Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Pathology
Traumatic brain injury (TBI) is one of the most prevalent causes of morbidity in the United States and is associated with numerous chronic sequelae long after the point of injury. One of the most common long-term complaints in patients with TBI is sleep dysfunction. It is reported that alterations in melatonin follow TBI and may be linked with various sleep and circadian disorders directly (via cellular signaling) or indirectly (via free radicals and inflammatory signaling).
- traumatic brain injury
- melatonin
- insomnia
- therapeutic
1. Introduction
Traumatic brain injury (TBI) is a prominent cause of morbidity and mortality around the world, with an estimated global incidence of nearly 1/100, as 69 million individuals sustain a TBI every year [1,2]. Patients with TBI experience a complex symptom constellation, varying widely between individuals and persisting for several years after the initial injury [3,4]. Disruption of normal sleep patterns following TBI of any severity is one of the most common complaints experienced in both acute and chronic recovery phases. Estimates for prevalence vary widely, ranging anywhere from 30% to 70% [5,6,7]. Sleep quality complaints with TBI correlate strongly with mood and pain domains. They are difficult to disentangle, as they independently associate with impaired cognition, pain sensitization, and mood disorders [8,9]; they also prolong recovery after injury [10]. Considering the high prevalence and health burden of sleep disorders following TBI, interventions that optimize sleep may provide one of the greatest opportunities to improve long-term outcomes in this population.
A suitable therapeutic intervention requires a balance of safety and efficacy, and it may be most effectively utilized with an understanding of how its mechanism of action addresses underlying injury pathophysiology. Despite growing insight into the importance of sleep dysfunction following CNS injury, detailed mechanisms for the cause of these disturbances remain largely unknown as they are likely multidimensional, depending on injury patterns and individualized comorbidities. Further, the mechanism of sleep dysfunction post-TBI may differ by chronicity since the injury. Acute parenchymal disruption has been shown to be caused by a mixture of the force-based primary injury and subsequent secondary injury, which includes resultant metabolic disruption, oxidative stress, and inflammation that may pervade long after the initial injury occurred, culminating in eventual neurodegeneration [11,12]. An ideal therapeutic might mitigate one or multiple causative injury mechanisms while simultaneously promoting a high safety and efficacy profile.
Melatonin has well-established properties as a potent antioxidant that also functions as a signaling hormone, regulating sleep and circadian physiology. For example, direct changes in melatonin production, receptor concentration, and circadian rhythm function have been repeatedly observed following TBI [13,14,15,16,17,18,19]. Disruptions of endogenous melatonin signaling after TBI may partly explain some of the pathological phenotypes related to sleep, inflammation, and hormonal function. As a therapeutic, exogenous melatonin has had several challenges. A host of negative or inconclusive clinical insomnia studies [20] conflict, in part, with supportive studies in comorbid sub-populations [21,22]. There are also some studies showing safety and efficacy in the use of melatonin for enhancing reproductive health and fertility [23,24], while some animal studies suggest there might be a risk in prenatal and childhood development due to hormone signals [25,26,27] (although no human evidence of developmental harm from melatonin is known to the authors of this paper). These data, combined with a lack of federal regulation and reports of inaccurate quantification and impurities during manufacture [28], have led to its removal from clinical guidelines and recommendations for the treatment of sleep disorders. Nonetheless, clinical use continues, and certain indications, such as the use of melatonin in shifting circadian timing (e.g., for jet lag), remain widely accepted [29] due to what appears to be an acceptable safety margin and side effect profile. Some argue that the increasingly prolific use in over-the-counter supplementation as a circadian clock-shifting stimulus and a sleep aid in the general population could be cause for concern in some susceptible populations [29].
2. Primary Injury
Proposed mechanisms underlying sleep dysfunction following TBI can be subdivided by chronicity and subsequent microscopic or macroscopic effects. Acute injury mechanisms implicate acceleration-deceleration (blast and/or coup-contrecoup), resulting in axonal shearing and diffuse interruption of affiliated functional networks, theoretically including those associated with wakefulness and sleep, as shown in Figure 1 [73]. Cranial surface morphology exerts traumatic action in areas of high shear stress, such as the sphenoid ridge, inferior frontal, anterior temporal, and basal forebrain regions. These areas are rich in axonal projections mediating sleep and wakefulness, such as those from the locus coeruleus (noradrenergic pathway), the suprachiasmatic nucleus (circadian rhythm disorders), posterior hypothalamus (orexin neurons), and tuberomammillary nucleus (histaminergic pathway) [73].
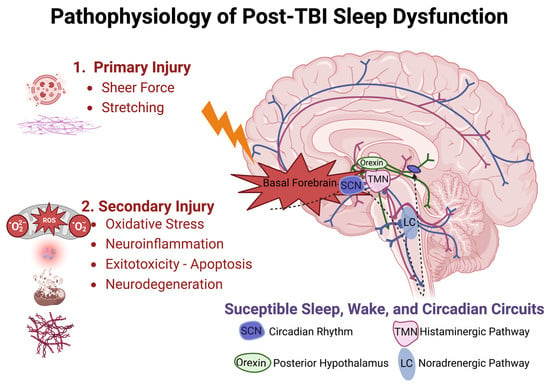
Figure 1.[1] Pathophysiologic model of traumatic brain injury and disrupted sleep-related circuitry. Injury is sustained in two phases, with primary injury likely to disrupt axonal projections near the skull base and secondary injury responsible for prolonged cellular injury owed to oxidative stress, neuroinflammation, glutamate excitotoxicity, and neurodegeneration over acute and chronic durations. Suprachiasmatic Nucleus (SCN), Tuberomammillary Nucleus (TMN), Locus Coeruleus (LC).
Delayed mechanisms inciting injury include hypoxemia, hypotension, increased intracranial pressure, seizures, and hematoma formation. Microscopic effects of cellular damage, unchecked free radical production, neuroinflammation, and biochemical excitotoxicity-related events have all been shown to disrupt normal neural function following TBI.
3. Secondary Injury
Extensive inflammatory cytokine release is observed following TBI, functioning as an innate mechanism to promote self-healing and stabilize the parenchymal microenvironment of the CNS [74,75]. However, chronic inflammation can prolong clinical recovery and predispose patients to additional deficits [36,76]. Following primary injury, mediators of inflammatory cascades are released, which in turn promote the recruitment, activation, and integration of immune cells and signaling molecules within the cerebral microenvironment, as shown in Figure 2 [75]. The inflammatory response following primary injury is a prominent catalyst for secondary insults such as ischemia, edema, hemorrhage, lipid peroxidation/free radical injury, and cell death [76,77]. Secondary injuries can prolong treatment and impair a complete, timely recovery, representing an important focus for an interventional study.
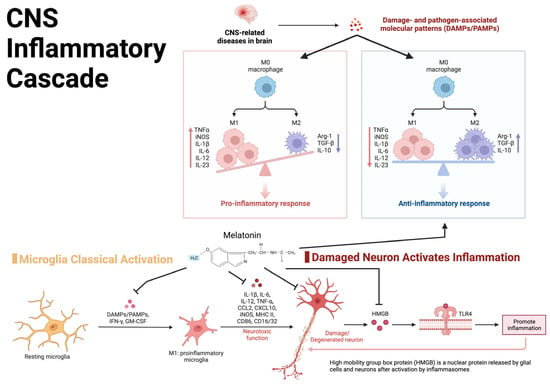
Figure 2.[1] Visual representation of the central nervous system inflammatory cascade and the inflammatory feedback loop potentially leading to chronic post-TBI symptoms.
4. Injury Severity
The inciting force which produces clinically recognized TBI can be as innocuous as head jostling, common to many recreational sports, or as complex as an explosion resulting in multiple pressure waves, lacerations, contusions, and fragmented bones. Severe TBI has been found to result in loss of function in wake-promoting tuberomammillary histaminergic systems and is associated with symptoms of daytime fatigue. A post-mortem examination of patients with severe TBI found a loss of 41% of histaminergic neurons, 29% melanin-concentrating hormone, and 21% of orexinergic neurons [78]. Cortical excitability and stimulation likely underpin excessive daytime sleepiness (EDS) and fatigue in the TBI population. The magnitude of the force is not predictive of the severity of the injury. The severity of a TBI is dependent on a multitude of factors, including the mechanism of injury, characteristics of the individual patient, such as age, previous central nervous system (CNS) injury, and predisposing conditions [79].
5. Genetic Risk
Genomic variation may also expose individuals to the risk of developing sleep dysfunction following TBI. Genetic susceptibility for developing circadian rhythm disorders following TBI has been identified, providing additional context for mechanisms related to pathophysiology and risk factor stratification [80]. The PERIOD (Per) gene family, which is a polymorphic regulator of circadian rhythm, has been implicated in delayed sleep phase syndrome and confers increased risk for shorter sleep duration following TBI, as reported by Hong et al. [81]. Heterozygous Per3 carriers were associated with a significant risk for persistent sleep dysfunction following TBI [81]. Just as the magnitude of force does not always predict injury severity, TBI severity does not predict the severity of sleep-related symptoms; whether accounting for the genetic background would improve sleep outcome prediction remains an open question.
This entry is adapted from the peer-reviewed paper 10.3390/clockssleep5020016
References
- Created with BioRender.com . BioRender. Retrieved 2023-4-24
This entry is offline, you can click here to edit this entry!
