The term COPD may not be precise in distinguishing various pulmonary conditions, including asthma, which can pose difficulties in distinguishing asthma from COPD, particularly among smokers and older adults. Moreover, some patients may exhibit clinical features that are common to both asthma and COPD. The diagnosis of pneumonia based solely on clinical signs and laboratory data can be challenging, given the variability of clinical presentations, particularly in the presence of chronic respiratory illness. The literature on COPD often lacks clarity in defining, documenting, classifying, and attributing pneumonia events in terms of severity. Furthermore, variations in the methods used to document and evaluate pneumonia across different countries can contribute to the variability in reported incidence rates, making cross-trial comparisons problematic. Patients with severe forms of COPD may experience exacerbations that can be challenging to differentiate clinically and radiographically from pneumonia, resulting in an overestimation of the number of pneumonia cases in these trials.
1. Introduction
1.1. Pneumonia in Patients with COPD Independent of the Use of ICS
Although pneumonia is often seen as a potential side effect of inhaled corticosteroids (ICSs) in individuals with chronic obstructive pulmonary disease (COPD), the actual frequency of pneumonia varies across studies, and certain analyses have reported varying rates of pneumonia associated with different types of ICS treatments [
1,
2,
3].
Several randomized controlled trials (RCTs) that involved a significant number of participants did not demonstrate an increase in the occurrence of pneumonia in patients who were randomly assigned to undergo ICS treatment [
4,
5,
6]. These findings imply that other factors, which are not related to the utilization of ICSs, could impact the probability of developing pneumonia in individuals with COPD.
1.2. Definition of COPD and Pneumonia
Patients with acute exacerbations of COPD (AECOPD), a serious public health issue, may exhibit symptoms resembling pneumonia.
Clinically relevant pneumonia can be differentiated from other comparable illnesses using traditional diagnostic criteria including a differential blood count and C-reactive protein (CRP) levels. However, such methods have suboptimal sensitivity and specificity in patients with suspected infections, leading to uncertainty when starting treatment [
9].
Bacterial colonization has been linked to increased inflammation, symptom aggravation, and more frequent exacerbations. Nearly 44% of all samples collected from stable COPD patients tested positive for bacterial colonization [
10].
2. Various Aspects of Infection in COPD and Its Capacity to Generate Pneumonia
It is widely acknowledged that potentially harmful microorganisms can inhabit the bronchial area in individuals with COPD. Studies have indicated that the composition of the lung microbiome in patients with stable COPD differs significantly from that of healthy individuals [
11,
12,
13,
14,
15,
16,
17,
18]. There is evidence of a relationship between the appearance of exacerbation symptoms and the acquisition of new bacterial strains [
19]. The majority of information about COPD is obtained from samples collected through various methods such as biopsies, lung tissue explants, bronchoalveolar lavage (BAL), protected specimen brush (PSB) techniques, and sputum. Research studies have shown that sputum samples contain different types of microorganisms compared to bronchoalveolar samples, and it has been confirmed that the lungs of COPD patients have unique microbiomes that differ from healthy individuals in terms of bacterial composition [
20,
21]. Alterations in the microbiome of the upper or lower respiratory tract can affect the immune response and make the host more vulnerable to developing pneumonia [
22].
Antibiotic resistance in bacteria that cause community-acquired pneumonia (CAP) such as pneumococci and Mycoplasma pneumoniae is becoming more common, which is a significant global health concern and a contributing factor in the increasing burden of disease, particularly in COPD patients. This information has been reported by several studies, including references [
23,
24,
25].
Pathogens have several ways of developing resistance to antibiotics, such as producing beta-lactamase, losing outer membrane proteins that are susceptible to antibiotics, changing their targets, forming biofilms, using efflux pumps, and acquiring integrons. The use of antibiotics at low concentrations can also contribute to the development of resistance among the exposed pathogens. Apart from the misuse of antibiotics in healthcare, the general population is exposed to non-iatrogenic antibacterial drugs in their daily lives, such as antibiotics used in the meat industry to treat livestock, leading to an increase in drug resistance in pathogens. The increased use of antibiotics in both clinical and nonclinical settings has resulted in an increasing number of clinically isolated drug-resistant strains, including carbapenem-resistant Klebsiella pneumoniae [
26].
The symptoms of SARS-CoV-2 infection can vary widely, from showing no symptoms at all to developing atypical pneumonia. COVID-19 pneumonia is a disease that continues to evolve over time. In fact, around 40% of cases of SARS-CoV-2 infection do not display any symptoms, another 40% have mild upper respiratory symptoms, and approximately 20% develop pneumonia [
27,
28,
29].
Klebsiella species consist of Klebsiella ozaenae, Klebsiella rhinoscleroma, and Klebsiella pneumoniae, with the latter having significant clinical implications as an important opportunistic and iatrogenic infectious pathogen. K. pneumoniae typically colonize different mucosal surfaces, including the upper respiratory tract, in humans. They are a significant cause of respiratory tract infections that can result in severe pneumonia and are transmitted to the human body via contaminated respirators, atomizers, catheters, and through self-contamination by colonizing bacteria.
The immunological system’s growth and maintenance, as well as general health, depend significantly on microflora. Dysbiosis, or changes in the microbial makeup and function in the intestinal and respiratory tract, has recently been connected to variations in immune responses and pulmonary development. Chronic gastrointestinal tract (GIT) disorders such as inflammatory bowel disease (IBD) or irritable bowel syndrome (IBS) frequently coexist with chronic lung diseases such as asthmatic processes or COPD.
Adults with IBD (up to 50%) and IBS (up to 33%) may exhibit symptoms of pulmonary inflammation or compromised pulmonary function. IBD diagnoses are also more common in COPD patients.
In patients with COPD, the intestinal lining is more permeable than in healthy individuals. Although the GIT and respiratory tract have different functions and environments, they share a common embryonic origin and structural similarities. Thus, it is not surprising that they can interact in both health and disease [
30,
31,
32,
33,
34].
Research indicates that commensal microbes in the respiratory tract may contribute to the development of pneumonia. Furthermore, studies have shown that the intestinal microbiota play a crucial role in regulating local and systemic host responses in clinically relevant models of pneumonia. The intestinal microbiota have been shown to offer protection against pneumonia by priming alveolar macrophages. The interaction between the intestine and lungs during infection has been observed, and it has been suggested that the intestinal microbiota can modulate the immune response in the lungs [
35,
36].
Periodontal diseases are a group of infectious conditions caused by multiple microorganisms, such as gingivitis and periodontitis, that affect the tissues supporting the teeth. These diseases have been associated with the worsening of various respiratory diseases. The presence of pathogens in the mouth can directly enter the lungs, increasing the risk of acute exacerbations of chronic obstructive pulmonary disease (AECOPD) or community-acquired pneumonia (CAP) in individuals with COPD [
37].
Vaccination against influenza, as well as Pneumococcus pneumoniae, has been proven to be effective in preventing infections not only in patients with COPD but also in individuals who are in close contact with them, thus reducing the risk of transmission. Encouraging complete vaccination can contribute to better healthcare management and allocation for patients with COPD [
38,
39] (
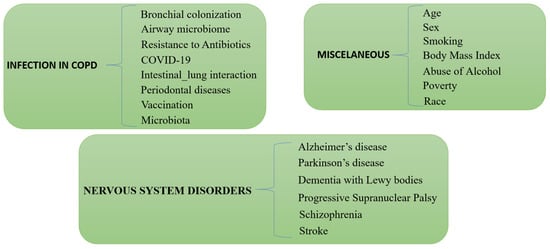
Figure 1).
Figure 1. Infections in COPD, miscellaneous, and nervous system disorders as causes of pneumonias in COPD independent of the use of ICS.
2.1. Miscellaneous: Age, Sex, Body Mass Index, Smoking, and Social Status
The elderly are more likely to develop pneumonia due to decreased organ function and an aging immune system, and may suffer multiple organ dysfunction syndrome (MODS), respiratory and circulatory failure, and even death. In fact, pneumonia has become one of the leading causes of death in the elderly [
40].
The likelihood of developing community-acquired pneumonia (CAP) depends on age and underlying medical conditions, with older individuals aged 65 or above who have COPD being at a higher risk. Within the COPD population, those aged 65–79 or over 80 are more susceptible to CAP than those aged 45–65. Several independent factors have been identified for recurrent CAP in adults, including COPD, older age, and a lack of pneumococcal vaccination [
6,
40,
41,
42,
43,
44].
The impact of seasonal influenza on health varies based on age and pre-existing medical conditions. Individuals aged 65 or older with COPD are at higher risk of serious medical complications leading to hospitalization and death. COPD is the third leading cause of death among people aged 65 and above in the United States. About 15 million adults in the US have been diagnosed with COPD, and 5 million of them are aged 65 or older. For people with COPD, influenza infection can cause severe complications and even death, especially in older adults. Patients with COPD have a higher risk of respiratory failure and are more likely to exhibit frailty. Any respiratory infection, including influenza, can cause airway inflammation and constriction, making it difficult to breathe properly. This inflammation can increase the likelihood of COPD exacerbations. As a result, people with COPD are advised to receive seasonal influenza vaccination [
45].
Adjusted incidences of all types of pneumonia, including community-acquired pneumonia (CAP) and hospital-acquired pneumonia (HAP), are higher in men than in women. Specifically, men have a 47% higher adjusted incidence of CAP and a 98% higher adjusted incidence of HAP than women. Furthermore, men with COPD have a higher risk of developing pneumonia than women with COPD [
46].
A single predictive factor for COPD is body mass index (BMI), and there is a direct correlation between lower body weight and higher death rates in COPD patients. While evidence suggest that people who can acquire weight have a better prognosis, more weight loss increases the danger. The prognostic relevance of a low BMI could be the result of waste in end-stage COPD. In turn, underweight patients may be less resistant to infections such as pneumonia [
47,
48,
49].
Additionally, smoking has been recognized as a risk factor for CAP, with the likelihood altering depending on the history of smoking. Smoking’s impact on the risk of CAP has been studied. Smoking was verified as an independent risk factor in the multivariate analysis, and both current smokers and former smokers were shown to have a greater risk of CAP compared to non-smokers. With higher pack years, the risk grew higher. The risk of CAP was substantially greater in ex-smokers who had quit smoking more recently (4 years) compared to those who had quit smoking less recently. Those who had never smoked but were exposed to passive smoking were similarly at a significantly higher risk of CAP. Likewise, elderly individuals aged 65 years or older who were subjected to involuntary exposure to passive smoke within their domestic environment exhibited a heightened susceptibility to community-acquired pneumonia (CAP). It has been observed that individuals who are current smokers and aged 65 years or above, are at a greater risk of contracting the infection compared to those who are ex-smokers, regardless of their age [
4,
6,
50,
51,
52,
53,
54,
55].
According to the Centers for Disease Control and Prevention (CDC), people who abuse alcohol are 10 times more likely to develop pneumococcal pneumonia and 4 times more likely to die from pneumonia than non-drinkers [
56,
57]. Heavy drinkers are more likely to suffer from COPD according to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) criteria and suffer more respiratory symptoms [
58].
Poverty is associated with an increased risk of pneumonia [
59]. Although race is a characteristic that must be taken into account, it can be conditioned by other co-existing factors such as socioeconomic condition. For example, Black adults in the United States are 2.6 times more likely to develop pneumonia than Caucasian adults, although in general, the former are also 4.4 times poorer than Caucasian adults [
60,
61] (
Figure 1).
2.2. Nervous System Disorders
Advanced-stage Alzheimer’s disease (AD) is often accompanied by two serious medical conditions: dysphagia and aspiration pneumonia. Dysphagia associated with pseudobulbar palsy can cause weight loss, despite attempts to manage swallowing difficulties. The underlying mechanisms that regulate the body’s basic functions, such as maintaining nutritional status, appear to be impaired in these patients. Aspiration pneumonia is the leading cause of death in end-stage AD.
Aspiration pneumonia is caused by a number of factors such as dysphagia, reduced consciousness, a loss of gag reflex, periodontal disease, and the mechanical effects of inserting tubes into the respiratory and gastrointestinal tracts. The bacteria responsible for the infection include oral flora, mostly aerobes, and nosocomial-acquired pathogens, such as Staphylococcus aureus, aerobic and facultative Gram-negative bacilli, which may colonize patients in hospitals and nursing homes. Besides the use of antibiotics, addressing the symptoms and managing AD in patients with pneumonia is critical in alleviating their suffering [
32].
Neurological disorders such as Alzheimer’s disease, Parkinson’s disease, Lewy bodies, and progressive supranuclear palsy have been found to increase the risk of pneumonia that is confirmed through autopsy. Patients with these conditions are often bedridden and may experience dysphagia, altered mental states, or respiratory muscle weakness, all of which can increase the risk of pneumonia. Additionally, the causes of pneumonia in patients with neurological conditions who also have COPD may be different from those in the general population, which can lead to differences in the distribution of pathogens causing the infection [
62].
Patients with schizophrenia are at increased risk of developing pneumonia, as well as other respiratory diseases such as COPD and asthma [
63].
HAD is one of the most important complications that can be prevented in a patient who has suffered a stroke. The occurrence of pneumonia worsens the prognosis of a patient, especially if he or she has had an ischemic stroke, reducing the chances of a full recovery and increasing the chances of bodily deterioration that can lead to the patient’s death. Although the chances of developing pneumonia in the general population range from approximately 8% to 30%, it increases to 44% in patients with COPD and who have had a stroke [
64] (
Figure 1)
This entry is adapted from the peer-reviewed paper 10.3390/biomedicines11051243