Cancer is one of the major public health issues in the world. It has become the second leading cause of death, with approximately 75% of cancer deaths transpiring in low- or middle-income countries. It causes a heavy global economic cost estimated at more than a trillion dollars per year. The conventional diagnostic technologies such as MRI (magnetic resonance imaging), CT (computerized tomography) scan, ultrasound and biopsy were not effective for cancer detection at primary stages; this is because of their dependency on tumorigenic properties or phenotypic characters of a tumor. Cancer is a very complex disease, with many epigenetic as well as genetic modifications which might alter the cell signaling process, related to development and resulting in tumorigenic transformation and malignancy. For almost all cancer patients, researchers and clinicians expect tests or methods that might diagnose cancer significantly earlier, provide better prognosis, and that can allow for increased survival rates. Cancer markers have been used in the oncology field. Biomarkers are molecules of biologic emergence found in blood, tissues, various body fluids such as urine, cerebrospinal fluid, or different body tissues that are elevated is the indicative of an abnormal disease or condition with cancer.
- Cancer Biomarkers
- Cancer Diagnosis
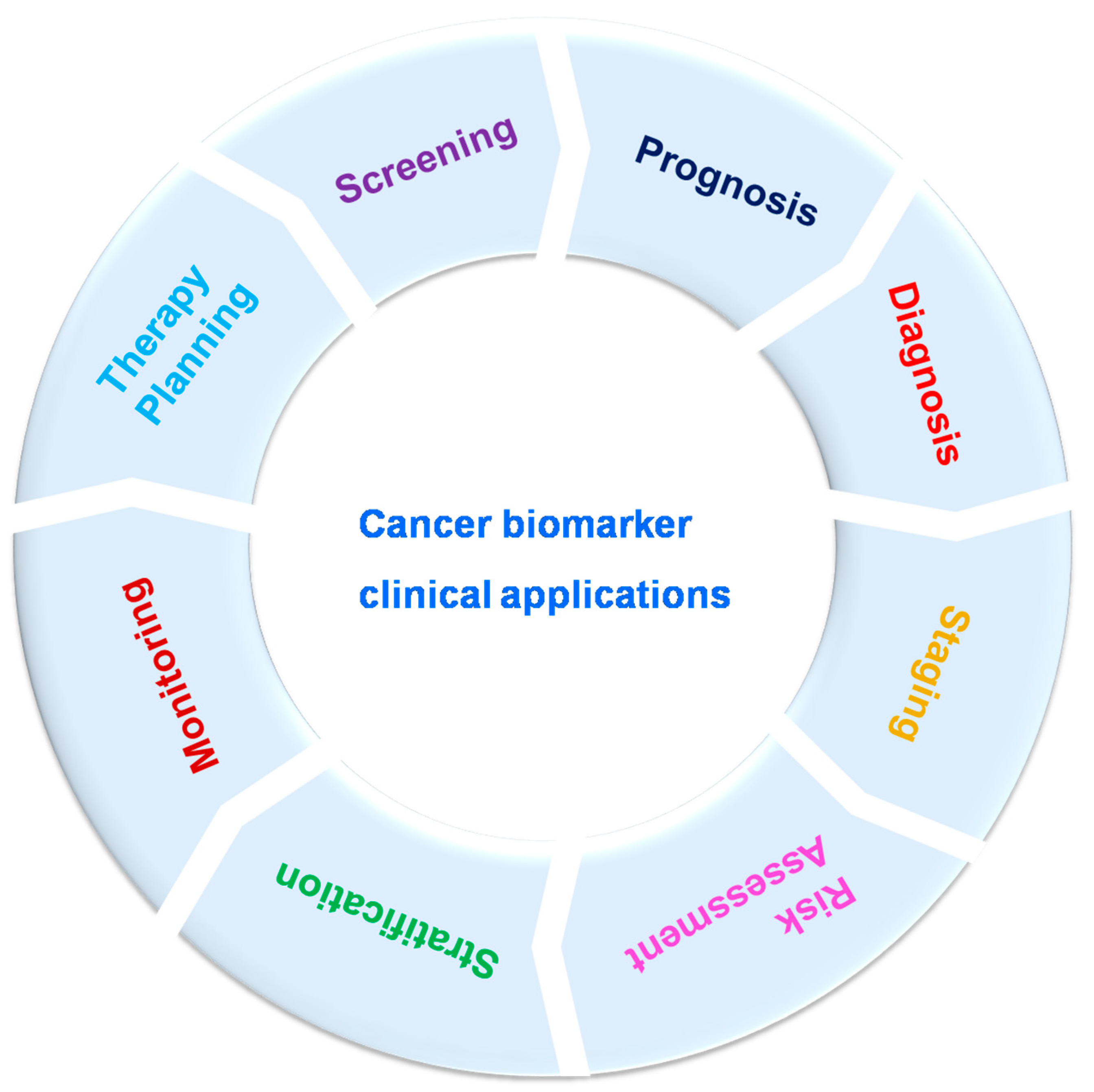
1. Clinical Significance of Cancer Biomarkers
2. Identification of Novel Cancer Biomarkers
3. Cancer Biomarkers Currently Used in Clinical Settings
3.1. AFP (Alpha-Fetoprotein)
3.2. PSA (Prostate Specific Antigen)
3.3. RCAS1 (Receptor-Binding Cancer Antigen)
3.4. CA 15-3 (Cancer Antigen 15-3)
3.5. Cancer–Testis (CT) Antigens
3.6. CA 125
3.7. CA 19-9
3.8. Nse (Neuron-Specific Enolase)
3.9. Tdt (Terminal Deoxynucleotidyl Transferase)
3.10. CYFRA21-1
This entry is adapted from the peer-reviewed paper 10.3390/bios13030398
References
- Jayanthi, V.S.A.; Das, A.B.; Saxena, U. Recent Advances in Biosensor Development for the Detection of Cancer Biomarkers. Biosens. Bioelectron. 2017, 91, 15–23.
- Chowdhury, S.G.; Ray, R.; Karmakar, P. Exosomal miRNAs—a diagnostic biomarker acting as a guiding light in the diagnosis of prostate cancer. Funct. Integr. Genom. 2023, 23, 23.
- Henry, N.L.; Hayes, D.F. Cancer Biomarkers. Mol. Oncol. 2012, 6, 140–146.
- Somerfield, M.R. Clinical Practice Guidelines for the Use of Tumor Markers in Breast and Colorectal Cancer. Adopted on May 17, 1996 by the American Society of Clinical Oncology. J. Clin. Oncol. 1996, 14, 2843–2877.
- Meindl, A. Comprehensive Analysis of 989 Patients with Breast or Ovarian Cancer Provides BRCA1 and BRCA2 Mutation Profiles and Frequencies for the German Population. Int. J. Cancer 2002, 97, 472–480.
- Easton, D.F.; Ford, D.; Bishop, D.T.; Haites, N.; Milner, B.; Allan, L.; Easton, D.F.; Ponder, B.A.J.; Peto, J.; Smith, S.; et al. Breast and Ovarian Cancer Incidence in BRCA1-Mutation Carriers. Breast Cancer Linkage Consortium. Am. J. Hum. Genet. 1995, 56, 265.
- Grossman, D.C.; Curry, S.J.; Owens, D.K.; Bibbins-Domingo, K.; Caughey, A.B.; Davidson, K.W.; Doubeni, C.A.; Ebell, M.; Epling, J.W.; Kemper, A.R.; et al. Screening for Prostate Cancer USPreventive Services task force recommendation Statement. JAMA-J. Am. Med. Assoc. 2018, 319, 1901–1913.
- Lin, K.; Lipsitz, R.; Miller, T.; Janakiraman, S. Benefits and Harms of Prostate-Specific Antigen Screening for Prostate Cancer: An Evidence Update for the U.S. Preventive Services Task Force. Ann. Intern. Med. 2008, 149, 192–199.
- Calonge, N.; Petitti, D.B.; Dewitt, T.G.; Dietrich, A.J.; Gregory, K.D.; Harris, R.; Isham, G.J.; Lefevre, M.L.; Leipzig, R.; Loveland-Cherry, C.; et al. Screening for Prostate Cancer: U.S. Preventive Services Task Force Recommendation Statement. Ann. Intern. Med. 2008, 149, 185–191.
- Van’t Veer, L.J.; Paik, S.; Hayes, D.F. Gene Expression Profiling of Breast Cancer: A New Tumor Marker. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2005, 23, 1631–1635.
- Paik, S.; Shak, S.; Tang, G.; Kim, C.; Baker, J.; Cronin, M.; Baehner, F.L.; Walker, M.G.; Watson, D.; Park, T.; et al. A Multigene Assay to Predict Recurrence of Tamoxifen-Treated, Node-Negative Breast Cancer. N. Engl. J. Med. 2004, 351, 2817–2826.
- Cohen, J. Detection and Localization of Surgically Resectable Cancers with a Multi-Analyte Blood Test. Science 2018, 359, 926–930.
- Cristofanilli, M.; Budd, G.T.; Ellis, M.J.; Stopeck, A.; Matera, J.; Miller, M.C.; Reuben, J.M.; Doyle, G.V.; Allard, W.J.; Terstappen, L.W.M.M.; et al. Circulating Tumor Cells, Disease Progression, and Survival in Metastatic Breast Cancer. N. Engl. J. Med. 2004, 351, 781–791.
- Zhao, Q.; Li, B.; Gao, Q.; Luo, Y.; Ming, L. Prognostic Value of Epithelial-Mesenchymal Transition Circulating Tumor Cells in Female Breast Cancer: A Meta-Analysis. Front. Oncol. 2022, 12, 1024783.
- Abe, S.; Kawai, K.; Nozawa, H.; Sasaki, K.; Murono, K.; Emoto, S.; Ozawa, T.; Yokoyama, Y.; Nagai, Y.; Anzai, H.; et al. Clinical Impact of Primary Tumor Sidedness and Sex on Unresectable Post-Recurrence Survival in Resected Pathological Stage II-III Colorectal Cancers: A Nationwide Multicenter Retrospective Study. BMC Cancer 2022, 22, 1–10.
- Allegra, C.J.; Jessup, J.M.; Somerfield, M.R.; Hamilton, S.R.; Hammond, E.H.; Hayes, D.F.; McAllister, P.K.; Morton, R.F.; Schilsky, R.L. American Society of Clinical Oncology Provisional Clinical Opinion: Testing for KRAS Gene Mutations in Patients with Metastatic Colorectal Carcinoma to Predict Response to Anti-Epidermal Growth Factor Receptor Monoclonal Antibody Therapy. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2009, 27, 2091–2096.
- Thuss-Patience, P.C.; Shah, M.A.; Ohtsu, A.; Van Cutsem, E.; Ajani, J.A.; Castro, H.; Mansoor, W.; Chung, H.C.; Bodoky, G.; Shitara, K.; et al. Trastuzumab Emtansine versus Taxane Use for Previously Treated HER2-Positive Locally Advanced or Metastatic Gastric or Gastro-Oesophageal Junction Adenocarcinoma (GATSBY): An International Randomised, Open-Label, Adaptive, Phase 2/3 Study. Lancet Oncol. 2017, 18, 640–653.
- Bang, Y.J.; Van Cutsem, E.; Feyereislova, A.; Chung, H.C.; Shen, L.; Sawaki, A.; Lordick, F.; Ohtsu, A.; Omuro, Y.; Satoh, T.; et al. Trastuzumab in Combination with Chemotherapy versus Chemotherapy Alone for Treatment of HER2-Positive Advanced Gastric or Gastro-Oesophageal Junction Cancer (ToGA): A Phase 3, Open-Label, Randomised Controlled Trial. Lancet 2010, 376, 687–697.
- Sawaki, M.; Taira, N.; Uemura, Y.; Saito, T.; Baba, S.; Kobayashi, K.; Kawashima, H.; Tsuneizumi, M.; Sagawa, N.; Bando, H.; et al. Adjuvant Trastuzumab without Chemotherapy for Treating Early HER2-Positive Breast Cancer in Older Patients: A Propensity Score-Adjusted Analysis of a Prospective Cohort Study. Breast 2022, 66, 245–254.
- Piccart-Gebhart, M.J.; Procter, M.; Leyland-Jones, B.; Goldhirsch, A.; Untch, M.; Smith, I.; Gianni, L.; Baselga, J.; Bell, R.; Jackisch, C.; et al. Trastuzumab after Adjuvant Chemotherapy in HER2-Positive Breast Cancer. N. Engl. J. Med. 2005, 353, 1659–1672.
- Perez, E.A.; Ballman, K.V.; Tenner, K.S.; Thompson, E.A.; Badve, S.S.; Bailey, H.; Baehner, F.L. Association of Stromal Tumor-Infiltrating Lymphocytes with Recurrence-Free Survival in the N9831 Adjuvant Trial in Patients with Early-Stage HER2-Positive Breast Cancer. JAMA Oncol. 2016, 2, 56–64.
- Romond, E.H.; Perez, E.A.; Bryant, J.; Suman, V.J.; Geyer, C.E.; Davidson, N.E.; Tan-Chiu, E.; Martino, S.; Paik, S.; Kaufman, P.A.; et al. Trastuzumab plus Adjuvant Chemotherapy for Operable HER2-Positive Breast Cancer. N. Engl. J. Med. 2005, 353, 1673–1684.
- Liu, J.; Gan, M.; Lin, Z.; Deng, Q.; Deng, J.; Zeng, B.; Shi, Y.; Ming, J. Clinical Features and Prognosis Analysis of Hormone Receptor-Positive, HER2-Negative Breast Cancer with Differential Expression Levels of Estrogen and Progesterone Receptors: A 10-Year Retrospective Study. Breast J. 2022, 2022, 5469163.
- Abe, O.; Abe, R.; Enomoto, K.; Kikuchi, K.; Koyama, H.; Masuda, H.; Nomura, Y.; Ohashi, Y.; Sakai, K.; Sugimachi, K.; et al. Relevance of Breast Cancer Hormone Receptors and Other Factors to the Efficacy of Adjuvant Tamoxifen: Patient-Level Meta-Analysis of Randomised Trials. Lancet 2011, 378, 771–784.
- Teutsch, S.M.; Bradley, L.A.; Palomaki, G.E.; Haddow, J.E.; Piper, M.; Calonge, N.; Dotson, W.D.; Douglas, M.P.; Berg, A.O. The Evaluation of Genomic Applications in Practice and Prevention (EGAPP) Initiative: Methods of the EGAPP Working Group. Genet. Med. Off. J. Am. Coll. Med. Genet. 2009, 11, 3–14.
- Hanash, S.M.; Pitteri, S.J.; Faca, V.M. Mining the Plasma Proteome for Cancer Biomarkers. Nature 2008, 452, 571–579.
- Mighton, C.; Shickh, S.; Aguda, V.; Krishnapillai, S.; Adi-Wauran, E.; Bombard, Y. From the Patient to the Population: Use of Genomics for Population Screening. Front. Genet. 2022, 13, 893832.
- Kohsaka, S.; Tada, Y.; Ando, M.; Nakaguro, M.; Shirai, Y.; Ueno, T.; Kojima, S.; Hirai, H.; Saigusa, N.; Kano, S.; et al. Identification of Novel Prognostic and Predictive Biomarkers in Salivary Duct Carcinoma via Comprehensive Molecular Profiling. Npj Precis. Oncol. 2022, 6, 82.
- Wang, N.; Zhang, H.; Li, D.; Jiang, C.; Zhao, H.; Teng, Y. Identification of Novel Biomarkers in Breast Cancer via Integrated Bioinformatics Analysis and Experimental Validation. Bioengineered 2021, 12, 12431.
- Wu, M.; Li, Q.; Wang, H. Identification of Novel Biomarkers Associated with the Prognosis and Potential Pathogenesis of Breast Cancer via Integrated Bioinformatics Analysis. Technol. Cancer Res. Treat. 2021, 20, 1533033821992081.
- Li, C.-J.; Lin, L.-T.; Chu, P.-Y.; Chiang, A.-J.; Tsai, H.-W.; Chiu, Y.-H.; Huang, M.-S.; Wen, Z.-H.; Tsui, K.-H.; Li, C.-J.; et al. Identification of Novel Biomarkers and Candidate Drug in Ovarian Cancer. J. Pers. Med. 2021, 11, 316.
- Islam, S.U.; Ahmed, M.B.; Ahsan, H.; Lee, Y.S. Role of Biomarkers in Personalized Medicine. In Cancer Biomarkers in Diagnosis and Therapeutics; Springer: Singapore, 2022; pp. 249–275.
- Janjua, K.A.; Shahzad, R.; Shehzad, A. Development of Novel Cancer Biomarkers for Diagnosis and Prognosis. In Cancer Biomarkers in Diagnosis and Therapeutics; Springer: Singapore, 2022; pp. 277–343.
- Bohunicky, B.; Mousa, S.A. Biosensors: The New Wave in Cancer Diagnosis. Nanotechnol. Sci. Appl. 2011, 4, 1–10.
- Nikanjam, M.; Kato, S.; Kurzrock, R. Liquid Biopsy: Current Technology and Clinical Applications. J. Hematol. Oncol. 2022, 15, 1–14.
- Altintas, Z.; Tothill, I. Biomarkers and Biosensors for the Early Diagnosis of Lung Cancer. Sens. Actuators B Chem. 2013, 188, 988–998.
- Tothill, I.E. Biosensors for Cancer Markers Diagnosis. Semin. Cell Dev. Biol. 2009, 20, 55–62.
- Prabhakar, B.; Shende, P.; Augustine, S. Current Trends and Emerging Diagnostic Techniques for Lung Cancer. Biomed. Pharmacother. 2018, 106, 1586–1599.
- Chen, M.; Wu, D.; Tu, S.; Yang, C.; Chen, D.J.; Xu, Y. A Novel Biosensor for the Ultrasensitive Detection of the LncRNA Biomarker MALAT1 in Non-Small Cell Lung Cancer. Sci. Rep. 2021, 11, 3666.
- Reddy, K.K.; Bandal, H.; Satyanarayana, M.; Goud, K.Y.; Gobi, K.V.; Jayaramudu, T.; Amalraj, J.; Kim, H. Recent Trends in Electrochemical Sensors for Vital Biomedical Markers Using Hybrid Nanostructured Materials. Adv. Sci. 2020, 7, 1902980.
- Ferraro, S.; Bussetti, M.; Bassani, N.; Rossi, R.S.; Incarbone, G.P.; Bianchi, F.; Maggioni, M.; Runza, L.; Ceriotti, F.; Panteghini, M. Definition of Outcome-Based Prostate-Specific Antigen (PSA) Thresholds for Advanced Prostate Cancer Risk Prediction. Cancers 2021, 13, 3381.
- Thompson, I.M.; Ankerst, D.P. Prostate-Specific Antigen in the Early Detection of Prostate Cancer. CMAJ Can. Med. Assoc. J. 2007, 176, 1853–1858.
- Wu, M.; Liu, H.; Liu, Z.; Liu, C.; Zhang, A.; Li, N. Analysis of Serum Alpha-Fetoprotein (AFP) and AFP-L3 Levels by Protein Microarray. J. Int. Med. Res. 2018, 46, 4297–4305.
- Yuan, Q.; Song, J.; Yang, W.; Wang, H.; Huo, Q.; Yang, J.; Yu, X.; Liu, Y.; Xu, C.; Bao, H. The Effect of CA125 on Metastasis of Ovarian Cancer: Old Marker New Function. Oncotarget 2017, 8, 50015–50022.
- Meyer, T.; Rustin, G.J. Role of Tumour Markers in Monitoring Epithelial Ovarian Cancer. Br. J. Cancer 2000, 82, 1535–1538.
- Chianca, M.; Panichella, G.; Fabiani, I.; Giannoni, A.; L’Abbate, S.; Aimo, A.; Del Franco, A.; Vergaro, G.; Grigoratos, C.; Castiglione, V.; et al. Bidirectional Relationship Between Cancer and Heart Failure: Insights on Circulating Biomarkers. Front. Cardiovasc. Med. 2022, 9, 936654.
- Tuxen, M.K.; Sölétormos, G.; Dombernowsky, P. Tumor Markers in the Management of Patients with Ovarian Cancer. Cancer Treat. Rev. 1995, 21, 215–245.
- Smith, D.S.; Humphrey, P.A.; Catalona, W.J. The Early Detection of Prostate Carcinoma with Prostate Specific Antigen: The Washington University Experience. Cancer 1997, 80, 1852–1856.
- Bill-Axelson, A.; Holmberg, L.; Ruutu, M.; Häggman, M.; Andersson, S.-O.; Bratell, S.; Spångberg, A.; Busch, C.; Nordling, S.; Garmo, H.; et al. Radical Prostatectomy versus Watchful Waiting in Early Prostate Cancer. N. Engl. J. Med. 2005, 352, 1977–1984.
- Jaffee, E.M.; Van Dang, C.; Agus, D.B.; Alexander, B.M.; Anderson, K.C.; Ashworth, A.; Barker, A.D.; Bastani, R.; Bhatia, S.; Bluestone, J.A.; et al. Future Cancer Research Priorities in the USA: A Lancet Oncology Commission. Lancet Oncol. 2017, 18, e653–e706.
- National Cancer Institute. Prostate-Specific Antigen (PSA) Test—NCI; National Cancer Institute: Bethesda, MD, USA, 2022.
- Kim, J.H.; Suh, Y.J.; Park, D.; Yim, H.; Kim, H.; Kim, H.J.; Yoon, D.S.; Hwang, K.S. Technological Advances in Electrochemical Biosensors for the Detection of Disease Biomarkers. Biomed. Eng. Lett. 2021, 11, 309–334.
- Dutsch-Wicherek, M.; Tomaszewska, R.; Lazar, A.; Wicherek, L.; Skladzien, J. The Association between RCAS1 Expression in Laryngeal and Pharyngeal Cancer and Its Healthy Stroma with Cancer Relapse. BMC Cancer 2009, 9, 35.
- Kazmierczak, W.; Lazar, A.; Tomaszewska, R.; Popiela, T.J.; Koper, K.; Wicherek, L.; Dutsch-Wicherek, M. Analysis of the Intensity of Immune Cell Infiltration and Immunoreactivity of RCAS1 in Diffuse Large B-Cell Lymphoma of the Palatine Tonsil and Its Microenvironment. Cell Tissue Res. 2015, 361, 823–831.
- Kubokawa, M.; Nakashima, M.; Yao, T.; Ito, K.I.; Harada, N.; Nawata, H.; Watanabe, T. Aberrant Intracellular Localization of RCAS1 Is Associated with Tumor Progression of Gastric Cancer. Int. J. Oncol. 2001, 19, 695–700.
- Naito, Y.; Okabe, Y.; Nagayama, M.; Nishinakagawa, T.; Taira, T.; Kawahara, A.; Hattori, S.; MacHida, K.; Ishida, Y.; Kaji, R.; et al. Accuracy of Differential Diagnosis for Pancreatic Cancer Is Improved in the Combination of RCAS1 and CEA Measurements and Cytology in Pancreatic Juice. Med. Mol. Morphol. 2011, 44, 86–92.
- Duffy, M.J. Serum Tumor Markers in Breast Cancer: Are They of Clinical Value? Clin. Chem. 2006, 52, 345–351.
- Hasan, D. Diagnostic Impact of CEA and CA 15-3 on Chemotherapy Monitoring of Breast Cancer Patients. J. Circ. Biomark. 2022, 11, 57–63.
- Tampellini, M.; Berruti, A.; Gerbino, A.; Buniva, T.; Torta, M.; Gorzegno, G.; Faggiuolo, R.; Cannone, R.; Farris, A.; Destefanis, M.; et al. Relationship between CA 15-3 Serum Levels and Disease Extent in Predicting Overall Survival of Breast Cancer Patients with Newly Diagnosed Metastatic Disease. Br. J. Cancer 1997, 75, 698–702.
- Lian, M.; Zhang, C.; Zhang, D.; Chen, P.; Yang, H.; Yang, Y.; Chen, S.; Hong, G. The Association of Five Preoperative Serum Tumor Markers and Pathological Features in Patients with Breast Cancer. J. Clin. Lab. Anal. 2019, 33, e22875.
- Bast, J.; Ravdin, P.; Hayes, D.F.; Bates, S.; Fritsche, H.J.; Jessup, J.M.; Kemeny, N.; Locker, G.Y.; Mennel, R.G.; Somerfield, M.R. 2000 Update of Recommendations for the Use of Tumor Markers in Breast and Colorectal Cancer: Clinical Practice Guidelines of the American Society of Clinical Oncology. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2001, 19, 1865–1878.
- Lin, M.J.; Svensson-Arvelund, J.; Lubitz, G.S.; Marabelle, A.; Melero, I.; Brown, B.D.; Brody, J.D. Cancer Vaccines: The next Immunotherapy Frontier. Nat. Cancer 2022, 3, 911–926.
- Chow, S.; Berek, J.S.; Dorigo, O. Development of Therapeutic Vaccines for Ovarian Cancer. Vaccines 2020, 8, 657.
- Jäger, E.; Chen, Y.T.; Drijfhout, J.W.; Karbach, J.; Ringhoffer, M.; Jäger, D.; Arand, M.; Wada, H.; Noguchi, Y.; Stockert, E.; et al. Simultaneous Humoral and Cellular Immune Response against Cancer-Testis Antigen NY-ESO-1: Definition of Human Histocompatibility Leukocyte Antigen (HLA)-A2-Binding Peptide Epitopes. J. Exp. Med. 1998, 187, 265–270.
- Tsuji, K.; Hamada, T.; Uenaka, A.; Wada, H.; Sato, E.; Isobe, M.; Asagoe, K.; Yamasaki, O.; Shiku, H.; Ritter, G.; et al. Induction of Immune Response against NY-ESO-1 by CHP-NY-ESO-1 Vaccination and Immune Regulation in a Melanoma Patient. Cancer Immunol. Immunother. 2008, 57, 1429–1437.
- Jäger, E.; Stockert, E.; Zidianakis, Z.; Chen, Y.T.; Karbach, J.; Jäger, D.; Arand, M.; Ritter, G.; Old, L.J.; Knuth, A. Humoral Immune Responses of Cancer Patients against “Cancer-Testis” Antigen NY-ESO-1: Correlation with Clinical Events. Int. J. Cancer 1999, 84, 506–510.
- Karbach, J.; Neumann, A.; Atmaca, A.; Wahle, C.; Brand, K.; Von Boehmer, L.; Knuth, A.; Bender, A.; Ritter, G.; Old, L.J.; et al. Efficient in Vivo Priming by Vaccination with Recombinant NY-ESO-1 Protein and CpG in Antigen Naive Prostate Cancer Patients. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2011, 17, 861–870.
- Stockert, E.; Jäger, E.; Chen, Y.T.; Scanlan, M.J.; Gout, I.; Karbach, J.; Arand, M.; Knuth, A.; Old, L.J. A Survey of the Humoral Immune Response of Cancer Patients to a Panel of Human Tumor Antigens. J. Exp. Med. 1998, 187, 1349–1354.
- Imai, N.; Ikeda, H.; Shiku, H. . Nihon Rinsho. Jpn. J. Clin. Med. 2012, 70, 2125–2129.
- Raza, A.; Merhi, M.; Inchakalody, V.P.; Krishnankutty, R.; Relecom, A.; Uddin, S.; Dermime, S. Unleashing the Immune Response to NY-ESO-1 Cancer Testis Antigen as a Potential Target for Cancer Immunotherapy. J. Transl. Med. J. Transl. Med. 2020, 18, 1–11.
- Patel, J.; Patel, P. Biosensors and Biomarkers: Promising Tools for Cancer Diagnosis. Int. J. Biosens. Bioelectron. 2017, 3, 00072.
- Babaier, A.; Mal, H.; Alselwi, W.; Ghatage, P. Low-Grade Serous Carcinoma of the Ovary: The Current Status. Diagnostics 2022, 12, 458.
- Neesham, D. Ovarian Cancer Screening. Aust. Fam. Physician 2007, 36, 126–128.
- Menon, U.; Gentry-Maharaj, A.; Hallett, R.; Ryan, A.; Burnell, M.; Sharma, A.; Lewis, S.; Davies, S.; Philpott, S.; Lopes, A.; et al. Sensitivity and Specificity of Multimodal and Ultrasound Screening for Ovarian Cancer, and Stage Distribution of Detected Cancers: Results of the Prevalence Screen of the UK Collaborative Trial of Ovarian Cancer Screening (UKCTOCS). Lancet Oncol. 2009, 10, 327–340.
- Wong, N.K.; Easton, R.L.; Panico, M.; Sutton-Smith, M.; Morrison, J.C.; Lattanzio, F.A.; Morris, H.R.; Clark, G.F.; Dell, A.; Patankar, M.S. Characterization of the Oligosaccharides Associated with the Human Ovarian Tumor Marker CA125. J. Biol. Chem. 2003, 278, 28619–28634.
- White, B.; Patterson, M.; Karnwal, S.; Brooks, C.L. Crystal Structure of a Human MUC16 SEA Domain Reveals Insight into the Nature of the CA125 Tumor Marker. Proteins Struct. Funct. Bioinform. 2022, 90, 1210–1218.
- Wang, Y.-S.; Ren, S.-F.; Jiang, W.; Lu, J.-Q.; Zhang, X.-Y.; Li, X.-P.; Cao, R.; Xu, C.-J. CA125-Tn ELISA Assay Improves Specificity of Pre-Operative Diagnosis of Ovarian Cancer among Patients with Elevated Serum CA125 Levels. Ann. Transl. Med. 2021, 9, 788.
- Seelenmeyer, C.; Wegehingel, S.; Lechner, J.; Nickel, W. The Cancer Antigen CA125 Represents a Novel Counter Receptor for Galectin-1. J. Cell Sci. 2003, 116, 1305–1318.
- Liang, L.; Fang, J.; Han, X.; Zhai, X.; Song, Y.; Lu, Y.; Zhang, Q.; Ma, R. Prognostic Value of CEA, CA19-9, CA125, CA724, and CA242 in Serum and Ascites in Pseudomyxoma Peritonei. Front. Oncol. 2021, 11, 594763.
- Li, B.; Li, Y.; Li, C.; Yang, J.; Liu, D.; Wang, H.; Xu, R.; Zhang, Y.; Wei, Q. An ultrasensitive split-type electrochemical immunosensor based on controlled-release strategy for detection of CA19-9. Biosens. Bioelectron. 2023, 227, 115180.
- Poruk, K.E.; Firpo, M.A.; Adler, D.G.; Mulvihill, S.J. Screening for Pancreatic Cancer: Why, How, and Who? Ann. Surg. 2013, 257, 17–26.
- Badheeb, M.; Abdelrahim, A.; Esmail, A.; Umoru, G.; Abboud, K.; Al-Najjar, E.; Rasheed, G.; Alkhulaifawi, M.; Abudayyeh, A.; Abdelrahim, M. Pancreatic Tumorigenesis: Precursors, Genetic Risk Factors and Screening. Curr. Oncol. 2022, 29, 8693–8719.
- Hatzakis, K.D.; Froudarakis, M.E.; Bouros, D.; Tzanakis, N.; Karkavitsas, N.; Siafakas, N.M. Prognostic Value of Serum Tumor Markers in Patients with Lung Cancer. Respiration 2002, 69, 25–29.
- Ferrigno, D.; Buccheri, G.; Giordano, C. Neuron-Specific Enolase Is an Effective Tumour Marker in Non-Small Cell Lung Cancer (NSCLC). Lung Cancer 2003, 41, 311–320.
- Gazdar, A.F.; Carney, D.N.; Nau, M.M.; Minna, J.D. Characterization of Variant Subclasses of Cell Lines Derived from Small Cell Lung Cancer Having Distinctive Biochemical, Morphological, and Growth Properties. Cancer Res. 1985, 45, 2924–2930.
- Isgrò, M.A.; Bottoni, P.; Scatena, R. Neuron-Specifi c Enolase as a Biomarker: Biochemical and Clinical Aspects. Adv. Exp. Med. Biol. 2015, 867, 125–143.
- Tian, Z.; Liang, C.; Zhang, Z.; Wen, H.; Feng, H.; Ma, Q.; Liu, D.; Qiang, G. Prognostic Value of Neuron-Specific Enolase for Small Cell Lung Cancer: A Systematic Review and Meta-Analysis. World J. Surg. Oncol. 2020, 18, 1–8.
- Campagnari, F.; Bombardieri, E.; de Braud, F.; Baldini, L.; Maiolo, A.T. Terminal Deoxynucleotidyl Transferase, Tdt, as a Marker for Leukemia and Lymphoma Cells. Int. J. Biol. Markers 1987, 2, 31–42.
- Peng, Y.; Shang, H.; Zheng, Z.; Li, H.; Chen, W.; Xu, J. Self-activation of symbiotic multi-DNA machines transducing exponentially amplified fluorescence for ultrasensitively signaling of terminal deoxynucleotidyl transferase activity. Sens. Actuators B. Chem 2023, 380, 133400.
- Sur, M.; AlArdati, H.; Ross, C.; Alowami, S. TdT Expression in Merkel Cell Carcinoma: Potential Diagnostic Pitfall with Blastic Hematological Malignancies and Expanded Immunohistochemical Analysis. Mod. Pathol. 2007, 20, 1113–1120.
- Mathewson, R.C.; Kjeldsberg, C.R.; Perkins, S.L. Detection of Terminal Deoxynucleotidyl Transferase (TdT) in Nonhematopoietic Small Round Cell Tumors of Children. Pediatr. Pathol. Lab. Med. J. Soc. Pediatr. Pathol. Affil. Int. Paediatr. Pathol. Assoc. 1997, 17, 835–844.
- Chapman, M.H.; Sandanayake, N.S.; Andreola, F.; Dhar, D.K.; Webster, G.J.; Dooley, J.S.; Pereira, S.P. Circulating CYFRA 21-1 Is a Specific Diagnostic and Prognostic Biomarker in Biliary Tract Cancer. J. Clin. Exp. Hepatol. 2011, 1, 6–12.
- Zhang, L.; Liu, D.; Li, L.; Pu, D.; Zhou, P.; Jing, Y.; Yu, H.; Wang, Y.; Zhu, Y.; He, Y.; et al. The Important Role of Circulating CYFRA21-1 in Metastasis Diagnosis and Prognostic Value Compared with Carcinoembryonic Antigen and Neuron-Specific Enolase in Lung Cancer Patients. BMC Cancer 2017, 17, 96.
- Dal Bello, M.G.; Filiberti, R.A.; Alama, A.; Orengo, A.M.; Mussap, M.; Coco, S.; Vanni, I.; Boccardo, S.; Rijavec, E.; Genova, C.; et al. The Role of CEA, CYFRA21-1 and NSE in Monitoring Tumor Response to Nivolumab in Advanced Non-Small Cell Lung Cancer (NSCLC) Patients. J. Transl. Med. 2019, 17, 74.
- Rapellino, M.; Niklinski, J.; Pecchio, F.; Furman, M.; Baldi, S.; Chyczewski, L.; Ruffini, E.; Chyczewska, E. CYFRA 21-1 as a Tumour Marker for Bronchogenic Carcinoma. Eur. Respir. J. 1995, 8, 407–410.
- Dall’Olio, F.G.; Abbati, F.; Facchinetti, F.; Massucci, M.; Melotti, B.; Squadrilli, A.; Buti, S.; Formica, F.; Tiseo, M.; Ardizzoni, A. CEA and CYFRA 21-1 as Prognostic Biomarker and as a Tool for Treatment Monitoring in Advanced NSCLC Treated with Immune Checkpoint Inhibitors. Ther. Adv. Med. Oncol. 2020, 12, 1758835920952994.
