In this review, the structure, function, absorption, and metabolism of soybean peptides are introduced brieflfly. The regulatory effects of soybean peptides on a few main chronic diseases were also reviewed, including obesity, diabetes mellitus, cardiovascular diseases (CVD), and cancer. We also addressed the shortcomings of functional research on soybean proteins and peptides in chronic diseases and the possible directions in the future.
- chronic diseases
- soybean peptides
- diabetes mellitus
- obesity
- cardiovascular diseases
- cancer
1. Introduction
With the development of urbanization and the increase in sedentary habits, chronic diseases have become a worldwide public health problem. Chronic diseases are noninfectious diseases, but not some specific diseases, with complex etiology, slow development, and long duration [1]. Chronic diseases may be caused by lifestyle, environment, diet, or genetic factors. There were 28 million people who died of chronic diseases world- wide in 1990, and this number increased to 36 million in 2008 and 39 million in 2016 [1]. More than two-thirds of the deaths worldwide are believed to be caused by chronic diseases [1]. In 2019, seven of the top ten causes of death were due to non-communicable diseases, according to the World Health Organization (WHO) [2]. At present, chronic diseases mainly include obesity, diabetes, cardiovascular diseases (CVD), and cancer, and they are key causes of premature death in humans [3]. The pathogenesis of chronic diseases is relatively complex, such as imbalances in the protease network, which can lead to malfunctions in the cellular signal network [4].
The expression of matrix metalloproteinases (MMPs) and the imbalance of the phosphoryladylinositol 3-kinase (PI3K)/AKT/major target of rapamycin (mTOR) signaling pathway may both have an impact on the development of chronic diseases such as CVD, type 2 diabetes (T2D), and cancer [4,5].
As metabolic diseases, chronic diseases are associated with metabolic syndrome (MetS). MetS is not a disease itself but a comprehensive concept, representing factors that increase the risks of individual diseases (as shown in Figure 1) [6]. It has been reported that several components of MetS led to a significant increase in the risk of chronic diseases and that the risk factors for chronic diseases and the definition of MetS partially overlap [7].
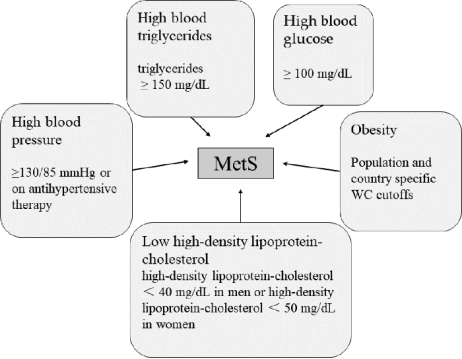
Figure 1. Main diagnosis of MetS. Three of the above five conditions are considered MetS [8].
Therefore, MetS may be a risk factor leading to the development of chronic diseases. Several diseases associated with both conditions have been identified, including obesity, T2D, CVD, and cancer [7].
Among these conditions (Figure 1), obesity is a major cause of MetS. Obesity may increase the susceptibility to insulin resistance, thus causing MetS. In 2005, the International Diabetes Federation recognized obesity as a necessary factor in the diagnosis of MetS [9], while Dr. Reaven objected to this and believed that insulin resistance might be the main cause of MetS [10]. MetS is an important risk factor for T2D and CVD (see Figure 2). With the increase in the number of patients with MetS, the number of patients with T2D and CVD also increased significantly [8].
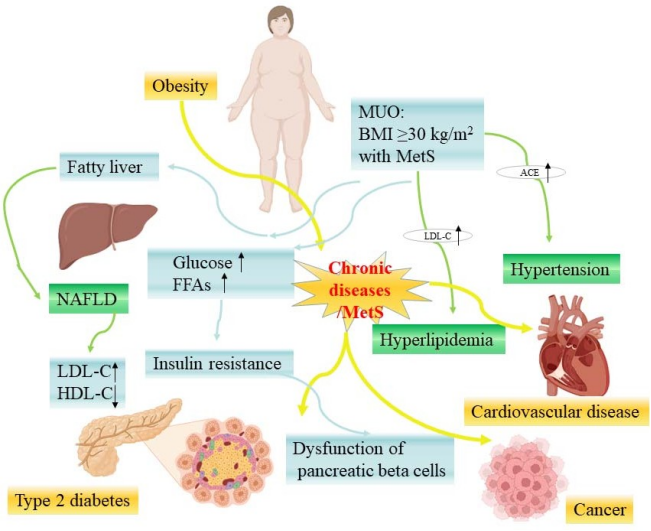
Figure 2. The relationship between chronic diseases and MetS-related diseases (some picture elements are from the BioRender). MUO—metabolic unhealthy obesity; NAFLD—nonalcoholic fatty liver disease; LDL-C—low-density lipoprotein cholesterol; HDL-C—high-density lipoprotein cholesterol; ACE—angiotensin-converting enzyme; FFAs—free fatty acids.
Obesity includes metabolic healthy obesity (MHO) and metabolic unhealthy obesity (MUO) [11], while MHO is unstable and transient, and most patients with MHO will transition to MUO stage with the accumulation of fat [12]. Morgan Mongraw Chaffin and colleagues found that MHO would develop into MUO when it exceeded a certain baseline (odds ratio [OR]: 1.60; 95% confidence interval [CI]: 1.14 to 2.25), and the risk of CVD for those with MUO increased significantly [13]. Due to the fact that obesity is the cause of heart diseases and the relationship between obesity and CVD is mediated by MetS, MetS can be regarded as a sign of obesity accumulation at the exposure threshold [13].
On the other direction, obesity can cause MetS to develop into diabetes, while nonalco- holic fatty liver disease (NAFLD), the most common metabolic liver disease, is a continuum between them [14]. In the United States, about 30% of adults have NAFLD, and 20% of them are developed by individuals with obesity [15]. In a meta-analysis of 24 studies involving 35,599 type 2 diabetic patients, the prevalence of NAFLD in ordinary diabetes patients was 59.67% but increased to 77.87% in diabetes patients with obesity [16]. MetS leads to an increase in glucose levels in the body and excessive production of free fatty acids [17], and the degree of dysfunction of pancreatic beta cells was related to the severity of MetS [18]. When pancreatic beta cells exceed a certain metabolic capacity for a long time, their quality and function will be reduced, and their metabolic function will be damaged [17].
At present, the treatments for chronic diseases include physical exercise and diet therapy, as well as drugs for related symptoms. Bioactive peptides derived from food proteins have been recognized by the industry as improving health because of their low costs and low side effects. A variety of bioactive peptides from different foods have been reported for their bioactivities, including anti-hypertension, anti-diabetes, and anti-cancer activities [19–21]. Studies have shown that increased intake of plant proteins is associated with decreased risk of obesity, CVD, diabetes, cancer, and other symptoms [21]. Soybean peptides, as one of the popular bioactive ingredients derived from soybean proteins, have been utilized in many health aspects, such as anti-obesity, anti-diabetes, anti-CVD, anti- cancer, and antioxidant activities [22].
As a traditional plant, soybean has been planted in China for nearly 5000 years [23]. The United States introduced soybeans in 1965 [24] and has now become the world’s highest soybean production country, with the production volume reaching 45% of the world’s total output [25]. Later on, the cultivation of soybeans gradually developed in other countries, and it has become a popular cash crop in the world. Proteins are the most abundant nutrient in soybean, accounting for about 40% of all nutrients, and they are a very important plant source of dietary proteins [26]. Soybean proteins contain all twenty types of amino acids, including nine essential amino acids [27,28]. Its nutritional value is equivalent to that of animal protein, and therefore, it is considered to be a full-value protein [22].
Soybean peptides are derived by the hydrolysis of soybean proteins using different proteases, and they are mixtures of oligopeptides with 3–6 amino acids and molecular weights of 300–700 Da [29]. The physiological activities of soybean peptides are determined by the size of their relative molecular weights and the sequences of amino acids [30]. Their amino acid composition and proportion are the same as those in soybean proteins, but they are easier to absorb and more stable [31]. Soy proteins and peptides have been shown to be safe and non-toxic in the past, which is important for their further utilization [32].
In this paper, we reviewed the structure, function, absorption, and metabolic characteristics of soybean peptides. We also discussed their potential effects on the regulation and improvement of chronic diseases.
2. The Effects of Soybean Peptides on Chronic Diseases
Researchers are interested in exploring peptides and protein hydrolysates as active ingredients to prevent or treat chronic diseases. As a potent bioactive with an abundant source, soybean peptides have attracted a lot of attention, and the functions of soybean peptides have been widely investigated. The functions of soybean proteins and peptides on chronic diseases, including anti-obesity, anti-diabetes, anti-CVD diseases, and anti-cancer activities, are of interest in this review (Figure 3).
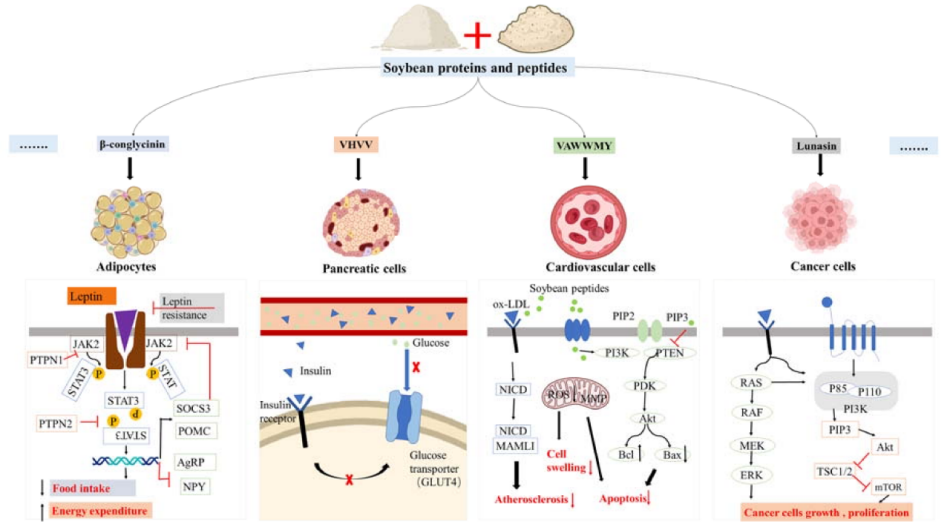
Figure 3. Partial potential mechanisms of the various activities of soybean proteins and peptides on chronic diseases (some picture elements are from the BioRender).
This entry is adapted from the peer-reviewed paper 10.3390/nu15081811
