapted from ‘enhanced’ CBT (CBT-E) for eating disorders[5] [5, 6] and Cooper et al. [7], and some have been developed ex novo. These integrations enable the treatment to be personalized, and help patients address the processes that our previous research has found to be respectively associated with drop-out, the amount of weight lost, and maintaining a lower weight in the long term (see Table 2).
Further details of personalized CBT-OB, together with a comprehensive description of the treatment and its implementation, can be found in the main treatment guide “Treating Obesity with Personalized Cognitive Behavioral Therapy”[6].
|
Table 2. CBT-OB strategies and procedures for reducing attrition, enhancing weight loss and improving weight-loss maintenance
Strategies and procedures for minimising attrition:
- Addressing patient’s difficulties attending the sessions
- Scheduling the sessions at times compatible with a patient’s work commitments
- Routinely asking the patients whether they are experiencing any difficulties as regards attending the sessions, and devoting time to understanding and/or overcoming them.
- Showing interest in each patient as a person, irrespective of their weight and/or other issues
- Adopting a “people first” policy—putting individuals before the disability or disease when describing persons affected by obesity (e.g., “person with obesity” instead of “obese person”
- Avoiding any use of potentially pejorative adjectives or adverbs, or any language that implies moral judgements or highlights patients’ “character flaws” regarding their weight
- Addressing unrealistic weight loss expectations
- Encouraging patients to pursue and be satisfied with achievable short-term weight-loss goals (i.e., a weight loss of between 0.5 kg and 1.0 kg/week) and not disputing unrealistic goals at the beginning of treatment
- Addressing unrealistic goals only when patients have achieved some success in reaching a healthy weight, but manifest dissatisfaction with the weight loss achieved
- Maintaining therapeutic momentum
- Identifying with the patients the best time to start the treatment
- Stressing the importance of avoiding any interruptions in treatment, especially during the first 8 weeks
- Explaining to the patients in advance that another therapist will take the place of the primary therapist in the event of their absence
- Developing a protocol for dealing with late attendance or non-attendance
- Encouraging patients to arrive a little early for session (e.g., 10–15 min) in order to relax and mentally prepare themselves
- If patients are running late for an appointment, calling them after 15 minutes to express concern about their absence, and to try to reschedule the appointment as soon as possible
Strategies and procedures for enhancing weight loss
- Increasing dietary restraint and decreasing dietary disinhibition
- Eating regularly (i.e., three planned meals and two snacks, and refraining from eating in the intervals between)
- Planning meals in advance (when, what and where to eat) on a specific monitoring record, making reference to a structured meal plan
- Supplying patients with grocery lists, menus and recipes
- Monitoring food intake in real-time
- Training patients to eat consciously (i.e., “think while you are eating”)
- Training patients to “ride out” the desire for food, educating them that any impulses will be transitory and can be tolerated
- Encouraging patients to consider their efforts to control eating as a necessary condition for achieving healthy weight loss and benefiting from its associated physical and psychological advantages
- Involving patients actively in identifying processes hindering weight loss using the “Weight-Loss Obstacles Questionnaire”
- Developing collaboratively with the patients their “Personal Formulation” of the processes that are hindering weight loss
- Designing personalized procedures aimed at addressing the specific obstacles encountered by each patient
- Involving, with the consent of patients, their significant others in treatment to create the optimal environment for facilitating patients attempts efforts to change their eating habits
Strategies and procedures for improving weight-loss maintenance
- Addressing weight-loss satisfaction before starting weight-loss maintenance
- Dedicating one or two sessions to preparing patients for weight maintenance, and collaboratively developing a weight-maintenance plan
- Encouraging patients to suspend any attempts to lose weight while learning weight-maintenance skills (i.e., at least 12 months)
- Creating a list of personal reasons to maintain weight
- Adopting a mindset with a constant focus on weight control, and keeping a constant but flexible focus on weight control and self-awareness regarding diet and physical activity
- Identifying and addressing high-risk weight- regain situations, preventing lapses from becoming relapses, and addressing any weight regain
- Implementing weekly self-weighing and ensuring patients maintain weight within a specific range of 4 kg
- Encouraging patients to follow a high-protein, low-glycaemic-index diet with moderate fat content, and to practice at least 30 minutes of moderate-intensity activity daily
|
3. The Versions of CBT-OB
CBT-OB has been designed to treat all classes of obesity within a stepped-care approach involving three levels of care (outpatient, day-hospital and residential). Outpatient CBT-OB can be delivered individually by a single therapist or in group by two therapists. It includes the following phases (see Figure 1):
- Preparatory Phase. This is delivered in one or two sessions, and has the aims of assessing the nature and severity of a patient’s obesity, as well as any associated medical and psychosocial comorbidities, as well as engaging the patient(s) in the treatment.
- Phase 1. This has been designed to help patients achieve a healthy rate of weight loss and be satisfied with the resulting weight. It lasts about 24 weeks and is delivered across 16 sessions, the first eight of which are held once a week, and the remaining eight on a two-weekly basis.
- Phase 2. This has the aim of helping patients to develop a lifestyle and mindset conducive to long-term weight maintenance. It usually lasts 48 weeks and is delivered across 12 sessions that are held at four-weekly intervals.
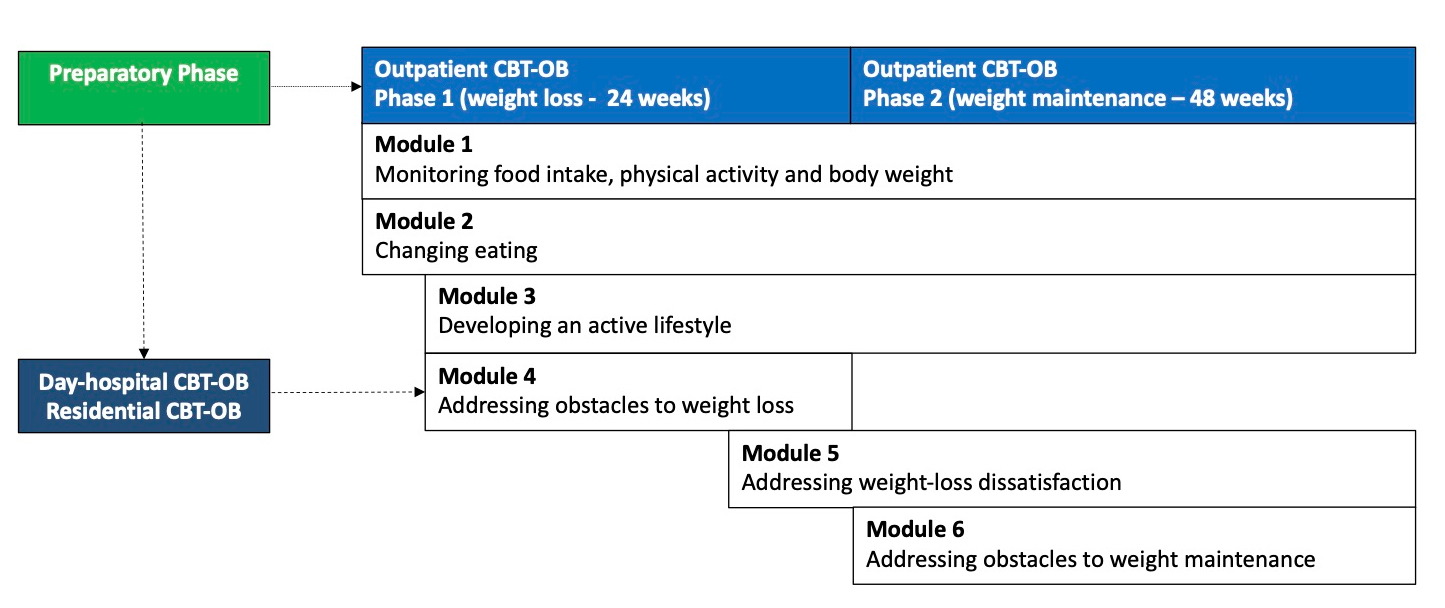
Figure 1. The map of personalised cognitive behavioural therapy for obesity (CBT-OB)
CBT-OB is delivered in six modules (see Table 3), each including specific strategies and procedures that may be adapted to the patient’s individual progress and barriers; the six modules are introduced in a flexible and individualized way, according to the patient’s needs, across Phase 1 and Phase 2.
Each session lasts 45 minutes (90 minutes when the treatment is delivered in group), and is divided into five parts, each with a distinct objective, specifically:
- In-session collaborative weighing (up to 5 minutes)
- Reviewing self-monitoring and other homework (up to 10 minutes)
- Collaboratively setting the session agenda (about 2 minutes)
- Working through the agenda and agreeing on homework tasks (up to 30 minutes).
- Concluding the session (about 3 minutes). This includes summarizing what has been addressed in session, confirming the homework assignment(s), and scheduling the next appointment.
Day-hospital and residential CBT-OB, on the other hand, which are indicated for patients with severe and disabling obesity, last 21 days.
Finally, CBT-OB may be also associated with weight loss drugs and/or bariatric surgery in selected case, and can also be adapted for patients with obesity associated with binge-eating disorder (BED).
|
Table 3. The main procedures of the six CBT-OB modules
Module 1 - Monitoring food Intake, physical activity and body weight
- Initiating weekly weighing
- Explaining what the treatment will involve
- Educating on energy balance
- Establishing real-time monitoring of food intake and physical activity
- Initiating weekly weighing
Module 2 - Changing eating
- Creating an energy deficit of 500–1000 kcal per day produce a variable weight loss of about 0.5–1 kg a week.
- Planning ahead when, what and where to eat
- Continuing real-time monitoring of food intake
- Eating consciously to modify the beaviour
Module 3 - Developing an active lifestyle
- Assessing the patient’s eligibility for exercise
- Assessing the patient’s functional exercise capacity
- Motivating the patient to exercise
- Developing an active lifestyle, reducing sedentary activities and increasing the daily step count
- Improving physical fitness
- Continuing or commencing formal exercise (in selected cases)
Module 4 - Addressing obstacles to weight loss
- Educating the patients on cognitive-behavioural weight-loss obstacles (antecedent stimuli, positive consequences, problematic thoughts)
- Introducing the Weight-Loss Obstacles Questionnaire
- Creating the Personal Formulation
- Addressing weight-loss obstacles
- Reducing environmental stimuli
- Addressing events influencing eating and exercise habits
- Addressing impulses and emotions influencing eating and exercise habits
- Addressing problematic thoughts
- Addressing the use of food as a reward, and the patient’s rational excuses for not adopting an active lifestyle
Module 5 - Addressing weight-loss dissatisfaction
- Detecting weight-loss dissatisfaction and its reasons
- Addressing unrealistic weight goals
- Addressing dysfunctional primary goals for losing weight
- Addressing negative body image
Module 6: Addressing the obstacles to weight maintenance
- Reviewing the changes achieved through weight loss
- Educating the patient on weight maintenance
- Involving the patient actively in the decision to start weight maintenance
- Introducing the procedures for weight maintenance
- Establishing weekly self-weighing and a weight-maintenance range
- Adopting eating habits and physical activity habits conducive to weight maintenance
- Constructing a weight-maintenance mindset
- Identifying and addressing high-risk situations and preventing a lapse becoming a relapse
- Addressing weight regain
- Discontinuing real-time monitoring of food intake
- Evaluating possible future weight-loss attempts
- Preparing a weight-maintenance plan
- Bringing the treatment to a close
|
4. The Current Status of Personalized CBT-OB
The research findings may be summarised as follows:
- A randomized control trial assessing the effectiveness of personalized CBT-OB (3 weeks of residential CBT-OB followed by outpatient CBT- OB) found that weight loss at 43 weeks in completers (n=69) was about 15%. The treatment was associated with improvements in cardiovascular risk factors and psychological profiles; what is more, no tendency to regain weight was observed between 6 and 12 months[6].
- A real-world study, conducted in an Italian National Health Service obesity clinic, assessed the effectiveness of group CBT-OB in 67 patients with severe obesity. 76.2% patients completed the treatment, displaying an average weight loss of 11.5% after 6 months and 9.9% after 18 months. This weight loss was associated with a significant reduction in cardiovascular risk factors, anxiety, depression and eating-disorder psychopathology, and an improvement in obesity-related quality of life[7].
- A study compared the long-term effects of residential CBT-OB in 54 patients with severe obesity with or without BED. Even though patients did not receive outpatient CBT-OB after discharge, at 5-year follow-up, 51.5% of the former group no longer met the diagnostic criteria for BED. Moreover, no difference was observed between the two groups in terms of mean weight loss (6.3 kg in BED vs. 7.4 kg in non-BED)[8].
