Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Robot-assisted surgical systems (RASS) have revolutionised the management of many urological conditions with robot-assisted radical prostatectomy (RARP) being considered by many to be the preferred surgical approach.
- robotic surgery
- learning curves
- prostatectomy
- robotic systems
1. Introduction
The advent of robot-assisted surgery (RAS) in the early 2000s has revolutionised the management of many urological conditions, particularly prostate cancer, with robot-assisted laparoscopic radical prostatectomy (RARP) now being considered by many to be the preferred surgical approach [1][2]. By 2017–2019, 88% of all radical prostatectomies in the UK were robot-assisted, a significant growth since the first ever RARP was performed in Germany in 2000 [3][4]. RAS has the benefits of minimally invasive surgery compared to open surgery with faster recovery, shorter length of stay and reduced tissue trauma, whilst also overcoming many of the challenges faced by laparoscopy [1][5][6]. RAS provides a 3D, magnified visualisation of the surgical field and improved ergonomics for the surgeon with instruments allowing greater dexterity [7]. Since its introduction, there has been a rapid uptake and adoption of RAS in many branches of medicine and surgery [8][9][10][11].
Within the field of urology, RAS systems have been utilised in a wide variety of oncological and non-oncological conditions, including cystectomy with intracorporeal or extracorporeal urinary diversion, partial or radical nephrectomy, retroperitoneal lymph node dissection (RPLND), adrenalectomy, pyeloplasty and artificial urinary sphincter insertion [10][11]. Robot-assisted radical cystectomy (RARC) has been associated with increased operative time but also a reduced length of stay compared to an open approach [12]. Robot-assisted partial nephrectomy has been associated with a reduced rate of conversion to open surgery compared to a laparoscopic approach, a reduced length of stay and a smaller reduction in glomerular filtration rate [13]. Robotic RPLND has been associated with reduced overall complication rate and reduced blood transfusion compared to open RPLND, but there was a 9% rate of conversion to open surgery in post-chemotherapy patients [14].
Since first approval by the US Food and Drug Administration (FDA) in 2000 for human use, the da Vinci surgical system (Intuitive Surgical, Sunnyvale, CA, USA) has dominated the market for more than 20 years to the extent that da Vinci has become synonymous with robotic surgery. The market dominance achieved through early successes and judicious patenting of technological developments appears to be coming to an end [8]. The lack of competition has allowed Intuitive Surgical to monopolise the global surgical robotics market, which was estimated at USD 3.6 billion in 2021 with a predicted annual growth rate of 19.3% from 2022 to 2030 [15]. Intuitive Surgical reported that almost 1.6 million operations were performed with the da Vinci systems in 2021 alone [16]. In the last few years, several alternative robotic surgical systems have been announced and are at various stages of development and commercial availability [17][18][19][20]. This heralds an exciting time for robotic surgery as the increased competition will inevitably drive forward technological advancements and cost reduction.
However, the current costs associated with RAS can be prohibitively expensive to many regions, limiting the use of robotic surgery [21]. Another challenge is the need to adequately train surgeons to competently perform RAS, with each procedure coming with its own learning curve [22]. Furthermore, mechanical failure of robotic surgery systems can rarely result in patient harm or the need to convert to an open procedure.
2. History of Robotics in Urology
Robotics was first introduced into urology in the 1980s when the PROBOT was developed as an autonomous robot to perform robotic transurethral resection of the prostate [23]. Although these trials proved to be safe and successful, the PROBOT was never widely produced and implemented. In the latter half of the 1990s, there was increasing interest in ‘master-slave’ robotic technology with a view to improving laparoscopic surgery. ZEUS (Computer Motion, Goleta, CA, USA) and da Vinci (Intuitive Surgical, Sunnyvale, CA, USA) were developed at a similar time; however, the seven degrees of freedom (DoF) afforded by the four arms of the da Vinci system with its 3D binocular imagery proved superior [24]. A merger between Intuitive and Computer Motion in 2003 paved the way for 20 years of dominance by successive generations of Intuitive’s da Vinci systems.
3. Robotic Systems
Robot-assisted surgical systems (RASS) are designed to overcome many of the shortcomings of conventional laparoscopic surgery. Whilst laparoscopic surgery undoubtedly has benefits in reducing tissue trauma and reducing the length of hospital stay for patients compared to open surgery, it does have some negative aspects [7]. Most are related to the ergonomics of laparoscopic surgery, where there is a high burden on surgeons and their assistants to hold equipment, retract tissue and manipulate the camera, which can be associated with negative health impacts, including shoulder and hand pain, due to unnatural working angles [25]. Robots take on this role, freeing clinicians and assistants to perform alternative tasks. Robotic surgery facilitates greater discriminatory movements afforded by seven DoF compared to four DoF for conventional laparoscopic surgery [7]. Alongside the greater dexterity and discriminatory movements offered by RAS, other benefits included tremor filtration and 3D visualisation that offers an improved field of view, particularly in the pelvis [1].
Developments in surgical technique have also been improved with the increased exposure and visibility afforded by RAS. Retzius-sparing RARP approaches the prostate from the posterior aspect of the bladder, which is a small space that would be inaccessible with laparoscopic surgery [9]. Reported benefits include improved early continence using a Retzius-sparing technique, but this difference has diminished at twelve months [9][26]. Although there have been some concerns regarding positive surgical margins when using a Retzius-sparing technique, a recent meta-analysis suggests these may be unfounded [26].
Longer term outcomes are also being reported for patients undergoing RAS. A multi-centre prospective study comparing RARP to open retropubic radical prostatectomy (RRP) found lower rates of erectile dysfunction, prostate cancer-specific mortality and biochemical recurrence for the RARP group after 8 years of follow-up, although despite 4000 participants, this study was limited by the lack of randomisation [27].
4. Da Vinci
Intuitive Surgical currently offers both multiport and single-port RAS systems with the X/Xi and SP models currently available. The da Vinci X/Xi consists of a patient cart, surgeon console away from the operating table, and a vision cart [28] (Figure 1). The closed surgeon console provides a 3D high-definition view and the surgeon uses the hand controls from a seated position to manipulate the robotic instruments [28]. The multi-arm patient cart utilises 8 mm diameter instruments and an 8 mm camera, allowing versatility of camera placement and therefore facilitating multi-quadrant procedures [28]. The da Vinci Xi incorporates EndoWrist technology which simulates the movements of a human wrist with seven DoF and is coupled with a tremor-filtering system for smooth, controlled movements [28].
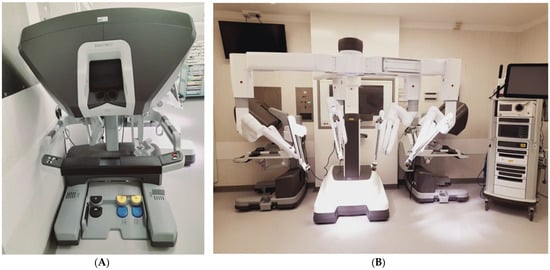
Figure 1. Da Vinci Xi Robotic System (A) Surgeon’s Console. (B) Robot cart with 4 arms deployed in centre of image, the vision cart is to the right of the image.
The da Vinci single-port (SP) system was approved for use in urological surgery in 2018 by the FDA. This system has a 25 mm multichannel port at the sole entry point, which incorporates a 12 × 10 mm articulating endoscopic camera and three double-jointed articulating instruments [29]. An additional assistant port is typically employed, usually in the right lower quadrant for RARP, for example [30][31]. As with the Xi, a dual surgeon console setup can facilitate training of surgeons [29]. A recent meta-analysis suggests equivalence of initial outcomes between single-port and multi-port RAS for RARP in terms of blood loss and operative time, with SP systems associated with having a shorter length of stay [32]. However, the studies included are predominately single-centre case series and due to the nascency of SP RASS, longer term functional and oncological outcomes are not yet known [32]. The technical differences between a SP and multi-port systems inevitably means that there will be a learning curve required to transition to single-port system, even for surgeons with substantial experience at performing RARPs using multi-port systems [30].
5. Versius
The Versius surgical system (CMR Ltd., Cambridge, UK) has been licensed for use in Europe as of March 2019 [33]. It features an open surgeon’s console that can be configured to allow for a sitting or standing position and is compact with individual bedside units for each robotic arm [18]. V-wrist technology is implemented, allowing seven DoF and 360 degrees of wrist motion to manipulate the sterilisable 5 mm instruments [18]. Whilst preclinical evaluation has been carried out with cadaveric nephrectomies and prostatectomies, there is a lack of clinical data published to date [34]. Early clinical experiences in colorectal surgery and gynaecology suggest that the Versius system is safe, but a greater body of evidence is required to substantiate these findings [35]. Nevertheless, CMR have reported that over 5000 clinical cases have now been performed across their 100 installed robots in November 2022 [36].
6. Senhance
The Senhance (Asensus Surgical, Durham, NC, USA) robotic system received FDA approval in 2017, but this was limited to general surgical and gynaecological procedures. Described as a digital laparoscopy system, with instrument controls at the surgeon console providing haptic feedback to the surgeon and resembling traditional laparoscopic instruments, it offers an easier transition to robotic surgery for those trained in laparoscopic surgery [17]. The console is open in design, allowing for greater teamwork, and the 3D imagery is obtained via specialist polarised glasses. The system also uses an eye-tracking control to manipulate the camera to adjust the field of view [17]. The four robotics arms have their own cart and the instruments utilised have diameters of 3, 5 and 10 mm and are reusable after sterilisation, reducing costs [17]. Although there are a few European case series from Lithuania and Croatia, the uptake has been limited in the US by a lack of FDA approval for urological surgery [37][38].
7. Hinotori
The Hinotori (Medicaroid Corporation, Kobe, Japan) surgical robotic system was approved for use in Japan by the Japanese authorities in 2020. The Hinotori has a four-arm operational unit that adds an eighth DoF over the da Vinci X/Xi systems, potentially enabling smoother movements [19]. The surgeon console is a semi-closed design and allows the surgeons to manipulate the instruments using loop-like controls. A first-in-human trial of RARP in 30 patients was recently successfully undertaken following pre-clinical trials [19]. The authors suggested an equivalent performance to the da Vinci system, but further studies will be required to validate these findings. The relative similarity between the Hinotori and da Vinci systems does suggest that transitioning between systems may be easier than with other robotic systems.
8. Revo-I
The Revo-I (Meere Company Inc., Yongin, Republic of Korea) has regulatory approval in South Korea granted by the Korean Ministry of Food and Drug Safety in 2017. The Revo-I has a closed surgeon console, four-arm bedside cart and vision cart [20]. The 7.4 mm instruments permit seven DoF and are reusable after sterilisation up to twenty times [20]. The first clinical study of Revo-I was for 17 patients undergoing Retzius-sparing RARP with successful completion of surgery and no conversions to open or laparoscopic surgery [20]. Subsequent comparisons have been made between the Revo-I and Da Vinci systems, although notably with the previous generation Si model, where there was no difference in short-term oncological times [39]. The authors also reported that the da Vinci Si system did have shorter operative duration but also a longer length of stay compared to the Revo-I [39].
9. Hugo
The Hugo RAS system (Medtronic, Minneapolis, MN, USA) was granted European approval for urological and gynaecological procedures in 2021, which broadened to include general surgery in 2022. It has an open surgeon console, four-individual arm carts and a systems tower [40]. Similar to the Senhance system, the 3D surgical display can be seen with dedicated glasses. An 11 mm port is used for the endoscopic camera with 8 mm ports for surgical instruments [40]. Initial reports of undertaking RARP with the Hugo system have recently been published with no intra-operative complications or technical failures identified [41][42]. However, these case series are of fewer than ten patients each and larger, multi-centre series are anticipated in the near future.
10. Avatera
The Avatera RAS system (Avateramedical, Jena, Germany) was awarded European approval in November 2019, primarily for use in urology and gynaecology [43] (Figure 2). It features a closed surgeon console unit and a robotic cart with four arms that use disposable 5 mm diameter instruments [43]. Initial studies undertaking six RARC with intracorporeal urinary diversion and six radical nephrectomies, respectively, in anaesthetised live porcine models reported no mechanical issues or major complications encountered [44][45].
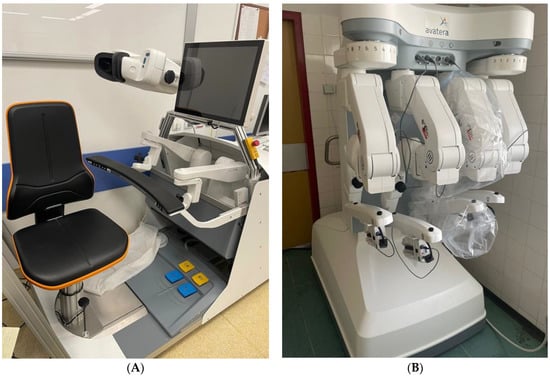
Figure 2. Avatera robotic system. (A) Closed surgeon’s console. (B) Robotic cart with four arms in the stored position.
11. Future Developments
The Dexter RAS system (Distalmotion, Épalinges, Switzerland) has European CE approval and differs from alternative RAS systems by offering ‘on-demand robotics’ at a lower cost [46]. The system is intended to allow an easy transition between laparoscopy and robotic access during an operation with two robotic arms that can be free-standing or fixed to the operating table with a sterile robotic console [46]. The company has recently announced completion of RARP and Millin’s prostatectomy using the Dexter system, but no formal evaluation has yet been published [47]. Johnson & Johnson’s Ottava RAS system is in development, a six-arm system that is designed to integrate into the operating table, thereby saving space and improving flexibility [48]. Whilst this may represent a significant development in the versatility of RAS systems, it is currently unclear when Ottava will be released.
Although RAS systems have been used in the management of renal tract calculi, these have predominately been utilised in select cases where conventional treatments have failed or have been deemed unsuitable [49]. However, the Monarch Platform robotic surgical system (Auris Health Inc., Redwood City, CA, USA) has recently been granted FDA approval for endourology use, having initially been approved for robot-assisted bronchoscopy [50]. Early findings in porcine models have recently been presented using the Monarch Platform in both percutaneous nephrolithotomy and ureteroscopy with results comparable to conventional devices [51].
Outcomes for RARP have been extensively investigated and tend to support improved early functional outcomes, but studies are less unanimous regarding longer term functional and oncological outcomes. Consequently, current EAU guidelines acknowledge that while RARP has become the preferred minimally invasive approach, it does not currently advocate any one approach (open, laparoscopic or robotic) over another [2].
A benefit of RASS is that the surgeon can operate on a patient away from the operating table. Typically, at a console within the same operating theatre, but there is the potential for robotic surgery to be combined with telemedicine to allow a surgeon to operate on a patient that is in a distant location and even in a different continent [52]. This could allow for improved accessibility to specialist healthcare with reduced need for travel, with particular benefits to those in rural areas or battlefield locations. Although the first transatlantic robotic surgery was first successfully performed 20 years ago, the use of remote robotic surgery is not widespread [53]. Current issues limiting its use are concerns with connectivity issues, time-lag and legal issues [52].
This entry is adapted from the peer-reviewed paper 10.3390/jcm12062268
References
- De Marchi, D.; Mantica, G.; Tafuri, A.; Giusti, G.; Gaboardi, F. Robotic surgery in urology: A review from the beginning to the single-site. AME Med. J. 2022, 7, 16.
- Mottet, N.; Cornford, P.; van den Bergh, R.C.N.; Eberli, D.; De Meerleer, G.; De Santis, M.; Gillessen, S.; Grummet, J.; Henry, A.M.; van der Kwast, T.H.; et al. European Association of Urologists Guidelines on Prostate Cancer. Available online: https://uroweb.org/guidelines/prostate-cancer (accessed on 14 November 2022).
- Binder, J.; Kramer, W. Robotically-assisted laparoscopic radical prostatectomy. BJU Int. 2001, 87, 408–410.
- The British Association of Urological Surgeons (BAUS). Radical Prostatectomy Outcomes Data. Available online: www.baus.org.uk/patients/surgical_outcomes/radical_prostatectomy (accessed on 2 November 2022).
- Hubert, N.; Gilles, M.; Desbrosses, K.; Meyer, J.P.; Felblinger, J.; Hubert, J. Ergonomic assessment of the surgeon’s physical workload during standard and robotic assisted laparoscopic procedures. Int. J. Med. Robot. 2013, 9, 142–147.
- Prete, F.P.; Pezzolla, A.; Prete, F.; Testini, M.; Marzaioli, R.; Patriti, A.; Jimenez-Rodriguez, R.M.; Gurrado, A.; Strippoli, G.F. Robotic versus laparoscopic minimally invasive surgery for rectal cancer: A systematic review and meta-analysis of randomized controlled trials. Ann. Surg. 2018, 267, 1034–1046.
- Supe, A.N.; Kulkarni, G.V.; Supe, P.A. Ergonomics in laparoscopic surgery. J. Minim. Access Surg. 2010, 6, 31–36.
- Rao, P.P. Robotic surgery: New robots and finally some real competition! World J. Urol. 2018, 36, 537–541.
- Rosenberg, J.E.; Jung, J.H.; Edgerton, Z.; Lee, H.; Lee, S.; Bakker, C.J.; Dahm, P. Retzius-sparing versus standard robotic-assisted laparoscopic prostatectomy for the treatment of clinically localized prostate cancer. Cochrane Database Syst. Rev. 2020, 8, CD013641.
- Pal, R.P.; Koupparis, A.J. Expanding the indications of robotic surgery in urology: A systematic review of the literature. Arab. J. Urol. 2018, 16, 270–284.
- Zahid, A.; Ayyan, M.; Farooq, M.; Cheema, H.A.; Shahid, A.; Naeem, F.; Ilyas, M.A.; Sohail, S. Robotic surgery in comparison to the open and laparoscopic approaches in the field of urology: A systematic review. J. Robotic Surg. 2023, 17, 11–29.
- Sathianathen, N.J.; Kalapara, A.; Frydenberg, M.; Lawrentschuk, N.; Weight, C.J.; Parekh, D.; Konety, B.R. Robotic Assisted Radical Cystectomy vs Open Radical Cystectomy: Systematic Review and Meta-Analysis. J. Urol. 2019, 201, 715–720.
- Choi, J.E.; You, J.H.; Kim, D.K.; Rha, K.H.; Lee, S.H. Comparison of perioperative outcomes between robotic and laparoscopic partial nephrectomy: A systematic review and meta-analysis. Eur. Urol. 2015, 67, 891–901.
- Garg, H.; Mansour, A.M.; Psutka, S.P.; Kim, S.P.; Porter, J.; Gaspard, C.S.; Dursun, F.; Pruthi, D.K.; Wang, H.; Kaushik, D. Robotic retroperitoneal lymph node dissection: A systematic review of perioperative outcomes. BJU Int. 2023. Epub ahead of print.
- Grand View Research. Surgical Robots Market Size, Share & Trends Analysis Report by Application (Orthopedics, Neurology, Urology, Gynecology), by Region (North America, Europe, Asia Pacific, LATAM, MEA), and Segment Forecasts, 2022–2030. Available online: https://www.grandviewresearch.com/industry-analysis/surgical-robot-market (accessed on 14 November 2022).
- Intuitive Surgical. Intuitive Announces Preliminary Fourth Quarter and Full Year 2021 Results. Available online: https://isrg.intuitive.com/news-releases/news-release-details/intuitive-announces-preliminary-fourth-quarter-and-full-year-1 (accessed on 14 November 2022).
- Stephan, D.; Sälzer, H.; Willeke, F. First Experiences with the New Senhance® Telerobotic System in Visceral Surgery. Visc. Med. 2018, 34, 31–36.
- Haig, F.; Medeiros, A.C.B.; Chitty, K.; Slack, M. Usability assessment of Versius, a new robot-assisted surgical device for use in minimal access surgery. BMJ Surg. Interv. Health Technol. 2020, 22, e000028.
- Hinata, N.; Yamaguchi, R.; Kusuhara, Y.; Kanayama, H.; Kohjimoto, Y.; Hara, I.; Fujisawa, M. Hinotori Surgical Robot System, a novel robot-assisted surgical platform: Preclinical and clinical evaluation. Int. J. Urol. 2022, 29, 1213–1220.
- Chang, K.D.; Abdel Raheem, A.; Choi, Y.D.; Chung, B.H.; Rha, K.H. Retzius-sparing robot-assisted radical prostatectomy using the Revo-i robotic surgical system: Surgical technique and results of the first human trial. BJU Int. 2018, 122, 441–448.
- Lam, K.; Clarke, J.; Purkayastha, S.; Kinross, J.M. Uptake and accessibility of surgical robotics in England. Int. J. Med. Robot. 2021, 17, e2174.
- Soomro, N.A.; Hashimoto, D.A.; Porteous, A.J.; Ridley, C.J.A.; Marsh, W.J.; Ditto, R.; Roy, S. Systematic review of learning curves in robot-assisted surgery. BJS Open 2020, 4, 27–44.
- Davies, B.L.; Hibberd, R.D.; Coptcoat, M.J.; Wickham, J.E.A. A surgeon robot prostatectomy—A laboratory evaluation. J. Med. Eng. Technol. 1989, 13, 273–277.
- Sung, G.T.; Gill, I.S. Robotic laparoscopic surgery: A comparison of the da Vinci and Zeus systems. J. Urol. 2001, 58, 893–898.
- Berguer, R.; Forkey, D.L.; Smith, W.D. The effect of laparoscopic instrument working angle on surgeons’ upper extremity workload. Surg. Endosc. 2001, 15, 1027–1029.
- Barakat, B.; Othman, H.; Gauger, U.; Wolff, I.; Hadaschik, B.; Rehme, C. Retzius Sparing Radical Prostatectomy Versus Robot-assisted Radical Prostatectomy: Which Technique Is More Beneficial for Prostate Cancer Patients (MASTER Study)? A Systematic Review and Meta-analysis. Eur. Urol. Focus 2022, 8, 1060–1071.
- Lantz, A.; Bock, D.; Akre, O.; Angenete, E.; Bjartell, A.; Carlsson, S.; Modig, K.K.; Nyberg, M.; Kollberg, K.S.; Steineck, G.; et al. Functional and Oncological Outcomes After Open Versus Robot-assisted Laparoscopic Radical Prostatectomy for Localised Prostate Cancer: 8-Year Follow-up. Eur. Urol. 2021, 80, 650–660.
- Ngu, J.C.; Tsang, C.B.; Koh, D.C. The da Vinci Xi: A review of its capabilities, versatility, and potential role in robotic colorectal surgery. Robot Surg. 2017, 4, 77–85.
- Agarwal, D.K.; Sharma, V.; Toussi, A.; Viers, B.R.; Tollefson, M.K.; Gettman, M.T.; Frank, I. Initial Experience with da Vinci Single-port Robot-assisted Radical Prostatectomies. Eur. Urol. 2020, 77, 373–379.
- Kim, J.E.; Kaldany, A.; Lichtbroun, B.; Singer, E.A.; Jang, T.L.; Ghodoussipour, S.; Kim, M.M.; Kim, I.Y. Single-Port Robotic Radical Prostatectomy: Short-Term Outcomes and Learning Curve. J. Endourol. 2022, 36, 1285–1289.
- Covas Moschovas, M.; Bhat, S.; Rogers, T.; Onol, F.; Roof, S.; Mazzone, E.; Mottrie, A.; Patel, P. Technical Modifications Necessary to Implement the da Vinci Single-port Robotic System. Eur. Urol. 2020, 78, 415–423.
- Hinojosa-Gonzalez, D.E.; Roblesgil-Medrano, A.; Torres-Martinez, M.; Alanis-Garza, C.; Estrada-Mendizabal, R.J.; Gonzalez-Bonilla, E.A.; Flores-Villalba, E.; Olvera-Posada, D. Single-port versus multiport robotic-assisted radical prostatectomy: A systematic review and meta-analysis on the da Vinci SP platform. Prostate 2022, 82, 405–414.
- CMR Surgical. CMR Presskit. Available online: https://cmrsurgical.com/press-kit (accessed on 23 February 2023).
- Thomas, B.C.; Slack, M.; Hussain, M.; Barber, N.; Pradhan, A.; Dinneen, E.; Stewart, G.D. Preclinical Evaluation of the Versius Surgical System, a New Robot-assisted Surgical Device for Use in Minimal Access Renal and Prostate Surgery. Eur. Urol. Focus 2021, 7, 444–452.
- Alkatout, I.; Salehiniya, H.; Allahqoli, L. Assessment of the Versius Robotic Surgical System in Minimal Access Surgery: A Systematic Review. J. Clin. Med. 2022, 11, 3754.
- CMR Surgical. CMR Surgical Announces more than 100 Versius Systems Installed Globally. Available online: https://cmrsurgical.com/wp-content/uploads/2022/11/English-PDF.pdf (accessed on 22 November 2022).
- Venckus, R.; Jasenas, M.; Telksnys, T.; Venckus, M.; Janusonis, V.; Dulskas, A.; Samalavicius, N.E. Robotic-assisted radical prostatectomy with the Senhance® robotic platform: Single center experience. World J. Urol. 2021, 39, 4305–4310.
- Kastelan, Z.; Hudolin, T.; Kulis, T.; Knezevic, N.; Penezic, L.; Maric, M.; Zekulic, T. Upper urinary tract surgery and radical prostatectomy with Senhance® robotic system: Single center experience-First 100 cases. Int. J. Med. Robot. 2021, 17, e2269.
- Alip, S.; Koukourikis, P.; Han, W.K.; Rha, K.H.; Na, J.C. Comparing Revo-i and da Vinci in Retzius-Sparing Robot-Assisted Radical Prostatectomy: A Preliminary Propensity Score Analysis of Outcomes. J. Endourol. 2022, 36, 104–110.
- Sarchi, L.; Mottaran, A.; Bravi, C.A.; Paciotti, M.; Farinha, R.; Piazza, P.; Puliatti, S.; De Groote, R.; De Naeyer, G.; Gallagher, A.; et al. Robot-assisted radical prostatectomy feasibility and setting with the Hugo™ robot-assisted surgery system. BJU Int. 2022, 130, 671–675.
- Bravi, C.A.; Paciotti, M.; Sarchi, L.; Mottaran, A.; Nocera, L.; Farinha, R.; De Backer, P.; Vinckier, M.H.; De Naeyer, G.; D’Hondt, F.; et al. Robot-assisted Radical Prostatectomy with the Novel Hugo Robotic System: Initial Experience and Optimal Surgical Set-up at a Tertiary Referral Robotic Center. Eur. Urol. 2022, 82, 233–237.
- Totaro, A.; Campetella, M.; Bientinesi, R.; Gandi, C.; Palermo, G.; Russo, A.; Aceto, P.; Bassi, P.; Sacco, E. The new surgical robotic platform HUGOTMRAS: System description and docking settings for robot-assisted radical prostatectomy. Urologia 2022, 89, 603–609.
- Avateramedical. Avatera system. Available online: https://www.avatera.eu/en/avatera-system (accessed on 23 February 2023).
- Peteniaris, A.; Kallidonis, P.; Tsaturyan, A.; Pagonis, K.; Faitatziadis, S.; Gkeka, K.; Vagionis, A.; Natsos, A.; Obaidat, M.; Anaplioti, E.; et al. The feasibility of robot-assisted radical cystectomy: An experimental study. World J. Urol. 2023, 41, 477–482.
- Gkeka, K.; Tsaturyan, A.; Faitatziadis, S.; Peteinaris, A.; Anaplioti, E.; Pagonis, K.; Vagionis, A.; Tatanis, V.; Vrettos, T.; Kallidonis, P.; et al. Robot-Assisted Radical Nephrectomy Using the Novel Avatera Robotic Surgical System: A Feasibility Study in a Porcine Model. J. Endourol. 2022. online ahead of print.
- Distalmotion. Distalmotion Dexter. Available online: https://www.distalmotion.com/product/ (accessed on 24 November 2022).
- Distalmotion. First Dexter Surgeries in Urology Carried Out in Bern. Available online: https://www.distalmotion.com/first-dexter-surgeries-in-urology/ (accessed on 24 November 2022).
- Whooley, S. Ottava Surgical Assistant Robot Finally Unveiled by Johnson and Johnson. Available online: www.therobotreport.com/ottava-surgical-assistant-robot-finally-unveiled-by-johnson-johnson (accessed on 24 November 2022).
- Suntharasivam, T.; Mukherjee, A.; Luk, A.; Aboumarzouk, O.; Somani, B.; Rai, B.P. The role of robotic surgery in the management of renal tract calculi. Transl. Androl. Urol. 2019, 8 (Suppl. S4), S457–S460.
- Murgu, S.D. Robotic assisted-bronchoscopy: Technical tips and lessons learned from the initial experience with sampling peripheral lung lesions. BMC Pulm. Med. 2019, 19, 89.
- Chi, T.; Hathaway, L.; Chok, R.; Stoller, M. MP15-09 Robotic-Assisted Percutaneous Nephrolithotomy and Ureteroscopy with the Monarch® Platform, Urology Compares Favorably Against Conventional Techniques. Abstracts of the 39th World Congress of Endourology: WCE 2022. J. Endourol. 2022, 36 (Suppl. S1), A1–A315.
- Mohan, A.; Wara, U.; Arshad Shaikh, M.; Rahman, R.M.; Zaidi, Z.A. Telesurgery and Robotics: An Improved and Efficient Era. Cureus 2021, 13, e14124.
- Marescaux, J.; Leroy, J.; Gagner, M.; Rubino, F.; Mutter, D.; Vix, M.; Butner, S.E.; Smith, M.K. Transatlantic robot-assisted telesurgery. Nature 2001, 413, 379–380.
This entry is offline, you can click here to edit this entry!
