Liver cirrhosis is a chronic disease that can be complicated by episodes of decompensation such as variceal bleeding, hepatic encephalopathy, ascites, and jaundice, with subsequent increased mortality. Infections are also among the most common complications in cirrhotic patients, mostly due to a defect in immunosurveillance. Among them, one of the most frequent is spontaneous bacterial peritonitis (SBP), defined as the primary infection of ascitic fluid without other abdominal foci. SBP is mainly induced by Gram-negative bacteria living in the intestinal tract, and translocating through the intestinal barrier, which in cirrhotic patients is defective and more permeable.
- cirrhosis
- spontaneous bacterial peritonitis
- gut-liver axis
- microbiota
- intestinal barrier
- bacterial translocation
1. Introduction
2. Infections and Liver Cirrhosis
2.1. Immune-Paralysis: Molecular and Cellular Mechanisms
2.2. Infections and Liver Cirrhosis: Clinical Concerns
2.3. Clinical Features of SBP
3. The Gut–Liver Axis in the Pathogenesis of SBP
3.1. Bacterial Translocation in Liver Cirrhosis
Portal hypertension causes a profound dysfunction of the gut–liver axis. The vasodilation of splanchnic vessels reduces blood flow velocity and capacitance in the intestinal mucosa, leading to a chronic ischemic condition. This acts as an inflammatory trigger, inducing fibromuscular proliferation of the intestinal layers and modifying the morphological characteristics of enterocytes [41]. In a descriptive pilot study, intestinal biopsies from a population of cirrhotic patients showed a reduced representation of tight junctions (TJ) proteins such as occludin and claudin 1. Histologically, loss of microvilli and reduced villi to crypt ratio have been evidenced too [41][42]. As a result of the epithelial barrier dysfunction, intestinal permeability is increased, realizing a condition also known as leaky gut, which promotes bacterial translocation and a consequent inflammatory cascade (Figure 2) [41]. The release of small amounts of PAMPs, such as endotoxins, lipopolysaccharides (LPS), and bacterial DNA, from the gut into the portal venous system to extra-intestinal sites is a physiological process, which has been described even in healthy subjects, with no clinical consequences. However, in patients with liver cirrhosis, bacterial translocation is exacerbated by several pathological mechanisms such as reduced secretion of defensins and regenerating islet-derived proteins (RegIIIβ and RegIIIγ), thickening of the inner mucus layer by over-expression of MUC2, reduced intestinal intraluminal concentration of secondary bile acids, decreased mucosal IgA secretion, impaired gastric acid secretion, and slower oro-cecal transit time (OCTT) due to ineffective gastrointestinal peristalsis [43]. Bacterial translocation underlies immunotolerance in cirrhotic patients; indeed, chronic inflammation induces a dysfunction of the innate and adaptive immune response, which together with the reduced number of circulating leukocytes due to hypersplenism and the reduced production of humoral and complement factor leads to a sort of “immune paralysis” [44]. Moreover, phagocytosis stimulated by the binding of LPS with TLR4 on the macrophage surface is ineffective, and secondly the Kupffer cells activated by bacterial products release multiple cytokines in a sort of “cytokine storm”, enhancing liver damage [45]. The vicious circle that links gut dysbiosis, bacterial translocation, and liver cirrhosis is described in Figure 2.
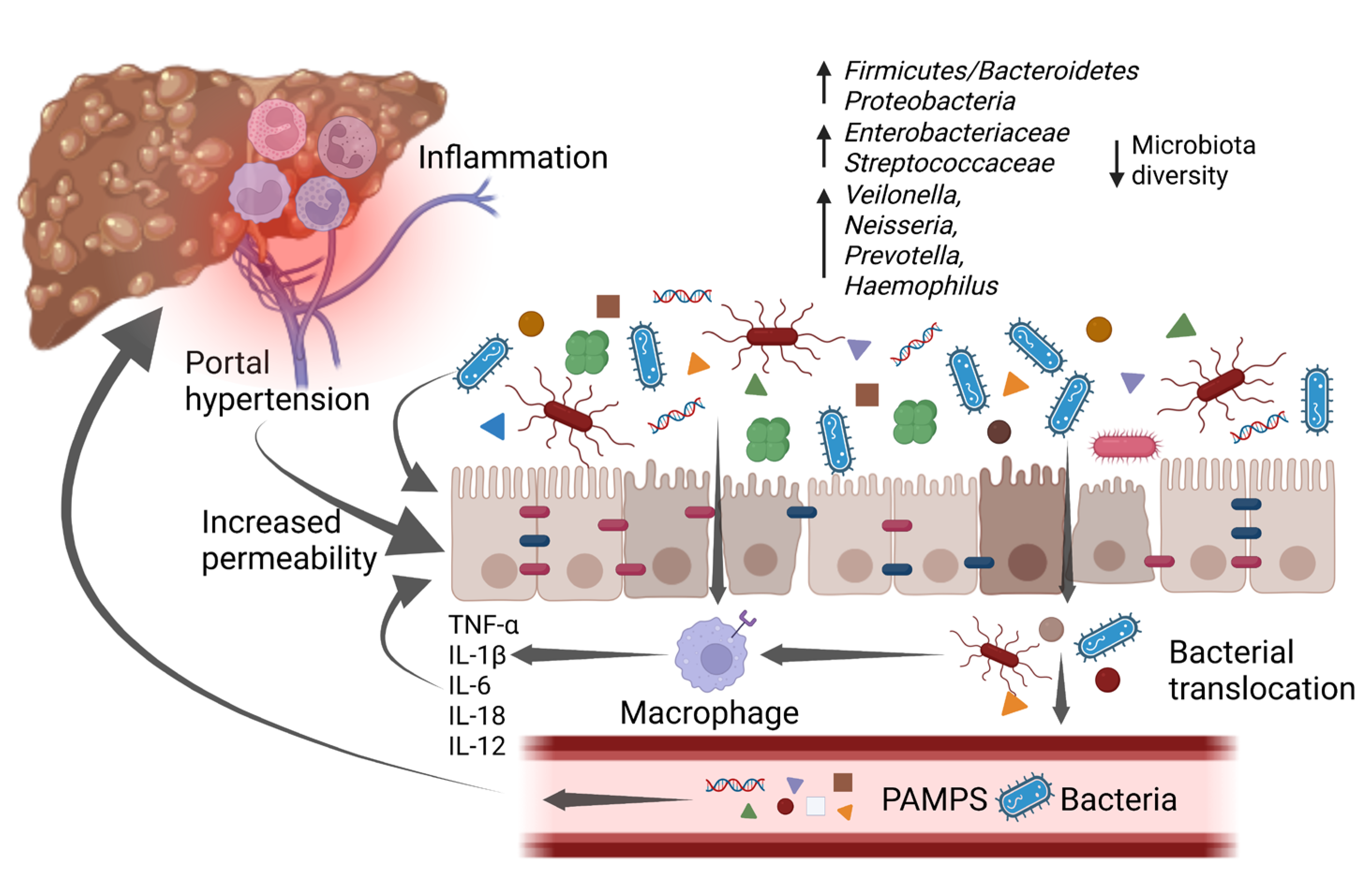 Figure 2. An increase in pro-inflammatory bacteria and a reduction in overall diversity are typical of gut microbiota changes associated with cirrhosis. These changes promote a low-grade chronic inflammatory state that impairs intestinal barrier function, which is already affected by portal hypertension, leading to a condition known as “leaky gut”. The increased intestinal permeability, along with the disrupted immune system, allows bacterial translocation and the increase of bacterial metabolites in the bloodstream. As a consequence, it enhances inflammation which worsens intestinal barrier disruption and in the liver promotes cirrhosis progression, with the emergence of its complications. IL-1β: interleukin-1β; IL-6: interleukin-6; IL-12: interleukin-12; IL-18: interleukin-18; PAMPs: pathogen-associated molecular patterns; TNF-α: tumor necrosis factor α. Created with BioRender.com accessed on 10 January 2023.
Figure 2. An increase in pro-inflammatory bacteria and a reduction in overall diversity are typical of gut microbiota changes associated with cirrhosis. These changes promote a low-grade chronic inflammatory state that impairs intestinal barrier function, which is already affected by portal hypertension, leading to a condition known as “leaky gut”. The increased intestinal permeability, along with the disrupted immune system, allows bacterial translocation and the increase of bacterial metabolites in the bloodstream. As a consequence, it enhances inflammation which worsens intestinal barrier disruption and in the liver promotes cirrhosis progression, with the emergence of its complications. IL-1β: interleukin-1β; IL-6: interleukin-6; IL-12: interleukin-12; IL-18: interleukin-18; PAMPs: pathogen-associated molecular patterns; TNF-α: tumor necrosis factor α. Created with BioRender.com accessed on 10 January 2023.
3.2. The Gut Microbiota in Cirrhotic Patients with SBP
Cirrhotic patients typically present qualitative and quantitative alterations of the gut microbiota composition, which worsen with the progression of the disease and hamper intestinal permeability and bacterial translocation [31][46]. Much evidence suggests that cirrhosis-related dysbiosis is characterized by the overabundance of pathogens such as Enterobacteriaceae and the depletion of beneficial commensals; furthermore, it is associated with the development of decompensation episodes as well as HCC, and may even identify patients at unfavorable prognosis [47][48][49][50]. Bacterial DNA can be detected in the ascites of half of cirrhotic patients even in the absence of SBP, probably due to bacterial opsonization [44]. Enterobacteriaceae, Streptococcus pneumoniae, and Streptococcus viridans are the bacterial species most frequently detected in the ascitic fluid of patients with SBP; among them, Escherichia coli is reported to be the most abundant, but also Gram-positive bacteria such as Staphylococcus, Streptococcus, and Enterococcus, as well as Helicobacter spp., including Helicobacter pylori, have been described [51]. Indeed, a remarkable result of the gastrointestinal dysfunction associated with liver cirrhosis is the oralization of the small intestinal and the colonic microbiota. About 48–73% of cirrhotic patients present a small intestinal bacterial overgrowth (SIBO), especially those with previous episodes of SBP or hepatic encephalopathy [52]. In particular, oral species such as Streptococcus oralis and Streptococcus parasanguinis not only co-existed with enteric species, such as Enterococcus spp., Clostridium spp., and Erysipelatoclostridium ramnosum, but were correlated with disease severity [48].
Nonetheless, SBP is associated with further gut microbiota perturbations. In fact, a lower alpha and beta diversity was observed in the gut microbiota of patients with SBP, with an increase of Pantoea, Serratia marcescens, Klebsiella pneumoniae, Prevotella oris, Escherichia coli, Clostridioides difficile, Enterococcus, Veillonella spp., and other potential pathobionts, as well as a lower abundance of the Ruminococcus torques, Faecalibacterium prausnitzii, Methanobrevibacter smithii, and Lactobacillus reuteri [53][54].
4. Gut Microbiota Modulation as a Future Treatment for SBP
4.1. Probiotics, Prebiotics and Synbiotics
4.2. Enterosorbent Compounds and Bile Acids Signaling
4.3. Intestinal Motility
4.4. Other Experimental Treatments
This entry is adapted from the peer-reviewed paper 10.3390/life13040991
References
- Blachier, M.; Leleu, H.; Peck-Radosavljevic, M.; Valla, D.C.; Roudot-Thoraval, F. The burden of liver disease in Europe: A review of available epidemiological data. J. Hepatol. 2013, 58, 593–608.
- Mokdad, A.A.; Lopez, A.D.; Shahraz, S.; Lozano, R.; Mokdad, A.H.; Stanaway, J. Liver cirrhosis mortality in 187 countries between 1980 and 2010: A systematic analysis. BMC Med. 2014, 12, 14.
- Yung, Y.K.; Yim, H.J. Reversal of liver cirrhosis: Current evidence and expectations. Korean J. Intern. Med. 2017, 32, 213–228.
- Tsochatzis, E.A.; Bosch, J.; Burroughs, A.K. Liver cirrhosis. Lancet 2014, 383, 1749–1761.
- Piano, S.; Tonon, M.; Angeli, P. Changes in the epidemiology and management of bacterial infections in cirrhosis. Clin. Mol. Hepatol. 2021, 27, 437–445.
- Ascione, T.; Di Flumeri, G.; Boccia, G.; De Caro, F. Infections in patients affected by liver cirrhosis: An update. Infez. Med. 2017, 25, 91–97.
- Di Tommaso, N.; Gasbarrini, A.; Ponziani, F.R. Intestinal Barrier in Human Health and Disease. Int. J. Environ. Res. Public Health 2021, 18, 12836.
- Mattos, A.A.; Wiltgen, D.; Jotz, R.F.; Dornelles, C.; Fernandes, M.V.; Mattos, Z. Spontaneous bacterial peritonitis and extraperitoneal infections in patients with cirrhosis. Ann. Hepatol. 2020, 19, 451–457.
- Madrid, A.M.; Cumsille, F.; Defilippi, C. Altered small bowel motility in patients with liver cirrhosis depends on severity of liver disease. Dig. Dis. Sci. 1997, 42, 738–742.
- Huelin, P.; Piano, S.; Solà, E.; Stanco, M.; Solé, C.; Moreira, R.; Pose, E.; Fasolato, S.; Fabrellas, N.; de Prada, G.; et al. Validation of a staging system for acute kidney injury in patients with cirrhosis and association with acute-on-chronic liver failure. Clin. Gastroenterol. Hepatol. 2017, 15, 438–445.
- Wong, F.; Piano, S.; Singh, V.; Bartoletti, M.; Maiwall, R.; Alessandria, C.; Fernandez, J.; Soares, E.C.; Kim, D.J.; Kim, S.E.; et al. Clinical features and evolution of bacterial infection-related acute-on- chronic liver failure. J. Hepatol. 2020, 74, 330–339.
- Levesque, E.; Saliba, F.; Ichaï, P.; Samuel, D. Outcome of patients with cirrhosis requiring mechanical ventilation in ICU. J. Hepatol. 2014, 60, 570–578.
- Fernández, J.; Bert, F.; Nicolas-Chanoine, M.H. The challenges of multidrug-resistance in hepatology. J. Hepatol. 2016, 65, 1043–1054.
- Patel VC, Lee S, McPhail MJW, et al. Rifaximin-α reduces gut-derived inflammation and mucin degradation in cirrhosis and encephalopathy: RIFSYS randomised controlled trial. J Hepatol. 2022;76(2):332-342. doi:10.1016/j.jhep.2021.09.010
- Patel VC, Lee S, McPhail MJW, et al.; Rifaximin-α reduces gut-derived inflammation and mucin degradation in cirrhosis and encephalopathy: RIFSYS randomised controlled trial.. J Hepatol. 2022, 76(2), 332-342, doi:10.1016/j.jhep.2021.09.010.
- Bajaj, J.S.; Reddy, K.R.; Tandon, P.; Garcia-Tsao, G.; Kamath, P.S.; O’Leary, J.G.; Wong, F.; Lai, J.; Vargas, H.; Thuluvath, P.J.; et al. Association of serum metabolites and gut microbiota at hospital admission with nosocomial infection development in patients with cirrhosis. Liver Transplant. 2022, 28, 1831–1840.
- Bernsmeier, C.; Van der Merwe, S.; Périanin, A. Innate immune cells in cirrhosis. J. Hepatol. 2020, 73, 186–201.
- Lebossé, F.; Gudd, C.; Tunc, E.; Singanayagam, A.; Nathwani, R.; Triantafyllou, E.; Pop, O.; Kumar, N.; Mukherjee, S.; Hou, T.Z.; et al. CD8+T cells from patients with cirrhosis display a phenotype that may contribute to cirrhosis-associated immune dysfunction. EBioMedicine 2019, 49, 258–268.
- Corrigall, D.; Harris, N.; Devshi, D.; Fairclough, S.; Wright, G.; Trebicka, J.; Alessandria, C.; Angeli, P.; Jalan, R.; Claria, J.; et al. First description of the immune checkpoint receptor landscape in decompensated cirrhosis & ACLF. J. Hepatol. 2019, 70, E175–E176.
- Bajaj, J.S.; Kamath, P.S.; Reddy, K.R. The evolving challenge of infections in cirrhosis. N. Engl. J. Med. 2021, 384, 2317–2330.
- Stengel, S.; Quickert, S.; Lutz, P.; Ibidapo-Obe, O.; Steube, A.; Köse-Vogel, N.; Yarbakht, M.; Reuken, P.A.; Busch, M.; Brandt, A.; et al. Peritoneal level of CD206 associates with mortality and an inflammatory macrophage phenotype in patients with decompensated cirrhosis and spontaneous bacterial peritonitis. Gastroenterology 2020, 158, 1745–1761.
- Porcheray, F.; Viaud, S.; Rimaniol, A.-C.; Léone, C.; Samah, B.; Dereuddre-Bosquet, N.; Dormont, D.; Gras, G. Macrophage activation switching: An asset for the resolution of inflammation. Clin. Exp. Immunol. 2005, 142, 481–489.
- Martinez-Pomares, L. The mannose receptor. J. Leukoc. Biol. 2012, 92, 1177–1186.
- Wang, C.; Ma, C.; Gong, L.; Guo, Y.; Fu, K.; Zhang, Y.; Zhou, H.; Li, Y. Macrophage polarization and its role in liver disease. Front. Immunol. 2021, 12, 5381.
- Bansal, R.; Van Baarlen, J.; Storm, G.; Prakash, J. The interplay of the Notch signaling in hepatic stellate cells and macrophages determines the fate of liver fibrogenesis. Sci. Rep. 2015, 5, 18272.
- Arvanitakis, K.; Koletsa, T.; Mitroulis, I.; Germanidis, G. Tumor-associated macrophages in hepatocellular carcinoma pathogenesis, prognosis and therapy. Cancers 2022, 14, 226.
- Li, R.; Zhou, R.; Wang, H.; Li, W.; Pan, M.; Yao, X.; Zhan, W.; Yang, S.; Xu, L.; Ding, Y.; et al. Gut microbiota-stimulated cathepsin K secretion mediates TLR4-dependent M2 macrophage polarization and promotes tumor metastasis in colorectal cancer. Cell Death Differ. 2019, 26, 2447–2463.
- Labonte, A.C.; Tosello-Trampont, A.C.; Hahn, Y.S. The role of macrophage polarization in infectious and inflammatory diseases. Mol. Cells 2014, 37, 275.
- Tsuchiya, K.; Suzuki, Y.; Yoshimura, K.; Yasui, H.; Karayama, M.; Hozumi, H.; Furuhashi, K.; Enomoto, N.; Fujisawa, T.; Nakamura, Y.; et al. Macrophage mannose receptor CD206 predicts prognosis in community-acquired pneumonia. Sci. Rep. 2019, 9, 18750.
- Van der Merwe, S.; Chokshi, S.; Bernsmeier, C.; Albillos, A. The multifactorial mechanisms of bacterial infection in decompensated cirrhosis. J. Hepatol. 2021, 75, S82–S100.
- Bernardi, M.; Angeli, P.; Claria, J.; Moreau, R.; Gines, P.; Jalan, R.; Caraceni, P.; Fernandez, J.; Gerbes, A.L.; O’Brien, A.J.; et al. Recent advances in clinical practice Albumin in decompensated cirrhosis: New concepts and perspectives. Gut 2020, 69, 1127–1138.
- Li, L.; Chen, L.; Lin, F.; Mu, J.; Wang, D.; Zhang, W.; Mi, L.; Qin, Y.; Zhou, Y. Study of the expression of inflammatory factors IL-4, IL-6, IL-10, and IL-17 in liver failure complicated by coagulation dysfunction and sepsis. J. Inflamm. Res. 2021, 14, 1447–1453.
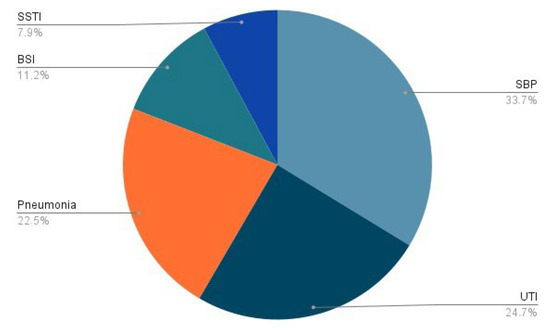
- Piano, S.; Singh, V.; Caraceni, P.; Maiwall, R.; Alessandria, C.; Fernandez, J.; Soares, E.C.; Kim, D.J.; Kim, S.E.; Marino, M.; et al. Epidemiology and effects of bacterial infections in patients with cirrhosis worldwide. Gastroenterology 2019, 156, 1368–1380.
- Bajaj, J.S.; Garcia-Tsao, G.; Biggins, S.W.; Kamath, P.S.; Wong, F.; McGeorge, S.; Shaw, J.; Pearson, M.; Chew, M.; Fagan, A.; et al. Comparison of mortality risk in patients with cirrhosis and COVID-19 compared with patients with cirrhosis alone and COVID-19 alone: Multicentre matched cohort. Gut 2020, 70, 531–536.
- Fernández, J.; Prado, V.; Trebicka, J.; Amoros, A.; Gustot, T.; Wiest, R.; Deulofeu, C.; Garcia, E.; Acevedo, J.; Fuhrmann, V.; et al. Multidrug-resistant bacterial infections in patients with decompensated cirrhosis and with acute-on-chronic liver failure in Europe. J. Hepatol. 2019, 70, 398–411.
- Such, J.; Runyon, B.A. Spontaneous bacterial peritonitis. Clin. Infect. Dis. 1998, 27, 669–674.
- Casafont, F.; Sánchez, E.; Martin, L.; Aguero, J.; Romero, F.P. Influence of malnutrition on the prevalence of bacterial translocation and spontaneous bacterial peritonitis in experimental cirrhosis in rats. Hepatology 1997, 25, 1334–1337.
- FFriedrich, K.; Baumann, C.; Brune, M.; Wannhoff, A.; Rupp, C.; Scholl, S.G.; Antoni, C.; Dollinger, M.; Neumann-Haefelin, C.; Weiss, K.H.; et al. Association of serum zinc levels with liver function and survival in patients awaiting liver transplantation. Langenbeck’s Arch. Surg. 2015, 400, 805–811.
- Yousif, M.M.; Sadek, A.M.E.M.; Farrag, H.A.; Selim, F.O.; Hamed, E.F.; Salama, R.I. Associated vitamin D deficiency is a risk factor for the complication of HCV-related liver cirrhosis including hepatic encephalopathy and spontaneous bacterial peritonitis. Intern. Emerg. Med. 2019, 14, 753–761.
- Tergast, T.L.; Laser, H.; Gerbel, S.; Manns, M.P.; Cornberg, M.; Maasoumy, B. Association between type 2 diabetes mellitus, HbA1c and the risk for spontaneous bacterial peritonitis in patients with decompensated liver cirrhosis and ascites. Clin. Transl. Gastroenterol. 2018, 9, e189.
- Nicoletti, A.; Ponziani, F.R.; Biolato, M.; Valenza, V.; Marrone, G.; Sganga, G.; Gasbarrini, A.; Miele, L.; Grieco, A. Intestinal permeability in the pathogenesis of liver damage: From non-alcoholic fatty liver disease to liver transplantation. World J. Gastroenterol. 2019, 25, 4814–4834.
- Paradis, T.; Bègue, H.; Basmaciyan, L.; Dalle, F.; Bon, F. Tight Junctions as a Key for Pathogens Invasion in Intestinal Epithelial Cells. Int. J. Mol. Sci. 2021, 22, 2506.
- Aguirre Valadez, J.M.; Rivera-Espinosa, L.; Méndez-Guerrero, O.; Chávez-Pacheco, J.L.; García Juárez, I.; Torre, A. Intestinal permeability in a patient with liver cirrhosis. Ther. Clin. Risk Manag. 2016, 12, 1729–1748.
- Wiest, R.; Lawson, M.; Geuking, M. Pathological bacterial translocation in liver cirrhosis. J. Hepatol. 2014, 60, 197–209.
- Tsuchida, T.; Friedman, S.L. Mechanisms of hepatic stellate cell activation. Nat. Rev. Gastroenterol. Hepatol. 2017, 14, 397–411.
- Qin, N.; Yang, F.; Li, A.; Prifti, E.; Chen, Y.; Shao, L.; Guo, J.; Le Chatelier, E.; Yao, J.; Wu, L.; et al. Alterations of the human gut microbiome in liver cirrhosis. Nature 2014, 513, 59–64.
- Ponziani, F.R.; Nicoletti, A.; Gasbarrini, A.; Pompili, M. Diagnostic and therapeutic potential of the gut microbiota in patients with early hepatocellular carcinoma. Ther. Adv. Med. Oncol. 2019, 11, 1758835919848184.
- Solé, C.; Guilly, S.; Da Silva, K.; Llopis, M.; Le-Chatelier, E.; Huelin, P.; Ginès, P. Alterations in gut microbiome in cirrhosis as assessed by quantitative metagenomics: Relationship with acute-on-chronic liver failure and prognosis. Gastroenterology 2021, 160, 206–218.
- Bajaj, J.S.; Heuman, D.M.; Hylemon, P.B.; Sanyal, A.J.; White, M.B.; Monteith, P.; Noble, N.A.; Unser, A.B.; Daita, K.; Fisher, A.R.; et al. Altered profile of human gut microbiome is associated with cirrhosis and its complications. J. Hepatol. 2014, 60, 940–947.
- Bajaj, J.S.; Hylemon, P.B.; Ridlon, J.M.; Heuman, D.M.; Daita, K.; White, M.B.; Monteith, P.; Noble, N.A.; Sikaroodi, M.; Gillevet, P.M. Colonic mucosal microbiome differs from stool microbiome in cirrhosis and hepatic encephalopathy and is linked to cognition and inflammation. Am. J. Physiol. Gastrointest. Liver Physiol. 2012, 303, 675–685.
- Feng, Y.; Chen, C.L.; Chen, T.H.; Liang, Y.H.; Chen, H.L.; Lin, C.Y.; Chiu, C.H. Application of next-generation sequencing to study ascitic microbiome in cirrhotic patients with or without spontaneous bacterial peritonitis. J. Microbiol. 2015, 48, 504–509.
- Guarner, C.; Soriano, G.; Tomas, A.; Bulbena, O.; Novella, M.T.; Balanzo, J.; Vilardell, F.; Mourelle, M.; Moncada, S. Increased serum nitrite and nitrate levels in patients with cirrhosis: Relationship to endotoxemia. Hepatology 1993, 18, 1139–1143.
- Bajaj, J.S.; Rodriguez, M.P.; Fagan, A.; McGeorge, S.; Sterling, R.K.; Lee, H.; Gillevet, P.M. Impact of Bacterial Infections and SBP Prophylaxis on Phage-Bacterial Dynamics in Cirrhosis. Hepatology 2022, 76, 1723–1734.
- Zhou, Z.; Lv, H.; Lv, J.; Shi, Y.; Huang, H.; Chen, L.; Shi, D. Alterations of gut microbiota in cirrhotic patients with spontaneous bacterial peritonitis: A distinctive diagnostic feature. Front. Cell Infect. Microbiol. 2022, 12, 999418.
- Mücke, M.M.; Rüschenbaum, S.; Mayer, A.; Mücke, V.T.; Schwarzkopf, K.M.; Zeuzem, S.; Lange, C.M. Stool and sputum microbiome during quinolone prophylaxis of spontaneous bacterial peritonitis: An exploratory study. Gut Pathog. 2020, 12, 51.
- Ponziani, F.R.; Gerardi, V.; Pecere, S.; D’Aversa, F.; Lopetuso, L.; Zocco, M.A.; Pompili, M.; Gasbarrini, A. Effect of rifaximin on gut microbiota composition in advanced liver disease and its complications. World J. Gastroenterol. 2015, 21, 12322–12333.
- Caraceni, P.; Vargas, V.; Solà, E.; Alessandria, C.; de Wit, K.; Trebicka, J.; Watson, H. The use of rifaximin in patients with cirrhosis. Hepatology 2021, 74, 1660–1673.
- Patel VC, Lee S, McPhail MJW, et al. Rifaximin-α reduces gut-derived inflammation and mucin degradation in cirrhosis and encephalopathy: RIFSYS randomised controlled trial. J Hepatol. 2022;76(2):332-342. doi:10.1016/j.jhep.2021.09.010
- Elfert, A.; Abo Ali, L.; Soliman, S.; Ibrahim, S.; Abd-Elsalam, S. Randomized-controlled trial of rifaximin versus norfloxacin for secondary prophylaxis of spontaneous bacterial peritonitis. Eur. J. Gastroenterol. Hepatol. 2016, 28, 1450–1454.
- Lo, R.S.; Austin, A.S.; Freeman, J.G. Is there a role for probiotics in liver disease? Sci. World J. 2014, 2014, 874768.
- Wiest, R.; Chen, F.; Cadelina, G.; Groszmann, R.J.; Garcia-Tsao, G. Effect of Lactobacillus-fermented diets on bacterial translocation and intestinal flora in experimental prehepatic portal hypertension. Dig. Dis. Sci. 2003, 48, 1136–1141.
- Pande, C.; Kumar, A.; Sarin, S.K. Addition of probiotics to norfloxacin does not improve efficacy in the prevention of spontaneous bacterial peritonitis: A double-blind placebo-controlled randomized-controlled trial. Eur. J. Gastroenterol. Hepatol. 2012, 24, 831–839.
- Markowiak, P.; Śliżewska, K. Effects of Probiotics, Prebiotics, and Synbiotics on Human Health. Nutrients 2017, 9, 1021.
- Potruch, A.; Schwartz, A.; Ilan, Y. The role of bacterial translocation in sepsis: A new target for therapy. Ther. Adv. Gastroenterol. 2022, 15, 17562848221094214.
- Rose, E.C.; Odle, J.; Blikslager, A.T.; Ziegler, A.L. Probiotics, prebiotics and epithelial tight junctions: A promising approach to modulate intestinal barrier function. Int. J. Mol. Sci. 2021, 22, 6729.
- Jiang, H.; Peng, Y.; Zhang, W.; Chen, Y.; Jiang, Q.; Zhou, Y. Gut microbiome-targeted therapies in liver cirrhosis: A protocol for systematic review and meta-analysis. Syst. Rev. 2022, 11, 181.
- Zacharias, H.D.; Zacharias, A.P.; Gluud, L.L.; Morgan, M.Y. Pharmacotherapies that specifically target ammonia for the prevention and treatment of hepatic encephalopathy in adults with cirrhosis. Cochrane Database Syst. Rev. 2019, 6, CD012334.
- Macnaughtan, J.; Ranchal, I.; Soeda, J.; Sawhney, R.; Oben, J.; Davies, N.; Mookerjee, R.; Marchesi, J.; Cox, J.; Jalan, R. Oral therapy with non-absorbable carbons of controlled porosity (Yaq-001) selectively modulates stool microbiome and its function and this is associated with restoration of immune function and inflammasome activation. J. Hepatol. 2015, 62, S240.
- Ubeda, M.; Lario, M.; Munoz, L.; Borrero, M.J.; Rodriguez-Serrano, M.; Sanchez-Diaz, A.M.; Del Campo, R.; Lledó, L.; Pastor, Ó.; García-Bermejo, L.; et al. Obeticholic acid reduces bacterial translocation and inhibits intestinal inflammation in cirrhotic rats. J. Hepatol. 2016, 64, 1049–1057.
- Tsuji, Y.; Kaji, K.; Kitade, M.; Kaya, D.; Kitagawa, K.; Ozutsumi, T.; Fujinaga, Y.; Takaya, H.; Kawaratani, H.; Namisaki, T.; et al. Bile acid sequestrant, sevelamer ameliorates hepatic fibrosis with reduced overload of endogenous lipopolysaccharide in experimental nonalcoholic steatohepatitis. Microorganisms 2020, 8, 925.
- Sandhu, B.S.; Gupta, R.; Sharma, J.; Singh, J.; Murthy, N.S.; Sarin, S.K. Norfloxacin and cisapride combination decreases the incidence of spontaneous bacterial peritonitis in cirrhotic ascites. J. Gastroenterol. Hepatol. 2005, 20, 599–605.
- Pérez-Paramo, M.; Muñoz, J.; Albillos, A.; Freile, I.; Portero, F.; Santos, M.; Ortiz-Berrocal, J. Effect of propranolol on factors promoting bacterial translocation in cirrhotic rats with ascites. Hepatology 2000, 31, 43–48.
- Tranah, T.H.; Edwards, L.A.; Schnabl, B.; Shawcross, D.L. Targeting the gut-liver-immune axis to treat cirrhosis. Gut 2021, 70, 982–994.
