Intraoperative OCT is an innovative and promising technology which allows anterior and posterior segment ocular surgeons to obtain a near-histologic cross-sectional and tomographic image of the tissues. Intraoperative OCT has several applications in ocular surgery which are particularly interesting in the context of corneal transplantation. Indeed, iOCT images provide a direct and meticulous visualization of the anatomy, which could guide surgical decisions. In particular, during both big-bubble and manual DALK, the visualization of the relationship between the corneal layers and instruments allows the surgeon to obtain a more desirable depth of the trephination, thus achieving more type 1 bubbles, better regularity of the plane, and a reduced risk of DM perforation. During EK procedures, iOCT supplies information about proper descemetorhexis, graft orientation, and interface quality in order to optimize the postoperative adhesion and reduce the need for re-bubbling. Finally, mushroom PK, a challenging technique for many surgeons, can be aided through the use of iOCT since it guides the correct apposition of the lamellae and their centration. The technology of iOCT is still evolving: a larger field of view could allow for the visualization of all surgical fields, and automated tracking and iOCT autofocusing guarantee the continued centration of the image.
1. Intraoperative OCT: Technology and Characteristics
Anterior segment OCT (AS-OCT) was described for the first time in 1994 by Izatt et al. as an essential tool for the clinical diagnosis and follow up of many corneal pathologies [
1]. Thanks to its high level of resolution, AS-OCT provides a near-histologic cross-sectional and tomographic image of the tissues, allowing for the detailed evaluation of clinical conditions, and is able to impact medical and surgical decisions. The introduction of this technology into the operating room was a natural consequence considering its several potential applications during both anterior and posterior segment surgery. Indeed, intraoperative OCT (iOCT) provides immediate feedback on the tissues’ anatomic configuration and could potentially directly guide surgical manipulations.
Standard OCT systems were unsuitable for a surgical setting due to their large dimensions and the traditional sitting position required for image acquisition, which was not practical for supine patients. The introduction of portable OCT systems allowed for the introduction of this tool into the operating room. The first two iOCT systems developed were the Bioptigen EnVisu (Bioptigen, Research Triangle Park, NC/Leica, Wetzlar, Germany) and the Optovue iVue (Optovue, Fremont, CA, USA) [
2,
3,
4,
5,
6,
7]. These systems were available in different configurations such as handheld, externally mounted, and microscope-mounted. Handheld imagine acquisition, although characterized by excellent image quality, is limited by potential motion artifacts, which could delay image capture and affect the quality of the resulting frames. In order to surpass these limitations, microscope-mounted systems were developed. These systems provided better stability; moreover, foot-pedal control of the microscope allowed for control of the probe location, with enhanced image reproducibility [
8,
9].
A major advance was achieved with the introduction of microscope-integrated OCT (MIOCT), which could finally enable the acquisition of real-time intraoperative OCT sections and the visualization of the instrument–tissue interaction [
10,
11]. Two of the currently most diffuse systems are the Zeiss OPMI LUMERA 700 (Carl Zeiss Meditec, Inc., Oberkochen, Germany) and the Leica Proveo 8 (Leica Microsystems, Wetzlar, Germany). Similar to the microscope-mounted systems, an MIOCT can be controlled by a foot pedal; furthermore, a heads-up display provides a combined visualization of the surgical field and the OCT data stream.
At first, iOCT was employed in vitreoretinal surgery, focusing on macular hole [
8,
12,
13], vitreomacular traction [
14,
15], epiretinal membrane [
16,
17], and retinal detachment surgery [
18,
19]. More recently, it has been applied to glaucoma surgery [
20], implantable collamer lens (ICL) implantation [
21], cataract surgery [
22], and corneal transplantation [
23,
24]. Concerning corneal surgery, its application is mainly related to lamellar surgery, both anterior and endothelial. Indeed, iOCT allows for a better visualization of the corneal layers, an evaluation of the instrument’s depth during anterior lamellar surgery, and confirmation of the complete adhesion of the lamella during endothelial surgery.
2. Intraoperative OCT Applications for Lamellar Corneal Surgery
Guiding Big-Bubble Deep Anterior Lamellar Keratoplasty (BB-DALK)
Deep anterior lamellar keratoplasty (DALK) is the gold standard for the treatment of diseases of the anterior cornea, such as corneal ectasia, anterior stromal leucomas, and stromal dystrophies. In terms of improved visual acuity, DALK is associated with better outcomes than penetrating keratoplasty thanks to lower incidences of post-operative astigmatism and rejection [
25,
26]. Moreover, this technique does not require an open-sky approach, thus limiting possible risks and complications associated with the surgery [
27,
28].
There are several applications of iOCT, aimed mostly at avoiding the conversion to PK. First, it allows for the assessment of the corneal and anterior segment architecture, thus determining corneal thickness and regularity, and for the detection of the presence of anomalies such as Descemet’s membrane (DM) rupture or peripheral anterior synechiae. The definition of corneal anatomy aids in making decisions about the depth of trephination, which can be identified by a vertical hyperreflective band along the anterior stroma in the peripheral cornea, where the cut was made. In their study, Santorum et al. suggested an intended stromal bed of 150 μm within the posterior corneal surface, measured with the built-in caliper tool of the intraoperative OCT software (InVivoVue, IVV 2.18, Lumivero. Denver, CO, USA) [
29]. However, in all their eyes, they needed to further extend the groove after the first trephination in order to obtain the desirable depth. Usually, we establish the depth of trephination based on the full thickness measured on the iOCT. The aim is to leave a residual stromal thickness of about 100 μm and thus reach the pre-Descemetic plane. The PIONEER study detected an incidence of further dissection after the initial trephination in 55.6% of cases, determined by an evaluation made by the surgeon in light of an iOCT scan [
9].
In BB-DALK surgery, the second step is the insertion of a cannula or needle into the stroma to create an air bubble. iOCT allows for the real-time visualization of the instrument, which can aid in guiding the insertion to the desirable depth and in the right direction. However, the visualization of the layers under the cannula can be masked by the hyperreflectivity of the instrument itself, hampering the correct assessment of the thickness of the tissue. In order to obtain the measurement of the residual stromal tissue, it is possible to remove the cannula and then, by acquiring a longitudinal iOCT scan, observe the presence of a stromal pocket, which is visible as an hyperreflective line along the posterior stroma [
30]. Alternatively, even if the cannula is not removed from the scleral pocket, a transversal iOCT scan across the width of the instrument can still allow for the visualization of a hyperreflective line extending laterally to the shadow of the cannula, similar to a “seagull wing” appearance (
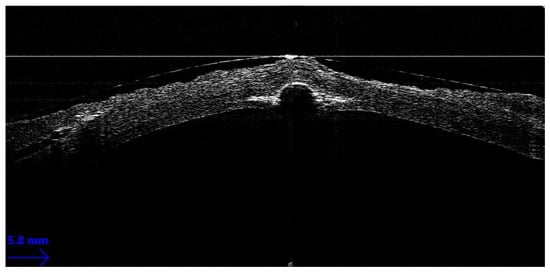
Figure 1). Once this line is identified, the measurement of the residual stromal bed can be performed with the caliper, which is usually integrated into the iOCT’s software, using the “seagull wing” as a reference.
Figure 1. Seagull wing sign.
The proper identification of the residual stromal thickness under the cannula is useful for predicting the probability of achieving the big bubble. In 2013, Scorcia and colleagues observed how the distance between the cannula tip and the DM was significantly smaller (90.4 ± 27.7 μm) in cases in which a big bubble was achieved than in a group of unsuccessful surgeries (136.7 ± 24.2 μm) [
31]. Indeed, corneal surgeons routinely employing iOCT could corroborate their evaluation of stromal depth with actual real-time thickness measurements, deciding whether a repositioning of the cannula to a deeper stromal plane is advisable and weighing the higher chances of achieving a big bubble with the increased risk of perforation.
The next step is the creation of the big bubble itself is to obtain a cleavage plan of the posterior stroma. The successful formation of the bubble is visualized on iOCT scans by observing the separation between the corneal stroma and DM, visible as a clear space between the internal concave surface and the external convex surface [
32]. iOCT is capable of detecting sub-clinical big bubbles that are indistinguishable to the human eye in 40% of cases [
33]. Moreover, iOCT could theoretically help to differentiate a type 1-BB from a type 2-BB by measuring the posterior wall of the bubble, which is made by pre-Descemetic stroma (the so-called Dua’s layer) and DM in type 1 and by DM only in type 2. The posterior wall of type 2 bubbles should therefore be thinner than the type 1 wall, even though this difference is in the order of a few microns and modern iOCT has not yet attained an image resolution capable of consistently differentiating the two bubbles [
34]. In cases of formation of small air bubbles distributed over the whole stroma, iOCT helps in identifying each bubble, allowing the surgeon to puncture them with a sharp instrument (e.g., a 15-degree blade) to create a bigger cavity, thus rescuing the surgery and proceeding with the stromal dissection without the need of a conversion to PK [
35] (
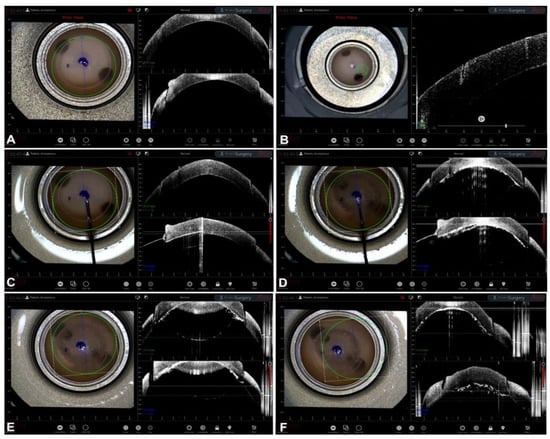
Figure 2).
Figure 2. BB-DALK. (A) Stromal trephination. (B) Detail of the vertical hyperreflective band along the anterior stroma. (C) Insertion of the cannula. (D) Injection of air and bubble formation. (E) Bubble profile. (F) Detail of bubble and trephination.
This entry is adapted from the peer-reviewed paper 10.3390/jcm12093048