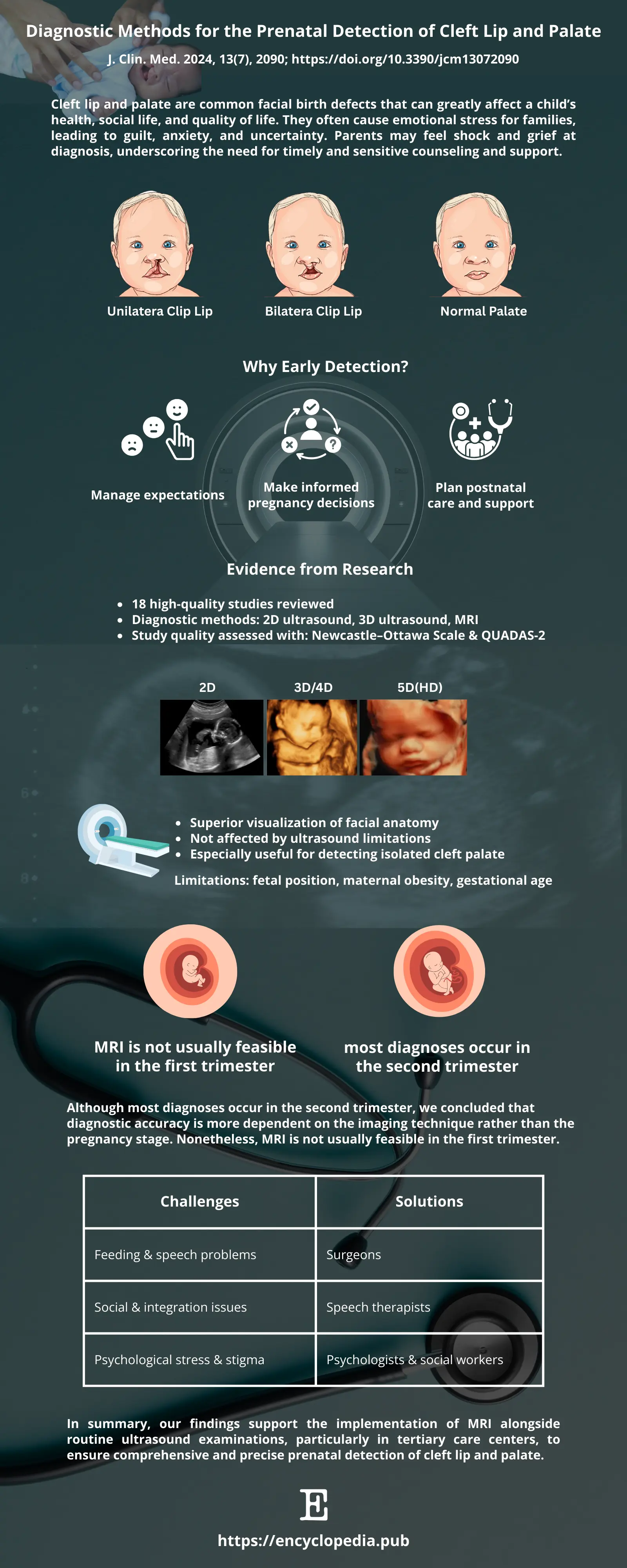
Seeing your baby’s face for the first time on an ultrasound is an unforgettable moment. For a small but significant number of families, that moment can also raise questions—could a cleft lip or cleft palate be present? Early, accurate detection matters: it informs clinical planning, supports prenatal counseling, and helps families prepare emotionally and practically.
Source: Encyclopedia Scientific Infographic (https://encyclopedia.pub/image/3758)
1. Ultrasound: The First Line of Defense
For most parents-to-be, ultrasound is the first glimpse of their baby. Traditional 2D ultrasound is widely used, safe, and effective—but it’s not perfect. Factors like the baby’s position, maternal body type, and the type of cleft can all affect how well it works.
2. Adding a Third Dimension
Enter 3D ultrasound. When paired with 2D imaging, it gives doctors a clearer view, especially for tricky cases like cleft palate. Think of it as switching from a flat sketch to a more detailed 3D model—it makes diagnosis more reliable.
3. MRI: The Backup Player That Shines
Sometimes ultrasound leaves doctors unsure. That’s when MRI can step in. MRI is excellent for spotting palate issues that ultrasound might miss. The downside? It’s expensive, less available, and usually reserved for specialized centers. Still, it can be a game-changer in complex cases.
4. Why Timing Matters
Most prenatal scans are performed during the second trimester, when fetal anatomy is easier to assess. However, the review highlights that there is no single “ideal” time for cleft detection. Earlier scans may identify concerns sooner, giving families more time to prepare, but they also carry a higher risk of missed or uncertain findings. Later scans can offer sharper detail, yet may delay decision-making. In practice, timing is a balance—what matters most is using the right imaging tool at the right stage.
5. Guidance for Families When a Cleft is Suspected
A possible diagnosis on ultrasound can feel overwhelming, but several practical steps can turn uncertainty into clarity and preparation:
-
Schedule a focused follow-up scan. A repeat 2D ultrasound with an experienced sonographer, ideally paired with 3D imaging, can often confirm or rule out the condition.
-
Seek specialist input. Referral to a fetal medicine clinic or a cleft care team provides access to expert evaluation and tailored counseling.
-
Use MRI for complex cases. If palate anatomy is unclear and detailed soft-tissue views are critical, MRI can add valuable information where ultrasound is limited.
-
Plan ahead with support. An early and accurate diagnosis gives families time to meet surgeons, feeding specialists, and speech therapists—ensuring the baby’s care plan is ready from day one.
6. Clinical Implications and the Way Forward
This review reinforces a simple but important point: no single test is perfect. 2D ultrasound remains the backbone of prenatal screening, but combining 2D with 3D—and using MRI selectively—yields the most reliable results. For clinicians, that means implementing clear referral pathways and collaborative workflows. For healthcare systems, it underscores the need to improve access to advanced imaging and to train sonographers in targeted fetal facial assessment.
Future research should aim for standardized imaging protocols, larger prospective studies, and clearer guidelines on the optimal timing and combination of imaging modalities. Until then, a stepwise diagnostic approach—start with 2D, add 3D when needed, and reserve MRI for ambiguous or complex cases—offers a practical path for accurate prenatal counseling and planning.
For more information about topic, you can view the online Infographic entitled "Prenatal Detection of Cleft Lip and Palate".
