本文简要介绍了大豆肽的结构、功能、吸收和代谢。本文还综述了大豆肽对肥胖、糖尿病、心血管疾病(CVD)和癌症等主要慢性疾病的调控作用。本文还探讨了大豆蛋白和多肽在慢性病中的功能研究的不足之处及未来可能的方向。
- chronic diseases
- soybean peptides
- diabetes mellitus
- obesity
- cardiovascular diseases
- cancer
With the development of urbanization and the increase in sedentary habits, chronic diseases have become a worldwide public health problem. Chronic diseases are noninfectious diseases, but not some specific diseases, with complex etiology, slow development, and long duration [1]. Chronic diseases may be caused by lifestyle, environment, diet, or genetic factors. There were 28 million people who died of chronic diseases world- wide in 1990, and this number increased to 36 million in 2008 and 39 million in 2016 [1]. More than two-thirds of the deaths worldwide are believed to be caused by chronic diseases [1]. In 2019, seven of the top ten causes of death were due to non-communicable diseases, according to the World Health Organization (WHO) [2]. At present, chronic diseases mainly include obesity, diabetes, cardiovascular diseases (CVD), and cancer, and they are key causes of premature death in humans [3]. The pathogenesis of chronic diseases is relatively complex, such as imbalances in the protease network, which can lead to malfunctions in the cellular signal network [4].
The expression of matrix metalloproteinases (MMPs) and the imbalance of the phosphoryladylinositol 3-kinase (PI3K)/AKT/major target of rapamycin (mTOR) signaling pathway may both have an impact on the development of chronic diseases such as CVD, type 2 diabetes (T2D), and cancer [4,5].
As metabolic diseases, chronic diseases are associated with metabolic syndrome (MetS). MetS is not a disease itself but a comprehensive concept, representing factors that increase the risks of individual diseases (as shown in Figure 1) [6]. It has been reported that several components of MetS led to a significant increase in the risk of chronic diseases and that the risk factors for chronic diseases and the definition of MetS partially overlap [7].
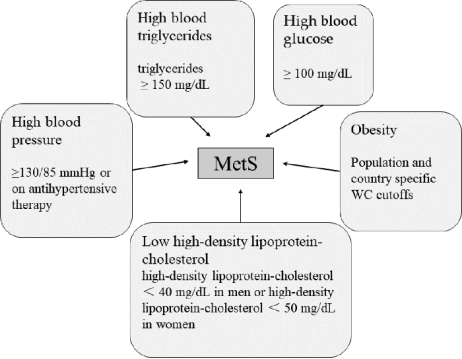
Figure 1. Main diagnosis of MetS. Three of the above five conditions are considered MetS [8].
Therefore, MetS may be a risk factor leading to the development of chronic diseases. Several diseases associated with both conditions have been identified, including obesity, T2D, CVD, and cancer [7].
Among these conditions (Figure 1), obesity is a major cause of MetS. Obesity may increase the susceptibility to insulin resistance, thus causing MetS. In 2005, the International Diabetes Federation recognized obesity as a necessary factor in the diagnosis of MetS [9], while Dr. Reaven objected to this and believed that insulin resistance might be the main cause of MetS [10]. MetS is an important risk factor for T2D and CVD (see Figure 2). With the increase in the number of patients with MetS, the number of patients with T2D and CVD also increased significantly [8].
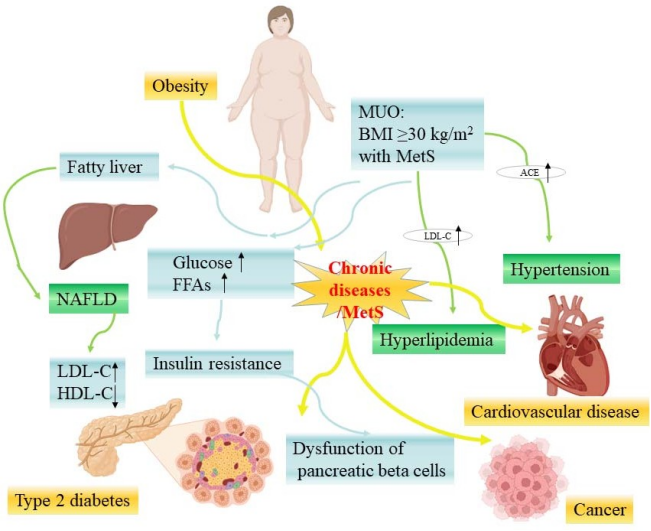
Figure 2. The relationship between chronic diseases and MetS-related diseases (some picture elements are from the BioRender). MUO—metabolic unhealthy obesity; NAFLD—nonalcoholic fatty liver disease; LDL-C—low-density lipoprotein cholesterol; HDL-C—high-density lipoprotein cholesterol; ACE—angiotensin-converting enzyme; FFAs—free fatty acids.
Obesity includes metabolic healthy obesity (MHO) and metabolic unhealthy obesity (MUO) [11], while MHO is unstable and transient, and most patients with MHO will transition to MUO stage with the accumulation of fat [12]. Morgan Mongraw Chaffin and colleagues found that MHO would develop into MUO when it exceeded a certain baseline (odds ratio [OR]: 1.60; 95% confidence interval [CI]: 1.14 to 2.25), and the risk of CVD for those with MUO increased significantly [13]. Due to the fact that obesity is the cause of heart diseases and the relationship between obesity and CVD is mediated by MetS, MetS can be regarded as a sign of obesity accumulation at the exposure threshold [13].
另一方面,肥胖可导致MetS发展为糖尿病,而非酒精性脂肪性肝病(NAFLD)是最常见的代谢性肝病,是两者之间的连续体[14]。在美国,约30%的成人患有NAFLD,其中20%是由肥胖者发展[15]。一篇meta分析纳入了24项研究,纳入了35,599例2型糖尿病患者,发现普通糖尿病患者NAFLD的患病率为59.67%,但在肥胖糖尿病患者中上升至77.87%[16]。MetS导致体内葡萄糖水平升高和游离脂肪酸过量产生[17],胰腺β细胞功能障碍程度与MetS的严重程度有关[18]。当胰腺β细胞长时间超过一定的代谢能力时,其质量和功能就会降低,代谢功能就会受损[17]。
目前,慢性病的治疗方法包括体育锻炼和饮食疗法,以及针对相关症状的药物。源自食品蛋白质的生物活性肽因其低成本和低副作用而被业界公认为改善健康。据报道,来自不同食物的多种生物活性肽具有生物活性,包括抗高血压、抗糖尿病和抗癌活性[19-21]。研究表明,增加植物蛋白的摄入量与降低肥胖、CVD、糖尿病、癌症和其他症状的风险有关[21]。大豆肽作为源自大豆蛋白的流行生物活性成分之一,已被用于许多健康方面,如抗肥胖、抗糖尿病、抗CVD、抗癌和抗氧化活性[22]。
作为一种传统植物,大豆在中国已有近5000年的种植历史[23]。美国于1965年引进大豆[24],现已成为世界上大豆产量最高的国家,产量达到世界总产量的45%[25]。后来,大豆的种植在其他国家逐渐发展起来,成为世界上流行的经济作物。蛋白质是大豆中最丰富的营养素,约占所有营养素的40%,是膳食蛋白质非常重要的植物来源[26]。大豆蛋白含有所有27种氨基酸,包括28种必需氨基酸[22,<>]。它的营养价值相当于动物蛋白,因此被认为是一种全价值蛋白质[<>]。
大豆肽是使用不同的蛋白酶水解大豆蛋白而衍生的,它们是寡肽的混合物,具有3-6个氨基酸,分子量为300-700 Da[29]。大豆肽的生理活性由其相对分子量的大小和氨基酸序列决定[30]。它们的氨基酸组成和比例与大豆蛋白相同,但更容易吸收,更稳定[31]。大豆蛋白和肽在过去已被证明是安全无毒的,这对它们的进一步利用很重要[32]。
本文综述了大豆肽的结构、功能、吸收和代谢特性。我们还讨论了它们对慢性病调节和改善的潜在影响。
This entry is adapted from the peer-reviewed paper 10.3390/nu15081811
