The global increase and prevalence of inflammatory-mediated diseases have been a great menace to human welfare. Several works have demonstrated the anti-inflammatory potentials of natural polyphenolic compounds, including flavonoid derivatives (EGCG, rutin, apigenin, naringenin) and phenolic acids (GA, CA, etc.), among others (resveratrol, curcumin, etc.). In order to improve the stability and bioavailability of these natural polyphenolic compounds, their recent loading applications in both organic (liposomes, micelles, dendrimers, etc.) and inorganic (mesoporous silica, heavy metals, etc.) nanocarrier technologies are being employed.
- polyphenolic
- nanocarriers
- drug delivery
- bioavailability
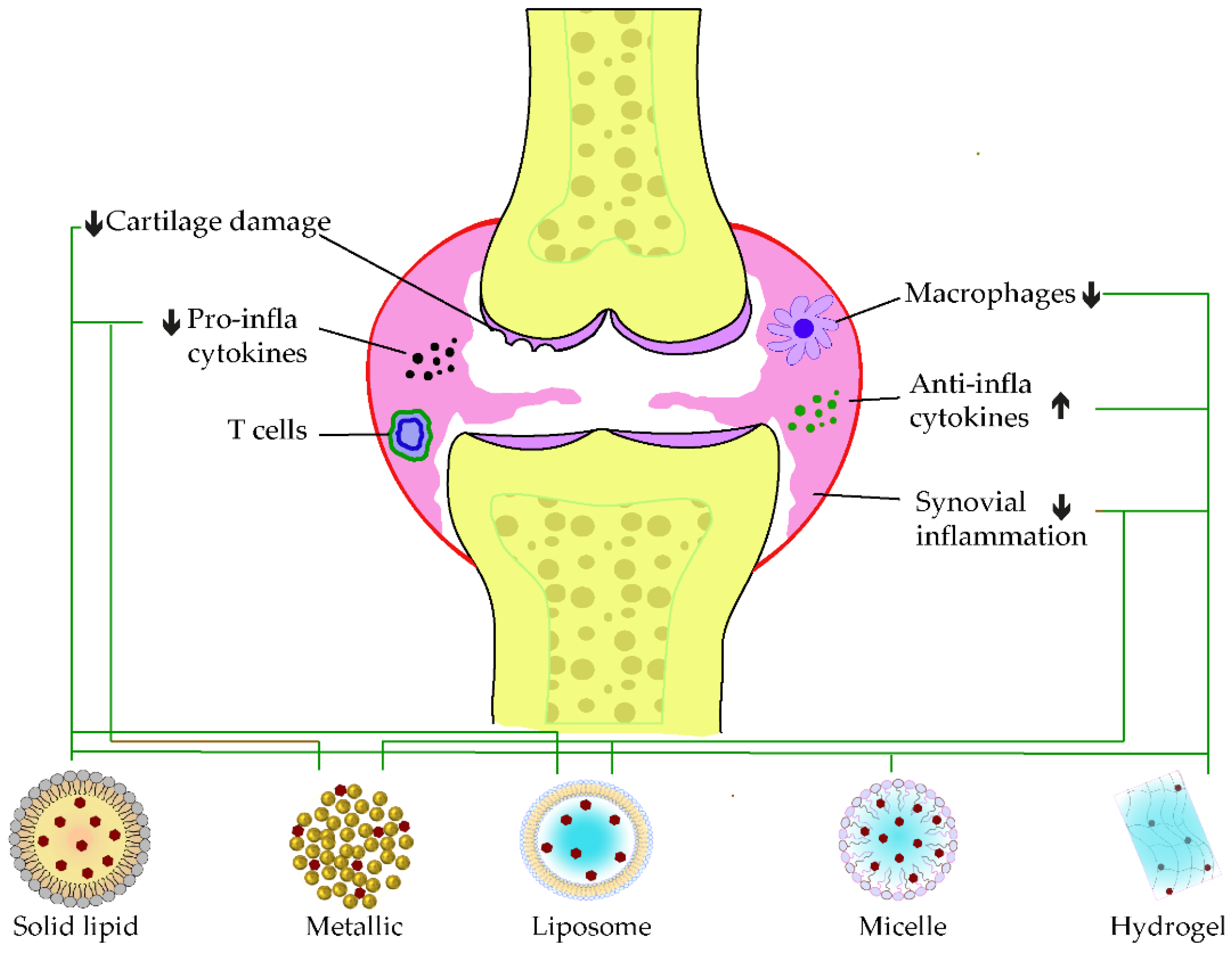
1. Polyphenolic Nano Delivery for Rheumatoid Arthritis
2. Polyphenolic Nano Delivery for Neurodegenerative Disease
3. Polyphenolic Nano Delivery for Skin Inflammation and Wound
| Phenolic Compounds |
Type of Nanocarriers (Size) |
Targets | Mechanism of Action | Ref. |
|---|---|---|---|---|
| EGCG | Polymeric nanocarrier: PEG-PLGA (176 nm) |
DNCB-induced dermatitis model | Reduces ear and skin thickness, mitigates the inflammatory cytokines releases (TNF-α, IFN-γ, IL-4, IL-6, and IL-17A), blockades necroptosis (RIP1, RIP3, and MLKL expressions), and regulates MAPK pathways (p-p38, ERK1, and ERK2) | [41] |
| EGCG | Polymeric nanocarrier: CHI-EGCG-NPs (211 nm) |
Cultured keratinocytes and IMQ-induced model | Reduces inflammatory responses and modulates psoriasis-related inflammatory cytokines | [40] |
| EGCG | Hydrogel nanocarrier: HG-Ag-EGCG (217 nm) |
Subcutaneous wound in Wistar rats | Accelerates wound properties (modulates growth factors and cytokines) | [43] |
| EGCG | Polymeric nanocarrier: EGCG-Vit C-Gelatin, chitosan (200 nm) |
Wound on STZ-induced diabetic mice | Promotes wound healing by raising collagen accumulation, promoting angiogenesis, and reducing inflammatory cell infiltrations | [42] |
| Rutin | Hydrogel nanocarrier: NC-RU-gel (447 nm) |
UV-induced BALB/c mice | Increases the skin permeability of rutin | [44] |
| Rutin | Ethosomal nanocarrier: ETOH-PL90G-H2O (112 nm) |
Keratinocyte cells (NCTC2544) and volunteer patients | Improves anti-inflammatory effect | [45] |
| Apigenin | Ethosomal nanocarrier (36 nm) |
UV-induced skin inflammation | Reduces COX-2 levels | [46] |
| Naringenin | Liposome: NAR-Polysorbate 80-Lipoid® (100 nm) |
3T3 fibroblasts and TPA-induced mice | Reduces skin inflammation | [47] |
| Naringenin | Liposome: chitosan-coated naringenin nanoemulsion (105 nm) |
Abrasion wound in rat model | Controls the delivery and ameliorates the wounds construction and skin regeneration | [48] |
| Gallic acid | Polymeric nanocarrier: Tween 80-chitosan (330 nm) |
HaCaT cell line | Reduces keratinocyte proliferation and exerts protein protection in vitro. | [50] |
| Gallic acid | Hydrogel nanocarrier | Total skin defect model | Enhance wound healing by reducing the expression of IL-6, IL-1β, and TNF-α | [52] |
| Gallic acid | Hydrogel nanocarrier: GH/GGA | Skin wounded mice | Speeds up the wound healing by scavenging the ROS and promoting tissue regeneration | [51] |
| Gallic acid | Polymeric nanocarrier: liposome, glycosome GA polyxomer (70 nm) | TPA induced mice | Improves the skin target delivery and blockades leukocytes infiltration | [49] |
| Caffeic acid | Nanofiber nanocarrier: PLGA | In vitro scratch assay | Presents better wound healing properties on human fibroblast | [54] |
| Caffeic acid | Nanofiber nanocarrier: Chitosan-PCL/CCA | NHDF-neo cell line | Improves cell attachment | [53] |
| Resveratrol | Lipid nanocarrier: Oleic acid-S75 (79 nm) |
TPA induced mice | Neutralizes the inflammatory response | [55] |
| Resveratrol | Lipid nanocarrier: DSPC/DOPE/ω3 (156 nm) |
RAW 264.7 cell line | Inhibits COX and NO productions | [56] |
| Resveratrol | Peptide-hydrogel nanocarrier: Fmoc-FFGGRGD | Rat skin damage model | Inhibits macrophage production of pro-inflammatory cytokines | [57] |
| Curcumin | Hydrogel nanocarriers: PLGA NPS in hydrogel (150 nm) |
IMQ-induced-C57/BL6 mice | Improves anti-psoriasis activity | [61] |
| Curcumin | Gelatin nanofiber mats | Rat wounded model | Improves the wounds by increasing fibroblast proliferation and migration, inhibiting macrophages, and reducing pro-inflammatory cytokines | [62] |
| Curcumin | Nanocrystal coated nanocarrier: Ch/CNC (Ag NPx/Cury) | Injured rat model | Accelerates wound closure and repairs tissues | [63] |
| Curcumin | Silica nanocarrier: CU-Si-Nps (36 nm) |
HDF fibroblast cell | Enhances fibroblast migrations | [65] |
| Curcumin | Nanostructured lipid carrier: EGF–Cur-NLC (331 nm) |
Punched wound on the skin | Accelerates wound closure | [64] |
| Curcumin | Hydrogel nanocarrier: PEG-PLA in dextran hydrogel (65 nm) |
BALB/c mice | Accelerates angiogenesis, fibroblast accumulation, and wound healing | [60] |
| Curcumin | Hydrogel nanocarrier: MPEG-PCL in CCS-OA hydrogel (nano: 40 nm) |
Injured tissue | Improves re-epithelialization of the injury | [58] |
| Curcumin | Hydrogel nanocarrier: PEG-PCL-PEG in hydrogel (micelle: 26 nm) |
Wound model | Enhances cutaneous repair, and increases collagen content and wound maturity | [59] |
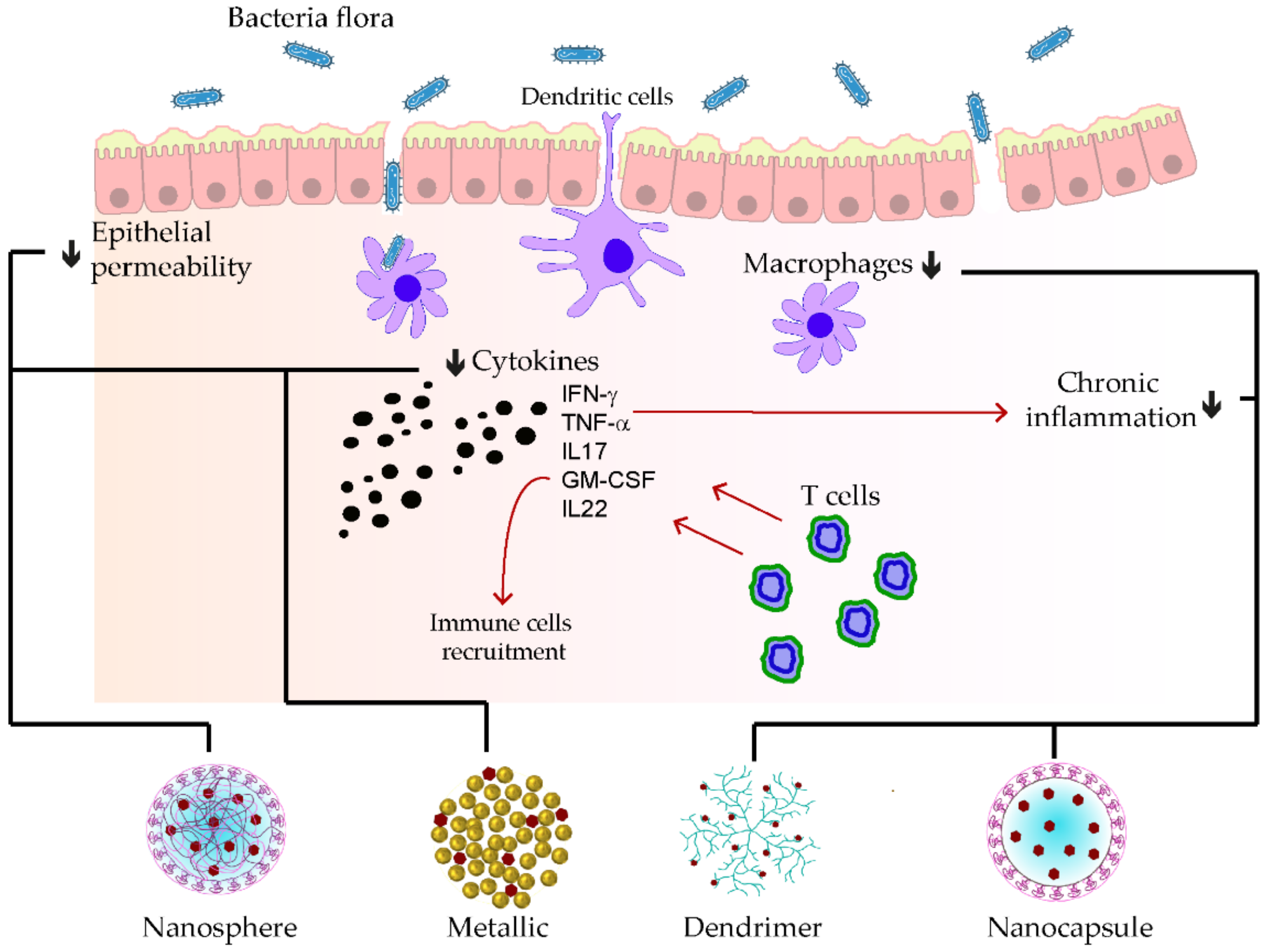
4. Polyphenolic Nano Delivery in Inflammatory Bowel Disease
5. Polyphenolic Nano Delivery for Metabolic Disorder
| Phenolic Compounds |
Type of Nanocarriers (Size) |
Targets | Mechanism of Action | Ref. |
|---|---|---|---|---|
| EGCG | Polymeric nanocarrier: EGCG-PLGA-in hydrogel (112 nm) |
SC model | Increases delivery and reduces cholesterol, LDL-cholesterol while increasing HDL | [83] |
| EGCG | Hybrid nanocarrier HG-AG-EGCG |
HFD-induced T2DM C57BL/6 | Improves wound healing in diabetes by suppressing related inflammation | [43] |
| EGCG | Protein nanocarrier: EGCG-β-Lg (22 nm) |
HFD obese mice | Lowers triglycerides amount in the model and improved glycemic homeostasis, as well as insulin sensitivity | [82] |
| Rutin | Lipid nanocarrier: Lecithin nanophytosome: (72 nm) |
STZ-induced diabetic rats | Mitigates hyperglycemia and hyperlipidemia, reduces the induced damage of the kidney, liver, and pancreas in rats | [85] |
| Rutin | Polymeric nanocarrier: ARG-EG-RU (68 nm) |
STZ-induced diabetic rats | Reduces glucose, GHb, and lipid levels, while increasing insulin amount | [84] |
| Rutin | Selenium nanocarrier: RU+Se-NPs | Sprague-Dawley rats | Upregulates SIRT-1, Nrf-2, and HO-1 and downregulates JAK-2/STAT3 pathways, as well as inflammatory markers | [86] |
| Apigenin | Polymeric nanocarrier: PEGlated-PLGA (160 nm) | Cholecystokinin- induced C57/BL6 mice | Inhibits PSC growth, promotes PSC apoptosis, reduce the expression of PSC-related inflammation | [87] |
| Naringenin | Lipid nanocarrier: NRG-Nano (98 nm) |
Methionine choline-induced mice | Improved absorption and showed protection in fatty liver | [89] |
| Naringenin | Polymeric nanocarrier: N-PLGA (129 nm) |
STZ-induced diabetic rat | Ameliorates diabetogenic (increases insulin level, and improves dyslipidemia) | [88] |
| Gallic acid | Hydrogel nanocarrier: GA-KGM | STZ-induced diabetic rats | Reduces the expression of IL-1β, TNF-α, and COX-2 | [98] |
| Gallic acid | Polymeric nanocarrier: HAP-PEG-GA-INS (396 nm) |
STZ-induced T1D rats | Reduces blood glucose level in diabetic rats due to a higher delivery of insulin | [99] |
| Caffeic acid | Lipid nanocarrier: CAPE-loaded-NL (309 nm) |
L-ornithine induced rat | Modulated Nrf2 and NF-kB signaling | [100] |
| Caffeic acid | Lipid nanocarrier: CA–PC (168 nm) |
HFD-induced hyperlipidemic model | Maintain hepatocyte structure which promotes lipid absorption | [101] |
| Resveratrol | Lipid nanocarrier: RSV-LPs (215 nm) |
Glucose/STZ-induced β- TC cell | Reduces glucose and increased insulin level | [102] |
| Resveratrol | Metallic nanocarrier: RES-Au-NPs (20 nm) |
STZ- induced diabetic rats | Overcomes blood-retinal barrier, reduces VEGF-1, TNF-α, MCP-1, ICAM-1, IL-6, and blockades of ERK1/2 signaling pathway | [93] |
| Resveratrol | Polymeric nanocarrier: RES/PEG-PPhe | Intestine of STZ-induced diabetic rats | Reduces glucose level and increases insulin level while alleviating intestine injury | [91] |
| Resveratrol | Solid lipid nanocarrier: SLN-RES (248 nm) |
STZ-induced rats | Displays hypoglycemic activity, reduces Snap 23, Stx4 and Vamp2 in insulin resistance | [92] |
| Resveratrol | Polymeric nanocarrier: RSV-PLGA-NPs (176 nm) |
OA-induced HepG2 | Promotes lipolysis and mitigates hepatocellular proliferation | [90] |
| Resveratrol | Hybrid nanocarrier: L-Rnano (90 nm) |
HFD-C57BL/6 J mice | Decreases fat mass and inflammation while improving glucose homeostasis | [94] |
| Curcumin | Polymeric nanocarrier: CU-PLA-PEG (117 nm) |
STZ-induced rat | Reduces NF-κB activation, COX-2, TGF-β, and PPARγ expressions | [96] |
| Curcumin | Polymeric nanocarrier: CoQ10-PLGA (115 nm) |
STZ-induced rat | Reduces CRP, IL-6, TNF-α, triglyceride, and total cholesterol levels in plasma. | [95] |
| Curcumin | Micelle nanocarrier: C3-CU-GRAS (12 nm) |
MetS patients for 12 weeks | Reduces the level of triglyceride and HOMA-b index | [97] |
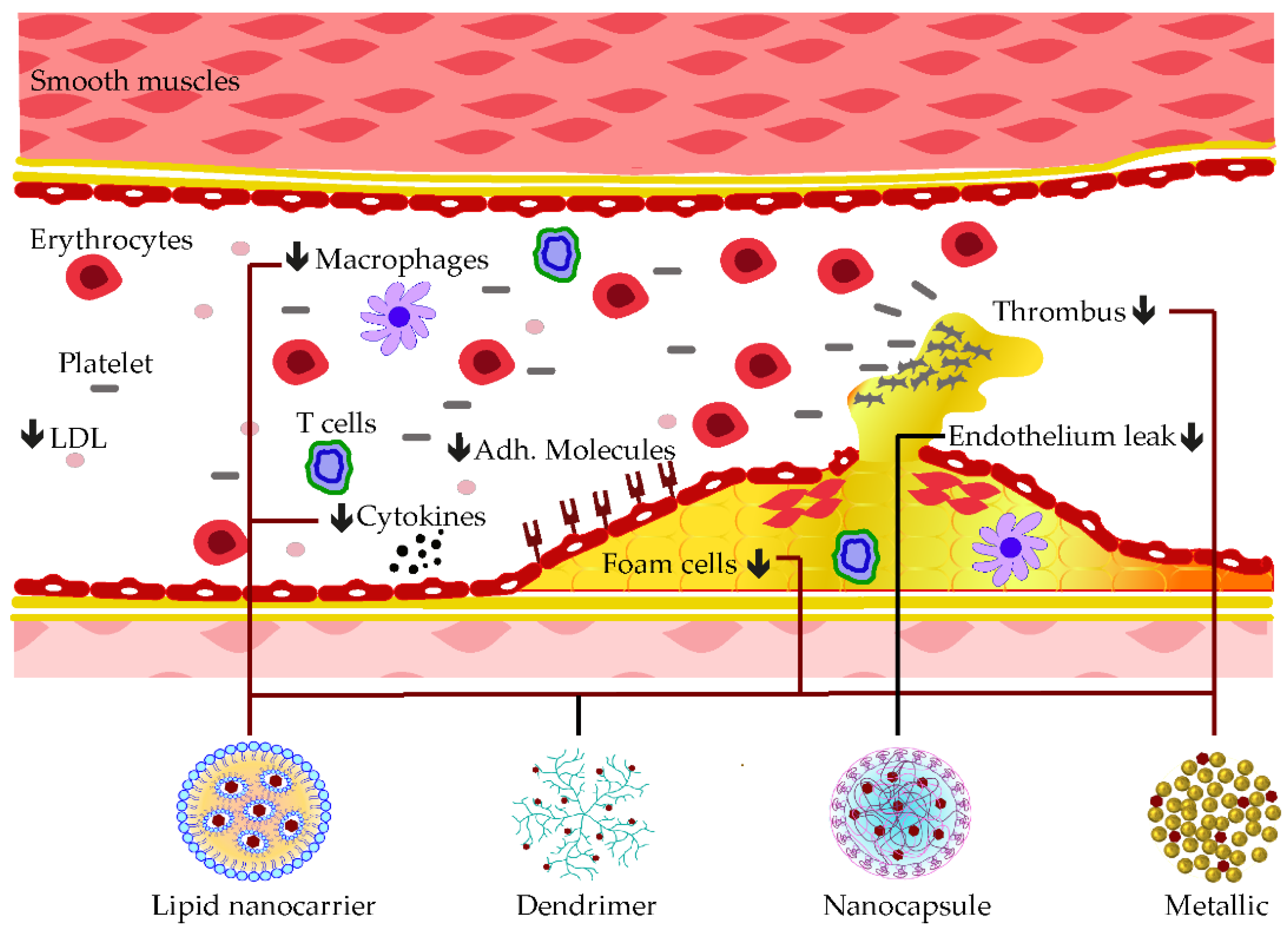
6. Polyphenolic Nano Delivery for Cardiovascular Disease
This entry is adapted from the peer-reviewed paper 10.3390/pharmaceutics15020699
References
- Jiang, Q.; Wang, X.; Huang, E.; Wang, Q.; Wen, C.; Yang, G.; Lu, L.; Cui, D. Inflammasome and Its Therapeutic Targeting in Rheumatoid Arthritis. Front. Immunol. 2022, 12, 816839.
- Kennedy, A.; Fearon, U.; Veale, D.J.; Godson, C. Macrophages in Synovial Inflammation. Front. Immunol. 2011, 2, 52.
- Macfarlane, E.; Seibel, M.J.; Zhou, H. Arthritis and the Role of Endogenous Glucocorticoids. Bone Res. 2020, 8, 33.
- Munir, A.; Muhammad, F.; Zaheer, Y.; Ali, A.; Iqbal, M.; Rehman, M.; Munir, M.U.; Akhtar, B.; Webster, T.J.; Sharif, A.; et al. Synthesis of Naringenin Loaded Lipid Based Nanocarriers and Their In-Vivo Therapeutic Potential in a Rheumatoid Arthritis Model. J. Drug Deliv. Sci. Technol. 2021, 66, 102854.
- Mohanty, S.; Sahoo, A.K.; Konkimalla, V.B.; Pal, A.; Si, S.C. Naringin in Combination with Isothiocyanates as Liposomal Formulations Potentiates the Anti-Inflammatory Activity in Different Acute and Chronic Animal Models of Rheumatoid Arthritis. ACS Omega 2020, 5, 28319–28332.
- Mohanty, S.; Konkimalla, V.B.; Pal, A.; Sharma, T.; Si, S.C. Naringin as Sustained Delivery Nanoparticles Ameliorates the Anti-Inflammatory Activity in a Freund’s Complete Adjuvant-Induced Arthritis Model. ACS Omega 2021, 6, 28630–28641.
- Zhang, G.; Sun, G.; Guan, H.; Li, M.; Liu, Y.; Tian, B.; He, Z.; Fu, Q. Naringenin Nanocrystals for Improving Anti-Rheumatoid Arthritis Activity. Asian J. Pharm. Sci. 2021, 16, 816–825.
- Chen, X.; Zhu, X.; Ma, L.; Lin, A.; Gong, Y.; Yuan, G.; Liu, J. A Core–Shell Structure QRu-PLGA-RES-DS NP Nanocomposite with Photothermal Response-Induced M2 Macrophage Polarization for Rheumatoid Arthritis Therapy. Nanoscale 2019, 11, 18209–18223.
- Kamel, R.; Abbas, H.; Shaffie, N.M. Development and Evaluation of PLA-Coated Co-Micellar Nanosystem of Resveratrol for the Intra-Articular Treatment of Arthritis. Int. J. Pharm. 2019, 569, 118560.
- Poonia, N.; Lather, V.; Kaur, B.; Kirthanashri, S.V.; Pandita, D. Optimization and Development of Methotrexate- and Resveratrol-Loaded Nanoemulsion Formulation Using Box–Behnken Design for Rheumatoid Arthritis. Assay Drug Dev. Technol. 2020, 18, 356–368.
- Cui, N.; Xu, Z.; Zhao, X.; Yuan, M.; Pan, L.; Lu, T.; Du, A.; Qin, L. In Vivo Effect of Resveratrol-Cellulose Aerogel Drug Delivery System to Relieve Inflammation on Sports Osteoarthritis. Gels 2022, 8, 544.
- Arora, R.; Kuhad, A.; Kaur, I.P.; Chopra, K. Curcumin Loaded Solid Lipid Nanoparticles Ameliorate Adjuvant-Induced Arthritis in Rats. Eur. J. Pain 2015, 19, 940–952.
- Coradini, K.; Friedrich, R.B.; Fonseca, F.N.; Vencato, M.S.; Andrade, D.F.; Oliveira, C.M.; Battistel, A.P.; Guterres, S.S.; da Rocha, M.I.U.M.; Pohlmann, A.R.; et al. A Novel Approach to Arthritis Treatment Based on Resveratrol and Curcumin Co-Encapsulated in Lipid-Core Nanocapsules: In Vivo Studies. Eur. J. Pharm. Sci. 2015, 78, 163–170.
- Yan, F.; Li, H.; Zhong, Z.; Zhou, M.; Lin, Y.; Tang, C.; Li, C. Co-Delivery of Prednisolone and Curcumin in Human Serum Albumin Nanoparticles for Effective Treatment of Rheumatoid Arthritis. Int. J. Nanomed. 2019, 14, 9113–9125.
- Naz, Z.; Ahmad, F.J. Curcumin-Loaded Colloidal Carrier System: Formulation Optimization, Mechanistic Insight, Ex Vivo and in Vivo Evaluation. Int. J. Nanomed. 2015, 10, 4293–4307.
- Dewangan, A.K.; Perumal, Y.; Pavurala, N.; Chopra, K.; Mazumder, S. Preparation, Characterization and Anti-Inflammatory Effects of Curcumin Loaded Carboxymethyl Cellulose Acetate Butyrate Nanoparticles on Adjuvant Induced Arthritis in Rats. J. Drug Deliv. Sci. Tech. 2017, 41, 269–279.
- Fan, Z.; Li, J.; Liu, J.; Jiao, H.; Liu, B. Anti-Inflammation and Joint Lubrication Dual Effects of a Novel Hyaluronic Acid/Curcumin Nanomicelle Improve the Efficacy of Rheumatoid Arthritis Therapy. ACS Appl. Mater. Interfaces 2018, 10, 23595–23604.
- Kang, C.; Jung, E.; Hyeon, H.; Seon, S.; Lee, D. Acid-Activatable Polymeric Curcumin Nanoparticles as Therapeutic Agents for Osteoarthritis. Nanomedicine 2020, 23, 102104.
- Chamani, S.; Bianconi, V.; Tasbandi, A.; Pirro, M.; Barreto, G.E.; Jamialahmadi, T.; Sahebkar, A. Resolution of Inflammation in Neurodegenerative Diseases: The Role of Resolvins. Mediat. Inflamm. 2020, 2020, e3267172.
- Wang, R.-X.; Zhou, M.; Ma, H.-L.; Qiao, Y.-B.; Li, Q.-S. The Role of Chronic Inflammation in Various Diseases and Anti-Inflammatory Therapies Containing Natural Products. Chem. Med. Chem. 2021, 16, 1576–1592.
- Forloni, G.; La Vitola, P.; Cerovic, M.; Balducci, C. Inflammation and Parkinson’s Disease Pathogenesis: Mechanisms and Therapeutic Insight. Prog. Mol. Biol. Transl. Sci. 2021, 177, 175–202.
- Singh, N.A.; Bhardwaj, V.; Ravi, C.; Ramesh, N.; Mandal, A.K.A.; Khan, Z.A. EGCG Nanoparticles Attenuate Aluminum Chloride Induced Neurobehavioral Deficits, Beta Amyloid and Tau Pathology in a Rat Model of Alzheimer’s Disease. Front. Aging Neurosci. 2018, 10, 244.
- Cano, A.; Ettcheto, M.; Chang, J.-H.; Barroso, E.; Espina, M.; Kühne, B.A.; Barenys, M.; Auladell, C.; Folch, J.; Souto, E.B.; et al. Dual-Drug Loaded Nanoparticles of Epigallocatechin-3-Gallate (EGCG)/Ascorbic Acid Enhance Therapeutic Efficacy of EGCG in a APPswe/PS1dE9 Alzheimer’s Disease Mice Model. J. Control. Release 2019, 301, 62–75.
- Lv, L.; Yang, F.; Li, H.; Yuan, J. Brain-Targeted Co-Delivery of β-Amyloid Converting Enzyme 1 ShRNA and Epigallocatechin-3-Gallate by Multifunctional Nanocarriers for Alzheimer’s Disease Treatment. IUBMB Life 2020, 72, 1819–1829.
- Li, Y.; Chen, Z.; Lu, Z.; Yang, Q.; Liu, L.; Jiang, Z.; Zhang, L.; Zhang, X.; Qing, H. “Cell-Addictive” Dual-Target Traceable Nanodrug for Parkinson’s Disease Treatment via Flotillins Pathway. Theranostics 2018, 8, 5469–5481.
- Zhang, J.; Zhou, X.; Yu, Q.; Yang, L.; Sun, D.; Zhou, Y.; Liu, J. Epigallocatechin-3-Gallate (EGCG)-Stabilized Selenium Nanoparticles Coated with Tet-1 Peptide To Reduce Amyloid-β Aggregation and Cytotoxicity. ACS Appl. Mater. Interfaces 2014, 6, 8475–8487.
- Wang, Y.; Luo, W.; Lin, F.; Liu, W.; Gu, R. Epigallocatechin-3-Gallate Selenium Nanoparticles for Neuroprotection by Scavenging Reactive Oxygen Species and Reducing Inflammation. Front. Bioeng. Biotechnol. 2022, 10, 989602.
- Pandian, S.R.K.; Pavadai, P.; Vellaisamy, S.; Ravishankar, V.; Palanisamy, P.; Sundar, L.M.; Chandramohan, V.; Sankaranarayanan, M.; Panneerselvam, T.; Kunjiappan, S. Formulation and Evaluation of Rutin-Loaded Solid Lipid Nanoparticles for the Treatment of Brain Tumor. Naunyn Schmiedebergs Arch. Pharmacol. 2021, 394, 735–749.
- Ahmad, H.; Arya, A.; Agrawal, S.; Mall, P.; Samuel, S.S.; Sharma, K.; Singh, P.K.; Singh, S.K.; Valicherla, G.R.; Mitra, K.; et al. Rutin Phospholipid Complexes Confer Neuro-Protection in Ischemic-Stroke Rats. RSC Adv. 2016, 6, 96445–96454.
- Hu, B.; Dai, F.; Fan, Z.; Ma, G.; Tang, Q.; Zhang, X. Nanotheranostics: Congo Red/Rutin-MNPs with Enhanced Magnetic Resonance Imaging and H2O2-Responsive Therapy of Alzheimer’s Disease in APPswe/PS1dE9 Transgenic Mice. Adv. Mat. 2015, 27, 5499–5505.
- Rahman, M.; Kumar, V. Apigenin Loaded Phospholipid Based Nanoemulsion in Therapeutics of Parkinson’s Disease via Attenuation of Oxidative Stress and Upregulation of Dopamine. J. Neur. Sci. 2019, 405, 247.
- Md, S.; Gan, S.Y.; Haw, Y.H.; Ho, C.L.; Wong, S.; Choudhury, H. In Vitro Neuroprotective Effects of Naringenin Nanoemulsion against β-Amyloid Toxicity through the Regulation of Amyloidogenesis and Tau Phosphorylation. Int. J. Biol. Macromol. 2018, 118, 1211–1219.
- Gaba, B.; Khan, T.; Haider, M.F.; Alam, T.; Baboota, S.; Parvez, S.; Ali, J. Vitamin E Loaded Naringenin Nanoemulsion via Intranasal Delivery for the Management of Oxidative Stress in a 6-OHDA Parkinson’s Disease Model. Biomed. Res. Int. 2019, 2019, e2382563.
- Ahmad, A.; Fauzia, E.; Kumar, M.; Mishra, R.K.; Kumar, A.; Khan, M.A.; Raza, S.S.; Khan, R. Gelatin-Coated Polycaprolactone Nanoparticle-Mediated Naringenin Delivery Rescue Human Mesenchymal Stem Cells from Oxygen Glucose Deprivation-Induced Inflammatory Stress. ACS Biomater. Sci. Eng. 2019, 5, 683–695.
- Saalbach, A.; Kunz, M. Impact of Chronic Inflammation in Psoriasis on Bone Metabolism. Front. Immunol. 2022, 13, 925503.
- Tashiro, T.; Sawada, Y. Psoriasis and Systemic Inflammatory Disorders. Int. J. Mol. Sci. 2022, 23, 4457.
- Yang, S.-C.; Alalaiwe, A.; Lin, Z.-C.; Lin, Y.-C.; Aljuffali, I.A.; Fang, J.-Y. Anti-Inflammatory MicroRNAs for Treating Inflammatory Skin Diseases. Biomolecules 2022, 12, 1072.
- Abdel-Mottaleb, M.M.; Try, C.; Pellequer, Y.; Lamprecht, A. Nanomedicine Strategies for Targeting Skin Inflammation. Nanomedicine 2014, 9, 1727–1743.
- Yang, G.; Seok, J.K.; Kang, H.C.; Cho, Y.-Y.; Lee, H.S.; Lee, J.Y. Skin Barrier Abnormalities and Immune Dysfunction in Atopic Dermatitis. Int. J. Mol. Sci. 2020, 21, 2867.
- Chamcheu, J.C.; Siddiqui, I.A.; Adhami, V.M.; Esnault, S.; Bharali, D.J.; Babatunde, A.S.; Adame, S.; Massey, R.J.; Wood, G.S.; Longley, B.J.; et al. Chitosan-Based Nanoformulated (−)-Epigallocatechin-3-Gallate (EGCG) Modulates Human Keratinocyte-Induced Responses and Alleviates Imiquimod-Induced Murine Psoriasiform Dermatitis. Int. J Nanomed. 2018, 13, 4189–4206.
- Han, M.; Wang, X.; Wang, J.; Lang, D.; Xia, X.; Jia, Y.; Chen, Y. Ameliorative Effects of Epigallocatechin-3-Gallate Nanoparticles on 2,4-Dinitrochlorobenzene Induced Atopic Dermatitis: A Potential Mechanism of Inflammation-Related Necroptosis. Front. Nutr. 2022, 9, 953646.
- Sun, M.; Xie, Q.; Cai, X.; Liu, Z.; Wang, Y.; Dong, X.; Xu, Y. Preparation and Characterization of Epigallocatechin Gallate, Ascorbic Acid, Gelatin, Chitosan Nanoparticles and Their Beneficial Effect on Wound Healing of Diabetic Mice. Int. J. Biol. Macromol. 2020, 148, 777–784.
- Kar, A.K.; Singh, A.; Dhiman, N.; Purohit, M.P.; Jagdale, P.; Kamthan, M.; Singh, D.; Kumar, M.; Ghosh, D.; Patnaik, S. Polymer-Assisted In Situ Synthesis of Silver Nanoparticles with Epigallocatechin Gallate (EGCG) Impregnated Wound Patch Potentiate Controlled Inflammatory Responses for Brisk Wound Healing. Int. J. Nanomed. 2019, 14, 9837–9854.
- Li, J.; Ni, W.; Aisha, M.; Zhang, J.; Sun, M. A Rutin Nanocrystal Gel as an Effective Dermal Delivery System for Enhanced Anti-Photoaging Application. Drug. Dev. Ind. Pharm. 2021, 47, 429–439.
- Cristiano, M.C.; Barone, A.; Mancuso, A.; Torella, D.; Paolino, D. Rutin-Loaded Nanovesicles for Improved Stability and Enhanced Topical Efficacy of Natural Compound. J. Funct. Biomater. 2021, 12, 74.
- Shen, L.-N.; Zhang, Y.-T.; Wang, Q.; Xu, L.; Feng, N.-P. Enhanced in Vitro and in Vivo Skin Deposition of Apigenin Delivered Using Ethosomes. Int. J. Pharm. 2014, 460, 280–288.
- Pleguezuelos-Villa, M.; Mir-Palomo, S.; Díez-Sales, O.; Buso, M.A.O.V.; Sauri, A.R.; Nácher, A. A Novel Ultradeformable Liposomes of Naringin for Anti-Inflammatory Therapy. Colloids Surf. B Biointerfaces 2018, 162, 265–270.
- Akrawi, S.H.; Gorain, B.; Nair, A.B.; Choudhury, H.; Pandey, M.; Shah, J.N.; Venugopala, K.N. Development and Optimization of Naringenin-Loaded Chitosan-Coated Nanoemulsion for Topical Therapy in Wound Healing. Pharmaceutics 2020, 12, 893.
- Caddeo, C.; Manca, M.L.; Matos, M.; Gutierrez, G.; Díez-Sales, O.; Peris, J.E.; Usach, I.; Fernàndez-Busquets, X.; Fadda, A.M.; Manconi, M. Functional Response of Novel Bioprotective Poloxamer-Structured Vesicles on Inflamed Skin. Nanomedicine 2017, 13, 1127–1136.
- Shandil, A.; Yadav, M.; Sharma, N.; Nagpal, K.; Jindal, D.K.; Deep, A.; Kumar, S. Targeting Keratinocyte Hyperproliferation, Inflammation, Oxidative Species and Microbial Infection by Biological Macromolecule-Based Chitosan Nanoparticle-Mediated Gallic Acid–Rutin Combination for the Treatment of Psoriasis. Polym. Bull. 2020, 77, 4713–4738.
- Thi, P.L.; Lee, Y.; Tran, D.L.; Thi, T.T.H.; Kang, J.I.; Park, K.M.; Park, K.D. In Situ Forming and Reactive Oxygen Species-Scavenging Gelatin Hydrogels for Enhancing Wound Healing Efficacy. Acta Biomater. 2020, 103, 142–152.
- Wang, X.-C.; Huang, H.-B.; Gong, W.; He, W.-Y.; Li, X.; Xu, Y.; Gong, X.-J.; Hu, J.-N. Resveratrol Triggered the Quick Self-Assembly of Gallic Acid into Therapeutic Hydrogels for Healing of Bacterially Infected Wounds. Biomacromolecules 2022, 23, 1680–1692.
- Oh, G.-W.; Ko, S.-C.; Je, J.-Y.; Kim, Y.-M.; Oh, J.; Jung, W.-K. Fabrication, Characterization and Determination of Biological Activities of Poly(ε-Caprolactone)/Chitosan-Caffeic Acid Composite Fibrous Mat for Wound Dressing Application. Int. J. Biol. Macromol. 2016, 93, 1549–1558.
- Kaya, S.; Yilmaz, D.E.; Akmayan, I.; Egri, O.; Arasoglu, T.; Derman, S. Caffeic Acid Phenethyl Ester Loaded Electrospun Nanofibers for Wound Dressing Application. J. Pharm. Sci. 2022, 111, 734–742.
- Caddeo, C.; Nacher, A.; Vassallo, A.; Armentano, M.F.; Pons, R.; Fernàndez-Busquets, X.; Carbone, C.; Valenti, D.; Fadda, A.M.; Manconi, M. Effect of Quercetin and Resveratrol Co-Incorporated in Liposomes against Inflammatory/Oxidative Response Associated with Skin Cancer. Int. J. Pharm. 2016, 513, 153–163.
- Caldas, A.R.; Catita, J.; Machado, R.; Ribeiro, A.; Cerqueira, F.; Horta, B.; Medeiros, R.; Lúcio, M.; Lopes, C.M. Omega-3- and Resveratrol-Loaded Lipid Nanosystems for Potential Use as Topical Formulations in Autoimmune, Inflammatory, and Cancerous Skin Diseases. Pharmaceutics 2021, 13, 1202.
- Zhao, C.-C.; Zhu, L.; Wu, Z.; Yang, R.; Xu, N.; Liang, L. Resveratrol-Loaded Peptide-Hydrogels Inhibit Scar Formation in Wound Healing through Suppressing Inflammation. Regen. Biomater. 2020, 7, 99–107.
- Li, X.; Chen, S.; Zhang, B.; Li, M.; Diao, K.; Zhang, Z.; Li, J.; Xu, Y.; Wang, X.; Chen, H. In Situ Injectable Nano-Composite Hydrogel Composed of Curcumin, N,O-Carboxymethyl Chitosan and Oxidized Alginate for Wound Healing Application. Int. J. Pharm. 2012, 437, 110–119.
- Gong, C.; Wu, Q.; Wang, Y.; Zhang, D.; Luo, F.; Zhao, X.; Wei, Y.; Qian, Z. A Biodegradable Hydrogel System Containing Curcumin Encapsulated in Micelles for Cutaneous Wound Healing. Biomaterials 2013, 34, 6377–6387.
- Alibolandi, M.; Mohammadi, M.; Taghdisi, S.M.; Abnous, K.; Ramezani, M. Synthesis and Preparation of Biodegradable Hybrid Dextran Hydrogel Incorporated with Biodegradable Curcumin Nanomicelles for Full Thickness Wound Healing. Int. J. Pharm. 2017, 532, 466–477.
- Sun, L.; Liu, Z.; Wang, L.; Cun, D.; Tong, H.H.Y.; Yan, R.; Chen, X.; Wang, R.; Zheng, Y. Enhanced Topical Penetration, System Exposure and Anti-Psoriasis Activity of Two Particle-Sized, Curcumin-Loaded PLGA Nanoparticles in Hydrogel. J. Control. Release 2017, 254, 44–54.
- Dai, X.; Liu, J.; Zheng, H.; Wichmann, J.; Hopfner, U.; Sudhop, S.; Prein, C.; Shen, Y.; Machens, H.-G.; Schilling, A.F. Nano-Formulated Curcumin Accelerates Acute Wound Healing through Dkk-1-Mediated Fibroblast Mobilization and MCP-1-Mediated Anti-Inflammation. NPG Asia Mater. 2017, 9, e368.
- Bajpai, S.K.; Ahuja, S.; Chand, N.; Bajpai, M. Nano Cellulose Dispersed Chitosan Film with Ag NPs/Curcumin: An in Vivo Study on Albino Rats for Wound Dressing. Int. J. Biol. Macromol. 2017, 104, 1012–1019.
- Lee, H.-J.; Jeong, M.; Na, Y.-G.; Kim, S.-J.; Lee, H.-K.; Cho, C.-W. An EGF- and Curcumin-Co-Encapsulated Nanostructured Lipid Carrier Accelerates Chronic-Wound Healing in Diabetic Rats. Molecules 2020, 25, 4610.
- Mirzahosseinipour, M.; Khorsandi, K.; Hosseinzadeh, R.; Ghazaeian, M.; Shahidi, F.K. Antimicrobial Photodynamic and Wound Healing Activity of Curcumin Encapsulated in Silica Nanoparticles. Photodiagnosis Photodyn. Ther. 2020, 29, 101639.
- Graham, D.B.; Xavier, R.J. Pathway Paradigms Revealed from the Genetics of Inflammatory Bowel Disease. Nature 2020, 578, 527–539.
- Papoutsopoulou, S.; Burkitt, M.D.; Bergey, F.; England, H.; Hough, R.; Schmidt, L.; Spiller, D.G.; White, M.H.R.; Paszek, P.; Jackson, D.A.; et al. Macrophage-Specific NF-ΚB Activation Dynamics Can Segregate Inflammatory Bowel Disease Patients. Front. Immunol. 2019, 10, 2168.
- Haep, L.; Britzen-Laurent, N.; Weber, T.G.; Naschberger, E.; Schaefer, A.; Kremmer, E.; Foersch, S.; Vieth, M.; Scheuer, W.; Wirtz, S.; et al. Interferon Gamma Counteracts the Angiogenic Switch and Induces Vascular Permeability in Dextran Sulfate Sodium Colitis in Mice. Inflamm. Bowel. Dis. 2015, 21, 2360–2371.
- Jovani, M.; Fiorino, G.; Danese, S. Anti-IL-13 in Inflammatory Bowel Disease: From the Bench to the Bedside. Curr. Drug. Targets 2013, 14, 1444–1452.
- Guo, Z.; Bai, G.; Zhan, X.; Zhuo, K.; Wang, J.; Wang, Y. Supramolecular Vector/Drug Coassemblies of Polyglycerol Dendrons and Rutin Enhance the PH Response. Langmuir 2022, 38, 3392–3402.
- Lv, F.; Zhang, Y.; Peng, Q.; Zhao, X.; Hu, D.; Wen, J.; Liu, K.; Li, R.; Wang, K.; Sun, J. Apigenin-Mn(II) Loaded Hyaluronic Acid Nanoparticles for Ulcerative Colitis Therapy in Mice. Front. Chem. 2022, 10, 969962.
- Pujara, N.; Wong, K.Y.; Qu, Z.; Wang, R.; Moniruzzaman, M.; Rewatkar, P.; Kumeria, T.; Ross, B.P.; McGuckin, M.; Popat, A. Oral Delivery of β-Lactoglobulin-Nanosphere-Encapsulated Resveratrol Alleviates Inflammation in Winnie Mice with Spontaneous Ulcerative Colitis. Mol. Pharm. 2021, 18, 627–640.
- Siu, F.Y.; Ye, S.; Lin, H.; Li, S. Galactosylated PLGA Nanoparticles for the Oral Delivery of Resveratrol: Enhanced Bioavailability and in Vitro Anti-Inflammatory Activity. Int. J. Nanomed. 2018, 13, 4133–4144.
- Rachmawati, H.; Pradana, A.T.; Safitri, D.; Adnyana, I.K. Multiple Functions of D-α-Tocopherol Polyethylene Glycol 1000 Succinate (TPGS) as Curcumin Nanoparticle Stabilizer: In Vivo Kinetic Profile and Anti-Ulcerative Colitis Analysis in Animal Model. Pharmaceutics 2017, 9, 24.
- Oshi, M.A.; Lee, J.; Naeem, M.; Hasan, N.; Kim, J.; Kim, H.J.; Lee, E.H.; Jung, Y.; Yoo, J.-W. Curcumin Nanocrystal/PH-Responsive Polyelectrolyte Multilayer Core–Shell Nanoparticles for Inflammation-Targeted Alleviation of Ulcerative Colitis. Biomacromolecules 2020, 21, 3571–3581.
- Kelly, T.; Yang, W.; Chen, C.-S.; Reynolds, K.; He, J. Global Burden of Obesity in 2005 and Projections to 2030. Int. J. Obes. 2008, 32, 1431–1437.
- Tsalamandris, S.; Antonopoulos, A.S.; Oikonomou, E.; Papamikroulis, G.-A.; Vogiatzi, G.; Papaioannou, S.; Deftereos, S.; Tousoulis, D. The Role of Inflammation in Diabetes: Current Concepts and Future Perspectives. Eur. Cardiol. 2019, 14, 50–59.
- Feuerer, M.; Shen, Y.; Littman, D.R.; Benoist, C.; Mathis, D. How Punctual Ablation of Regulatory T Cells Unleashes an Autoimmune Lesion within the Pancreatic Islets. Immunity 2009, 31, 654–664.
- Laveti, D.; Kumar, M.; Hemalatha, R.; Sistla, R.; Naidu, V.G.M.; Talla, V.; Verma, V.; Kaur, N.; Nagpal, R. Anti-Inflammatory Treatments for Chronic Diseases: A Review. Inflamm. Allergy Drug Targets. 2013, 12, 349–361.
- Divella, R.; Gadaleta Caldarola, G.; Mazzocca, A. Chronic Inflammation in Obesity and Cancer Cachexia. J. Clin. Med. 2022, 11, 2191.
- Shoelson, S.E.; Herrero, L.; Naaz, A. Obesity, Inflammation, and Insulin Resistance. Gastroenterology 2007, 132, 2169–2180.
- Zagury, Y.; Chen, S.; Edelman, R.; Karnieli, E.; Livney, Y.D. β-Lactoglobulin Delivery System for Enhancing EGCG Biological Efficacy in HFD Obesity Mice Model. J. Funct. Foods 2019, 59, 362–370.
- Zhang, X.-Z.; Guan, J.; Cai, S.-L.; Du, Q.; Guo, M.-L. Polymeric In Situ Hydrogel Implant of Epigallocatechin Gallate (EGCG) for Prolonged and Improved Antihyperlipidemic and Anti-Obesity Activity: Preparation and Characterization. J. Biomater. Tissue Eng. 2015, 5, 813–817.
- Bhattacherjee, A.; Chakraborti, A.S. Argpyrimidine-Tagged Rutin-Encapsulated Biocompatible (Ethylene Glycol Dimers) Nanoparticles: Application for Targeted Drug Delivery in Experimental Diabetes (Part 2). Int. J. Pharm. 2017, 528, 8–17.
- Amjadi, S.; Shahnaz, F.; Shokouhi, B.; Azarmi, Y.; Siahi-Shadbad, M.; Ghanbarzadeh, S.; Kouhsoltani, M.; Ebrahimi, A.; Hamishehkar, H. Nanophytosomes for Enhancement of Rutin Efficacy in Oral Administration for Diabetes Treatment in Streptozotocin-Induced Diabetic Rats. Int. J. Pharm. 2021, 610, 121208.
- Zaghloul, R.A.; Abdelghany, A.M.; Samra, Y.A. Rutin and Selenium Nanoparticles Protected against STZ-Induced Diabetic Nephropathy in Rats through Downregulating Jak-2/Stat3 Pathway and Upregulating Nrf-2/HO-1 Pathway. Eur. J. Pharmacol. 2022, 933, 175289.
- Feng, W.; Guo, H.; Xue, T.; Wang, X.; Tang, C.; Ying, B.; Gong, H.; Cui, G. Anti-Inflammation and Anti-Fibrosis with PEGylated, Apigenin Loaded PLGA Nanoparticles in Chronic Pancreatitis Disease. RSC Adv. 2015, 5, 83628–83635.
- Maity, S.; Chakraborti, A.S. Formulation, Physico-Chemical Characterization and Antidiabetic Potential of Naringenin-Loaded Poly D, L Lactide-Co-Glycolide (N-PLGA) Nanoparticles. Eur. Polymer. J. 2020, 134, 109818.
- Chen, C.; Jie, X.; Ou, Y.; Cao, Y.; Xu, L.; Wang, Y.; Qi, R. Nanoliposome Improves Inhibitory Effects of Naringenin on Nonalcoholic Fatty Liver Disease in Mice. Nanomedicine 2017, 12, 1791–1800.
- Wan, S.; Zhang, L.; Quan, Y.; Wei, K. Resveratrol-Loaded PLGA Nanoparticles: Enhanced Stability, Solubility and Bioactivity of Resveratrol for Non-Alcoholic Fatty Liver Disease Therapy. R. Soc. Open Sci. 2018, 5, 181457.
- Wang, Z.; Yan, Y.; Wang, Y.; Tong, F. The Interaction between CSE/H2S and the INOS/NO-Mediated Resveratrol/Poly(Ethylene Glycol)-Poly(Phenylalanine) Complex Alleviates Intestinal Ischemia/Reperfusion Injuries in Diabetic Rats. Biomed. Pharmacother. 2019, 112, 108736.
- Mohseni, R.; ArabSadeghabadi, Z.; Ziamajidi, N.; Abbasalipourkabir, R.; RezaeiFarimani, A. Oral Administration of Resveratrol-Loaded Solid Lipid Nanoparticle Improves Insulin Resistance Through Targeting Expression of SNARE Proteins in Adipose and Muscle Tissue in Rats with Type 2 Diabetes. Nanoscale Res. Lett. 2019, 14, 227.
- Dong, Y.; Wan, G.; Yan, P.; Qian, C.; Li, F.; Peng, G. Fabrication of Resveratrol Coated Gold Nanoparticles and Investigation of Their Effect on Diabetic Retinopathy in Streptozotocin Induced Diabetic Rats. J. Photochem. Photobiol. B 2019, 195, 51–57.
- Zu, Y.; Zhao, L.; Hao, L.; Mechref, Y.; Zabet-Moghaddam, M.; Keyel, P.A.; Abbasi, M.; Wu, D.; Dawson, J.A.; Zhang, R.; et al. Browning White Adipose Tissue Using Adipose Stromal Cell-Targeted Resveratrol-Loaded Nanoparticles for Combating Obesity. J. Control. Release 2021, 333, 339–351.
- Devadasu, V.R.; Wadsworth, R.M.; Kumar, M.N.V.R. Protective Effects of Nanoparticulate Coenzyme Q10 and Curcumin on Inflammatory Markers and Lipid Metabolism in Streptozotocin-Induced Diabetic Rats: A Possible Remedy to Diabetic Complications. Drug Deliv. Transl. Res. 2011, 1, 448–455.
- El-Naggar, M.E.; Al-Joufi, F.; Anwar, M.; Attia, M.F.; El-Bana, M.A. Curcumin-Loaded PLA-PEG Copolymer Nanoparticles for Treatment of Liver Inflammation in Streptozotocin-Induced Diabetic Rats. Colloids Surf. B Biointerfaces 2019, 177, 389–398.
- Bateni, Z.; Rahimi, H.R.; Hedayati, M.; Afsharian, S.; Goudarzi, R.; Sohrab, G. The Effects of Nano-Curcumin Supplementation on Glycemic Control, Blood Pressure, Lipid Profile, and Insulin Resistance in Patients with the Metabolic Syndrome: A Randomized, Double-Blind Clinical Trial. Phytother. Res. 2021, 35, 3945–3953.
- Hou, Y.; Huang, H.; Gong, W.; Wang, R.; He, W.; Wang, X.; Hu, J. Co-Assembling of Natural Drug-Food Homologous Molecule into Composite Hydrogel for Accelerating Diabetic Wound Healing. Biomat. Adv. 2022, 140, 213034.
- Zhang, Y.; Zhang, L.; Ban, Q.; Li, J.; Li, C.-H.; Guan, Y.-Q. Preparation and Characterization of Hydroxyapatite Nanoparticles Carrying Insulin and Gallic Acid for Insulin Oral Delivery. Nanomedicine 2018, 14, 353–364.
- Shahin, N.N.; Shamma, R.N.; Ahmed, I.S. A Nano-Liposomal Formulation of Caffeic Acid Phenethyl Ester Modulates Nrf2 and NF-Κβ Signaling and Alleviates Experimentally Induced Acute Pancreatitis in a Rat Model. Antioxidants 2022, 11, 1536.
- Mangrulkar, S.; Shah, P.; Navnage, S.; Mazumdar, P.; Chaple, D. Phytophospholipid Complex of Caffeic Acid: Development, In Vitro Characterization, and In Vivo Investigation of Antihyperlipidemic and Hepatoprotective Action in Rats. AAPS Pharm. Sci. Tech. 2021, 22, 28.
- Yücel, Ç.; Karatoprak, G.Ş.; Aktaş, Y. Nanoliposomal Resveratrol as a Novel Approach to Treatment of Diabetes Mellitus. J. Nanosci. Nanotechnol. 2018, 18, 3856–3864.
- Frąk, W.; Wojtasińska, A.; Lisińska, W.; Młynarska, E.; Franczyk, B.; Rysz, J. Pathophysiology of Cardiovascular Diseases: New Insights into Molecular Mechanisms of Atherosclerosis, Arterial Hypertension, and Coronary Artery Disease. Biomedicines 2022, 10, 1938.
- Kotlyarov, S.; Kotlyarova, A. Molecular Pharmacology of Inflammation Resolution in Atherosclerosis. Int. J. Mol. Sci. 2022, 23, 4808.
- Mirhafez, S.R.; Mohebati, M.; Feiz Disfani, M.; Saberi Karimian, M.; Ebrahimi, M.; Avan, A.; Eslami, S.; Pasdar, A.; Rooki, H.; Esmaeili, H.; et al. An Imbalance in Serum Concentrations of Inflammatory and Anti-Inflammatory Cytokines in Hypertension. J. Am. Soc. Hypertens. 2014, 8, 614–623.
- Wu, H.; Su, M.; Jin, H.; Li, X.; Wang, P.; Chen, J.; Chen, J. Rutin-Loaded Silver Nanoparticles With Antithrombotic Function. Front. Bioeng. Biotechnol. 2020, 8, 598977.
- Chen, D.; Liu, Y.; Liu, P.; Zhou, Y.; Jiang, L.; Yuan, C.; Huang, M. Orally Delivered Rutin in Lipid-Based Nano-Formulation Exerts Strong Antithrombotic Effects by Protein Disulfide Isomerase Inhibition. Drug Deliv. 2022, 29, 1824–1835.
- Guo, M.; He, Z.; Jin, Z.; Huang, L.; Yuan, J.; Qin, S.; Wang, X.; Cao, L.; Song, X. Oral Nanoparticles Containing Naringenin Suppress Atherosclerotic Progression by Targeting Delivery to Plaque Macrophages. Nano Res. 2023, 16, 925–937.
- He, Y.; Wang, J.; Yan, W.; Huang, N. Gallic Acid and Gallic Acid-Loaded Coating Involved in Selective Regulation of Platelet, Endothelial and Smooth Muscle Cell Fate. RSC Adv. 2014, 4, 212–221.
- Alfei, S.; Grazia Signorello, M.; Schito, A.; Catena, S.; Turrini, F. Reshaped as Polyester-Based Nanoparticles, Gallic Acid Inhibits Platelet Aggregation, Reactive Oxygen Species Production and Multi-Resistant Gram-Positive Bacteria with an Efficiency Never Obtained. Nanoscale Adv. 2019, 1, 4148–4157.
- Yadav, Y.C.; Pattnaik, S.; Swain, K. Curcumin Loaded Mesoporous Silica Nanoparticles: Assessment of Bioavailability and Cardioprotective Effect. Drug Dev. Ind. Pharm. 2019, 45, 1889–1895.
- Li, X.; Xiao, H.; Lin, C.; Sun, W.; Wu, T.; Wang, J.; Chen, B.; Chen, X.; Cheng, D. Synergistic Effects of Liposomes Encapsulating Atorvastatin Calcium and Curcumin and Targeting Dysfunctional Endothelial Cells in Reducing Atherosclerosis. Int. J. Nanomed. 2019, 14, 649–665.
