Microalgae and cyanobacteria could represent a potential natural alternative to antibiotic, antiviral, or antimycotic therapies, as well as a good supplement for the prevention and co-adjuvant treatment of different oral diseases.
- microalgae
- Spirulina platensis
- Chlorella vulgaris
- oral health
- antimicrobial activity
- Streptococcus mutans
Definition
Microalgae and cyanobacteria could represent a potential natural alternative to antibiotic, antiviral, or antimycotic therapies, as well as a good supplement for the prevention and co-adjuvant treatment of different oral diseases.
1. Introduction
Today, the majority of the bioactive peptides added in well-being promoting aliments, food supplements, pharmaceutic, and cosmetic formulations are realized by chemical production or by the partial digestion of proteins derived from animals. Therefore, they are not always well-regarded by the users due to the risks related to solvent contamination or the utilization of animal-derived ingredients. Alternatively, plant and microalgae-resulting peptides are recognized as selective, useful, nontoxic and well accepted when consumed, having a significant potentiality for utilization in functional aliments, drugs, and cosmetic products. Furthermore, due to the increasing issue of the antibiotic resistance against pathogenic bacteria, research has been targeted to exploring new antibacterial compounds derived from different natural environments [1][2][3][4]. Consequently, in recent years, growing scientific interest has been centered on the study of the bioactivity of extracts derived from plant species. In particular, the focus is on food plants included in the so-called traditional medicine [5][6][7][8]. For example, polyphenols derived from some edible plants drew attention as potential sources of agents that, among the wide range of health benefits, were shown to inhibit the bacterial growth of some oral pathogens[9][10]. A recent study on a large sample of vulnerary plants from Italian areas has identified a small number of extracts that could find application for the prevention of dental caries [11]: extracts of Camelia sinensis and Plantago lanceolata, rich in flavonoids, showed inhibitory activity against the species of cariogenic Streptococci [11][12].
Functional foods are arising as a dietary resource for preventing diseases. They can be defined as technologically developed ingredients explicating specific actions on human health. In the scenario of growing promising sources of functional foods and preventive drugs, cyanobacteria and microalgae are drawing global interest, due to their content of highly valuable substances [13][14]
Cyanobacteria and microalgae are respectively prokaryotic or eukaryotic microorganisms growing through oxygenic photosynthesis. Their energetic intake requires light, carbon dioxide, water, and nutrients with phosphorus and nitrogen as major nutrients, whereas the products of metabolic activity are primarily carbohydrates, along with a surprisingly high number of chemicals, some of which are known to be useful for humans [13].
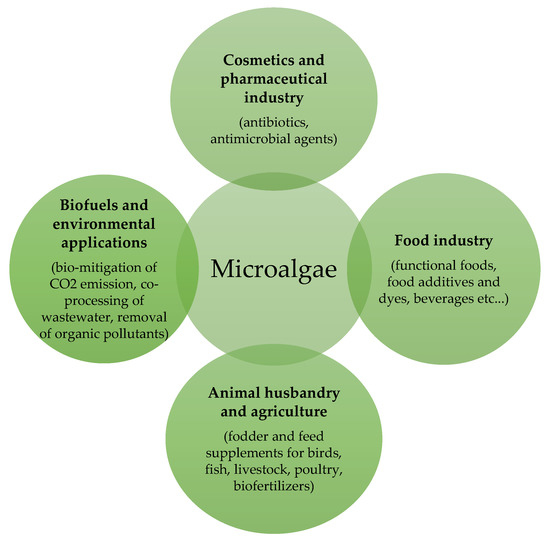
Both cyanobacteria and microalgae are widely spread in freshwater and marine ecosystems as well as on terrestrial habitats and in a wide range of extreme environments, from hot springs to barren rocks of deserts. This flexibility makes them the major producers of biomass under sustainable conditions, since they do not deprive agriculture of sources, while allowing water recycling and lowering polluting gas emissions [15]. Moreover, cyanobacteria and microalgae bring the potential to be converted into a wide range of products of economic interest, such as biofuels, cosmetics, renewable chemicals and other valuable compounds[15], animal and human food, especially as sources of proteins, lipids, and phytochemicals (Figure 1) [16].
2. Microalgal Effects on Oral Health
2.1. Antiviral Activity
2.2. Oral Cancer Chemoprevention
2.3. Oral Antimicrobial Activity
2.4. Potential Effects in the Treatment of Periodontitis
2.5. Control of Oral Submucous Fibrosis
2.6. Salivary Secretion Improving
2.7. More Oral Benefits from Chlorella sp. and Other Algal Extracts
This entry is adapted from the peer-reviewed paper 10.3390/molecules25215164
References
- Mundt, S.; Kreitlow, S.; Nowotny, A.; Effmert, U. Biochemical and pharmacological investigations of selected cyanobacteria. Int. J. Hyg. Environ. Health 2001, 203, 327–334.
- Safonova, E.; Kvitko, K.; Kuschk, P.; Möder, M.; Reisser, W. Biodegradation of Phenanthrene by the Green Alga Scenedesmus obliquus ES--55. Eng. Life Sci. 2005, 5, 234–239.
- Ghasemi, Y.; Mohagheghzadeh, A.; Mohammad, H.M.; Moradian, A.; Shadman, S. Antifungal and Antibacterial Activity of the Microalgae Collected from Paddy Fields of Iran: Characterization of Antimicrobial Activity of Chroococcus disperses. J. Biol. Sci. 2007, 7, 904–910.
- Prakash, O.; Hussain, K.; Aneja, K.R.; Sharma, C. Synthesis and Antimicrobial Activity of Some New 2-(3-(4-Aryl)-1-phenyl-1H-pyrazol-4-yl) Chroman-4-ones. Indian J. Pharm. Sci. 2011, 73, 586–590.
- De Natale, A.; Pollio, A. Plants species in the folk medicine of Montecorvino Rovella (inland Campania, Italy). J. Ethnopharmacol. 2007, 109, 295–303.
- Perrin, S.; Fougnies, C.; Grill, J.P.; Jacobs, H.; Schneider, F. Fermentation of chicory fructo-oligosaccharides in mixtures of different degrees of polymerization by three strains of bifidobacteria. Can. J. Microbiol. 2002, 48, 759–763.
- Lee, M.H.; Kwon, H.A.; Kwon, D.Y.; Park, H.; Sohn, D.H.; Kim, Y.C.; Eo, S.K.; Kang, H.Y.; Kim, S.W.; Lee, J.H. Antibacterial activity of medicinal herb extracts against Salmonella. Int. J. Food Microbiol. 2006, 111, 270–275.
- Mazzanti, G. Pharmacological considerations on herbal medicine use. Ann. Ist. Super. Sanita 2005, 41, 23–26.
- Taguri, T.; Tanaka, T.; Kouno, I. Antimicrobial activity of 10 different plant polyphenols against bacteria causing food-borne disease. Biol. Pharm. Bull. 2004, 27, 1965–1969.
- Ferrazzano, G.F.; Cantile, T.; Roberto, L.; Ingenito, A.; Catania, M.R.; Roscetto, E.; Palumbo, G.; Zarrelli, A.; Pollio, A. Determination of the in vitro and in vivo antimicrobial activity on salivary Streptococci and Lactobacilli and chemical characterisation of the phenolic content of a Plantago lanceolata infusion. Biomed. Res. Int. 2015, 2015, 286817.
- Ferrazzano, G.F.; Roberto, L.; Catania, M.R.; Chiaviello, A.; De Natale, A.; Roscetto, E.; Pinto, G.; Pollio, A.; Ingenito, A.; Palumbo, G. Screening and Scoring of Antimicrobial and Biological Activities of Italian Vulnerary Plants against Major Oral Pathogenic Bacteria. Evid. Based Complement. Altern. Med. 2013, 316280, doi:10.1155/2013/316280.
- Ferrazzano, G.F.; Amato, I.; Ingenito, A.; Zarrelli, A.; Pinto, G.; Pollio, A. Plant polyphenols and their anti-cariogenic properties: A review. Molecules 2011, 16, 1486–1507.
- Galasso, C.; Gentile, A.; Orefice, I.; Ianora, A.; Bruno, A.; Noonan, D.M.; Sansone, C.; Albini, A.; Brunet, C. Microalgal Derivatives as Potential Nutraceutical and Food Supplements for Human Health: A Focus on Cancer Prevention and Interception. Nutrients 2019, 11, 6.
- Apone, F.; Barbulova, A.; Colucci, M.G. Plant and Microalgae Derived Peptides Are Advantageously Employed as Bioactive Compounds in Cosmetics. Front. Plant Sci. 2019, 10, 756.
- Camacho, F.; Macedo, A.; Malcata, F. Potential Industrial Applications and Commercialization of Microalgae in the Functional Food and Feed Industries: A Short Review. Mar. Drugs 2019, 17, 6.
- Langi, P.; Kiokias, S.; Varzakas, T.; Proestos, C. Carotenoids: From Plants to Food and Feed Industries. Methods Mol. Biol. 2018, 1852, 57–71.
- Suzich, J.B.; Cliffe, A.R. Strength in diversity: Understanding the pathways to herpes simplex virus reactivation. Virology 2018, 522, 81–91.
- Mader, J.; Gallo, A.; Schommartz, T.; Handke, W.; Nagel, C.H.; Günther, P.; Brune, W.; Reich, K. Calcium spirulan derived from Spirulina platensis inhibits herpes simplex virus 1 attachment to human keratinocytes and protects against herpes labialis. J. Allergy Clin. Immunol. 2016, 137, 197–203.
- Wong, T.; Wiesenfeld, D. Oral Cancer. Aust. Dent. J. 2018, 1, 91–99.
- Shibahara, T. Oral cancer -diagnosis and therapy-. Clin. Calcium 2017, 27, 1427–1433.
- Mori, H.; Tanaka, T.; Sugie, S.; Yoshimi, N.; Kawamori, T.; Hirose, Y.; Ohnishi, M. Chemoprevention by naturally occurring and synthetic agents in oral, liver, and large bowel carcinogenesis. J. Cell. Biochem. Suppl. 1997, 27, 35–41.
- Tanaka, T.; Makita, H.; Ohnishi, M.; Mori, H.; Satoh, K.; Hara, A. Chemoprevention of rat oral carcinogenesis by naturally occurring xanthophylls, astaxanthin and canthaxanthin. Cancer Res. 1995, 55, 4059–4064.
- Grawish, M.E. Effects of Spirulina platensis extract on Syrian hamster cheek pouch mucosa painted with 7,12-dimethylbenz[a]anthracene. Oral Oncol. 2008, 44, 956–962.
- Grawish, M.E.; Zaher, A.R.; Gaafar, A.I.; Nasif, W.A. Long-term effect of Spirulina platensis extract on DMBA-induced hamster buccal pouch carcinogenesis (immunohistochemical study). Med. Oncol. 2010, 27, 20–28.
- Schwartz, J.; Shklar, G.; Reid, S.; Trickler, D. Prevention of experimental oral cancer by extracts of Spirulina-Dunaliella algae. Nutr. Cancer. 1988, 11, 127–134.
- Kowshik, J.; Baba, A.B.; Giri, H.; Deepak Reddy, G.; Dixit, M.; Nagini, S. Astaxanthin inhibits JAK/STAT-3 signaling to abrogate cell proliferation, invasion and angiogenesis in a hamster model of oral cancer. PLoS ONE 2014, 9, 109–114.
- Azizi, A.; Aghayan, S.; Zaker, S.; Shakeri, M.; Entezari, N.; Lawaf, S. In Vitro Effect of Zingiber officinale Extract on Growth of Streptococcus mutans and Streptococcus sanguinis. Int. J. Dent. 2015, 2015, 489842.
- Zhou, Y.; Millhouse, E.; Shaw, T.; Lappin, D.F.; Rajendran, R.; Bagg, J.; Lin, H.; Ramage, G. Evaluating Streptococcus mutans Strain Dependent Characteristics in a Polymicrobial Biofilm Community. Front. Microbiol. 2018, 9, 1498.
- Rakic, M.; Galindo-Moreno, P.; Monje, A.; Radovanovic, S.; Wang, H.L.; Cochran, D.; Sculean, A.; Canullo, L. How frequent does peri-implantitis occur? A systematic review and meta-analysis. Clin. Oral Investig. 2018, 22, 1805–1816.
- Komiyama, E.Y.; Lepesqueur, L.S.; Yassuda, C.G.; Samaranayake, L.P.; Parahitiyawa, N.B.; Balducci, I.; Koga-Ito, C.Y. Enterococcus Species in the Oral Cavity: Prevalence, Virulence Factors and Antimicrobial Susceptibility. PLoS ONE 2016, 11, e0163001.
- Davoodbasha, M.; Edachery, B.; Nooruddin, T.; Lee, S.Y.; Kim, J.W. An evidence of C16 fatty acid methyl esters extracted from microalga for effective antimicrobial and antioxidant property. Microb. Pathog. 2018, 115, 233–238.
- Uma, R.; Sivasubramanian, V.; Niranjali Devaraj, S. Preliminary phycochemical analysis and in vitro antibacterial screening of green microalgae, Desmococcus Olivaceous, Chlorococcum humicola and Chlorella vulgaris. J. Algal Biomass Utln. 2011, 2, 74–81.
- Madhumathi, V.; Deepa, P.; Jeyachandran, S.; Manoharan, C.; Vijayakumar, S. Antimicrobial Activity of Cyanobacteria Isolated from Freshwater Lake. Int. J. Microbiol. Res. 2011, 2, 213–216.
- Zarska, M.; Novotny, F.; Havel, F.; Sramek, M.; Babelova, A.; Benada, O.; Novotny, M.; Saran, H.; Kuca, K.; Musilek, K.; et al. Two-Step Mechanism of Cellular Uptake of Cationic Gold Nanoparticles Modified by (16-Mercaptohexadecyl) trimethylammonium Bromide. Bioconjug. Chem. 2016, 27, 2558–2574.
- Wei, L.; Lu, J.; Xu, H.; Patel, A.; Chen, Z.S.; Chen, G. Silver nanoparticles: Synthesis, properties, and therapeutic applications. Drug Discov. Today. 2015, 20, 595–601.
- Salaheldin, T.A.; Loutfy, S.A.; Ramadan, M.A.; Youssef, T.; Mousa, S.A. IR-enhanced photothermal therapeutic effect of graphene magnetite nanocomposite on human liver cancer HepG2 cell model. Int. J. Nanomed. 2019, 14, 4397–4412.
- Rashad, S.; El-Chaghaby, G.A.; Elchaghaby, M.A. Antibacterial activity of silver nanoparticles biosynthesized using Spirulina platensis microalgae extract against oral pathogens. Egypt. J. Aquat. Biol. Fish. 2019, 23, 261–266.
- Bosshardt, D.D. The periodontal pocket: Pathogenesis, histopathology and consequences. Periodontol. 2000 2018, 76, 43–50.
- Deas, D.E.; Moritz, A.J.; Sagun, R.S. Jr; Gruwell, S.F.; Powell, C.A. Scaling and root planing vs. conservative surgery in the treatment of chronic periodontitis. Periodontal. 2000 2016, 71, 128–139.
- Mahendra, J.; Mahendra, L.; Muthu, J.; John, L.; Romanos, G.E. Clinical effects of subgingivally delivered spirulina gel in chronic periodontitis cases: A placebo controlled clinical trial. J. Clin. Diagn. Res. 2013, 7, 2330–2333.
- Balci Yuce, H.; Lektemur Alpan, A.; Gevrek, F.; Toker, H. Investigation of the effect of astaxanthin on alveolar bone loss in experimental periodontitis. J. Periodontal Res. 2018, 53, 131–138.
- Hwang, Y.; Kwang-Jin, K.; Su-Jin, K.; Seul-Ki, M.; Seong-Gyeol, H.; Young-Jin, S.; Sung-Tae, Y. Suppression Effect of Astaxanthin on Osteoclast Formation In Vitro and Bone Loss In Vivo. Int. J. Mol. Sci. 2018, 19, 1–17.
- Kose, O.; Arabaci, T.; Yemenoglu, H.; Kara, A.; Ozkanlar, S.; Kayis, S.; Duymus, Z.Y. Influences of Fucoxanthin on Alveolar Bone Resorption in Induced Periodontitis in Rat Molars. Mar. Drugs 2016, 14, 70.
- Molteni, M.; Bosi, A.; Rossetti, C. The Effect of Cyanobacterial LPS Antagonist (CyP) on Cytokines and Micro-RNA Expression Induced by Porphyromonas gingivalis LPS. Toxins 2018, 10, 290.
- Orpha.Net. Available online: https://www.orpha.net/consor/cgi-bin/OC_Exp.php?lng=IT&Expert=357154 (accessed on 10 February 2019).
- Kanjani, V.; Annigeri, R.G.; Revanappa, M.M.; Rani, A. Efficacy of Spirulina along with Different Physiotherapeutic Modalities in the Management of Oral Submucous Fibrosis. Ann. Maxillofac. Surg. 2019, 9, 23–27.
- Shetty, P.; Shenai, P.; Chatra, L.; Rao, P.K. Efficacy of spirulina as an antioxidant adjuvant to corticosteroid injection in management of oral submucous fibrosis. Indian J. Dent. Res. 2013, 24, 347–350.
- Mulk, B.S.; Deshpande, P.; Velpula, N.; Chappidi, V.; Chintamaneni, R.L.; Goyal, S. Spirulina and pentoxyfilline-a novel approach for treatment of oral submucous fibrosis. J. Clin. Diagn. Res. 2013, 7, 3048–3050.
- Kuraji, M.; Matsuno, T.; Satoh, T. Astaxanthin affects oxidative stress and hyposalivation in aging mice. J. Clin. Biochem. Nutr. 2016, 59, 79–85.
- Yamada, T.; Ryo, K.; Tai, Y.; Tamaki, Y.; Inoue, H.; Mishima, K.; Tsubota, K.; Saito, I. Evaluation of Therapeutic Effects of Astaxanthin on Impairments in Salivary Secretion. J. Clin. Biochem. Nutr. 2010, 47, 130–137.
- Otsuki, T.; Shimizu, K.; Zempo-Miyaki, A.; Maeda, S. Changes in salivary flow rate following Chlorella-derived multicomponent supplementation. J. Clin. Biochem. Nutr. 2016, 59, 45–48.
- Merino, J.J.; Parmigiani-Izquierdo, J.M.; Toledano Gasca, A.; Cabaña-Muñoz, M.E. The Long-Term Algae Extract (Chlorella and Fucus sp) and Aminosulphurate Supplementation Modulate SOD-1 Activity and Decrease Heavy Metals (Hg++, Sn) Levels in Patients with Long-Term Dental Titanium Implants and Amalgam Fillings Restorations. Antioxidants 2019, 8, 101.
- Cicco, S.R.; Vona, D.; Leone, G.; De Giglio, E.; Bonifacio, M.A.; Cometa, S.; Fiore, S.; Palumbo, F.; Ragni, R.; Farinola, G.M. In vivo functionalization of diatom biosilica with sodium alendronate as osteoactive material. Mater. Sci. Eng. C Mater. Biol. Appl. 2019, 104, 109897.
