Cancer is one of the major public health issues in the world. It has become the second leading cause of death, with approximately 75% of cancer deaths transpiring in low- or middle-income countries. It causes a heavy global economic cost estimated at more than a trillion dollars per year. The conventional diagnostic technologies such as MRI (magnetic resonance imaging), CT (computerized tomography) scan, ultrasound and biopsy were not effective for cancer detection at primary stages; this is because of their dependency on tumorigenic properties or phenotypic characters of a tumor. Cancer is a very complex disease, with many epigenetic as well as genetic modifications which might alter the cell signaling process, related to development and resulting in tumorigenic transformation and malignancy. For almost all cancer patients, researchers and clinicians expect tests or methods that might diagnose cancer significantly earlier, provide better prognosis, and that can allow for increased survival rates. Cancer markers have been used in the oncology field. Biomarkers are molecules of biologic emergence found in blood, tissues, various body fluids such as urine, cerebrospinal fluid, or different body tissues that are elevated is the indicative of an abnormal disease or condition with cancer.
1. Clinical Significance of Cancer Biomarkers
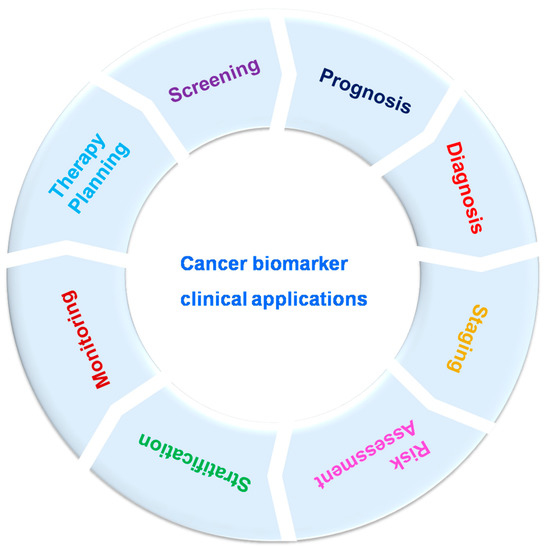
Cancer biomarkers can be utilized for cancer patient evaluation in different clinical levels, as well as disease screening, prognosis, diagnosis, staging, risk assessment, stratification, therapy planning and monitoring (
Figure 2). Still, to date, several cancer markers have indicated poor validity and efficacy, especially in the most widespread cancers such as lung and breast cancers. Cancer biomarkers are bio-molecules necessary for remodeling throughout cancer which maintain excessive clinical relevance. These can be enzymes, iso-enzymes, nucleic acids, proteins, metabolites. Biomarkers are classified into three types based on their clinical advantage: prognostic, predictive and diagnostic. Prognostic biomarkers provide details about course of recurrence of the disease; patient response to the treatment is estimated by predictive biomarkers; disease detection can be performed by using diagnostic biomarkers [
43,
47,
48,
49]. The difference in the level of any unique biomarker in a cell or tissue is often used as evidence of tumor expansion. Biomarkers also play potential role in differentiating benign and malignant tumors and one type of malignancy from another type; specific biomarkers are helpful in unique settings, other biomarkers can be involved in multiple settings [
48]. Biomarkers might be helpful to estimate a person’s chance of developing tumors/cancer. For example, a person having a solid family network (via ancestors) with ovarian cancer might receive a genetic test to decide whether they are acting as a carrier for a specific germ line modification or mutation, such as BRCA1, which could cause potential chance of developing breast and/or ovarian cancer [
50,
51]. Biomarkers might be helpful to determine malignancy in fit populations. A frequently utilized component for screening is PSA (prostate-specific antigen). It was approved by Food and Drug Administration (FDA) in 1986. Enhanced screening in male population above 50 years old lead to growth in the identification of prostate cancer. These kinds of traditional biomarkers also have limitations. In the previous decade, U.S. Preventive Services Task Force survey noted that an adequate documentation for common diagnosis with PSA [
52,
53,
54]. Biomarkers were used to monitor prognosis and possibility of cancer reappearance irrespective of therapy/treatment. The clinical and pathological properties of a tumor could be useful for the prediction of cancers. Recently, modern techniques were used to evaluate prognosis of independent tumors; for example, a large number of genetic marks that had been matured in breast cancer might be useful to evaluate the identification for an individual patient depending on tumor assessment [
55,
56]. During breast cancer (metastatic) condition, circulating tumor cells are indicative of overall survival [
57,
58,
59]. Biomarkers could be utilized as stimulus changers or prognostic factors for unique type of therapy, as well as to select the effective type of treatment. KRAS is a predictive biomarker for colorectal cancer; mutations occurring to KRAS in somatic cells are related to low response to anti-EGFR-mediated treatment [
60,
61]. Likewise, HER2 over-expression in the breast cancer as well as gastric cancer anticipates for stimulus to anti-Her2 drugs such as trastuzumab [
62,
63,
64,
65,
66,
67], and over-expression of estrogen receptor anticipates for stimulus to anti-endocrine therapy or treatment such as tamoxifen in breast cancer [
68,
69]. Identification of novel cancer biomarkers might help in quick and efficient diagnosis as well as monitoring of cancer progression.
Figure 2. Cancer biomarker clinical applications.
2. Identification of Novel Cancer Biomarkers
Possible cancer biomarkers could be recognized through various approaches. An excellent way to recognize novel biomarkers mostly depends on biological nature of tumor and nearby environment of a tumor or metabolism of the drugs or biological products. With most recent studies and new information related to cancers and appearance of latest technology, cancer biomarker detection is performed frequently these days with applying a discovery approach. In this approach, few major areas of research such as gene expression arrays, proteomic technologies (mass spectroscopy, LC-MS/MS, MALDI-MS), and high throughput sequencing can be used to rapidly recognize unique biomarkers or pool of biomarkers which can show difference in the middle of cohorts. Expansion of sophisticated software algorithms for large data analysis has emerged in rapid advancement in the identification of novel cancer biomarkers. Openly available software programs can sort these data and compare the sequences to annotated genome databases to permit quantitative comparative evaluation of proteomes from multiple sources such as tumor area and nearby healthy tissues. Thus, over-expressed or down-regulated proteins in a cancer cell can be identified as putative cancer biomarkers. Huge amount of data produced with these technological methods mean that special attention needs to be directed toward both developing a study plan and conducting a large data analysis. Moreover, it is crucial to reduce the possibility of detecting relationships that are eventually determined to provide false-positive results. The most crucial features of biomarker improvement and identification to consider in depth include mindful study pattern to minimize any kind of bias, extensive evaluation, validation, and accurate communication of the results [
48,
70,
71,
72,
73,
74,
75,
76,
77,
78,
79].
3. Cancer Biomarkers Currently Used in Clinical Settings
A cancer biomarker is a molecule existing inside and/or generated by tumor cells or surrounding cells in tissues or organs in stimulus to tumor or certain noncancerous (benign) situations, which can provide information about cancer, mostly which stage it is, whether it can respond to treatment, and what type of therapy might be useful. Here, few recent cancer biomarkers used in clinical practice are explained. New cancer biomarkers become available continuously, and they may not be explained below [
27,
40,
44,
80,
81,
82].
3.1. AFP (Alpha-Fetoprotein)
AFP (Alpha-fetoprotein) is one of the leading biomarker. Early fetal life of a baby (mostly yolk sac and liver) produces AFP during pregnancy. AFP can be detected in huge amounts in serum of the patients with specific tumors. According to Yuri Semenovich Tatarinov, AFP was first accepted as an antigen unique for human HCC (hepatocellular carcinoma) [
83,
84]. The scientific literature has explained that AFPs are classified into subtypes based on their dissimilar affinities to LCA (lens culinaris agglutinin), such as AFP-L1 (LCA unreactive AFP), AFP-L2 (LCA mild active AFP) and AFP-L3 (LCA active AFP). In healthy individual serum, an average level of AFP is less than 20 ng 8 mL
−1 [
85,
86,
87]. AFP is widely established for HCC (hepatocellular carcinoma) diagnosis. Moreover, in congenital tyrosinemia, cirrhosis, hepatitis (alcohol-induced), hepatitis (viral-induced), ataxia-telangiectasia syndrome or in several malignancies such as testicular cancer, liver cancer, gastric cancer and nasopharyngeal cancer elevated AFP levels may also be present. Hence, sensing the AFP values is completely mandatory in clinical settings. High recognition rates of molecular assays have been obtained in quantitative observation of AFP due to their specificity and unalterable affinity of the probes to molecular targets [
88,
89].
3.2. PSA (Prostate Specific Antigen)
PSA (prostate-specific antigen) was one of the first recognized cancer biomarkers, utilized to detect and screen prostate cancer in clinical setting. It has been shown that increased levels of PSA can directly relate to prostate cancer. Human regular PSA level is 4 ng/mL. According to the study by Smith et. al, almost 30% of individuals with PSA values higher than normal (range of 4.1–9.9 ng/mL) were diagnosed with prostate cancer [
90]. Along with this, raised PSA values may also indicate benign tumors (non-fatal), prostatitis/prostate inflammation or benign prostatic hyperplasia. Therefore, elevated values of PSA may not consistently suggest malignant tumors. There is a fact that caused reasonable controversy about using regular PSA screening to detect prostate cancer. Small-sized tumors identified by PSA screening may grow very slowly; death caused by small tumor might not be feasible in an individual lifetime. Moreover, it is very expensive to treat such slow-growing tumors. Other frequent issue with PSA screening is false-positives. This limitation of PSA testing can be overcome by modern biosensing technology mediated by biosensors [
79,
84,
91,
92,
93]. PSA detection can be performed by various methods; these traditional methods are time-consuming as well as expensive. Yang et al. explained a graphene oxide/ssDNA-based biosensor integrated with dual antibody-modified PLLA NPs to amplify electrochemical signals for the effective and rapid electrochemical capture of PSA in serum samples from prostate cancer patients. The detection limit for PSA was 1 ng/mL, which achieved a wide linear range of 1–100 ng/mL for PSA. This is one of the examples that shows the usefulness of modern biosensing technology mediated by biosensors [
94].
3.3. RCAS1 (Receptor-Binding Cancer Antigen)
RCAS1 (receptor-binding cancer antigen) overexpression data has been described in many gastric carcinomas; it is related with progression of gastric cancer. Further, RCAS1 is also suggested as a cancer biomarker for poor prediction in breast, esophageal, endometrial, bladder cancers and is associated with tumor weakening in pharyngeal carcinoma and laryngeal cancer. RCAS overexpression is observed in several types of cancers. Thus, it serves as a potential biomarker for cancer detection and prediction [
95,
96,
97,
98].
3.4. CA 15-3 (Cancer Antigen 15-3)
The most predominant cancer marker for breast cancer identification as well as monitoring is cancer antigen 15-3; additional biomarkers that are related to breast cancer are CA 27.29, BRCA1, BRCA2 and (carcinoembryonic antigen) CEA [
44,
99,
100]. This particular marker is frequently used on a clinical level to monitor the therapy for breast cancer in its advanced stages. During breast cancer, CA 15-3 values increased by 10, 20, 30 and 40 % at various stages first, second, third and fourth stage [
49]. Tampellini et. al showed the connection between breast cancer and CA 15-3 levels, also mentioning that before treatment, patients with levels of 30U/mL had notably higher survival rate compared to patients with higher values. Raised CA 15-3 values correspond with extensive metastasis [
101,
102]. Other research data explained that raised CA 15-3 levels post cancer treatment can be a sign of disease recurrence. Nowadays, to determine breast cancer treatment, protocol CA 15-3 values are considered along with risk factors (negative) such as PR/ER condition as well as iHer-2, cancer stage and tumor dimension. Hepatitis, endometriosis, pelvic inflammatory disease, lactation and pregnancy are conditions other than cancer where CA 15-3 levels are increased [
103].
3.5. Cancer–Testis (CT) Antigens
Cancer–testis antigens are a specific type of cancer biomarkers. They are expressed in various cancers. CT antigen expression is limited to male germ cells of the testis but not shown in normal adult cells. These antigens are also expressed in trophoblast and ovary cells. Therefore, CT antigens have been considered as possible immunogenic targets for cancer vaccines (cancer immunotherapies). CT antigen autoantibodies have been studied as potential cancer biomarkers [
104]. NY-ESO-1 (NewYorkesophagealsquamouscellcarcinoma1) is encoded by
CTAG-1B; this is the class of antigens with high immunogenic nature which induces very robust cellular and humoral immune response in NY-ESO-1-positive cancers. Antibody titer to NY-ESO-1 has been shown to relate with disease progression. One of the best benefits of using CT autoantibodies as tumor biomarkers is the fact that they are easy to obtain and are also more stable proteins present in serum compared to tissues obtained via biopsy. Thus, they can be useful for cancer progression and recurrence [
105,
106,
107,
108,
109]. Major limitation of CT antigens is the fact that many cancers express CT antigens, and they are rarely tumor-specific. Biosensor technology can obtain a profile for CT antigen, which can enhance the use of these antigens in cancer prognosis and diagnosis [
110,
111,
112].
3.6. CA 125
The rise in CA 125 levels is primarily related to ovarian cancer. It is further correlated with several different cancers such as cervix, lungs, breast, liver, pancreas, uterus, stomach and colon cancers. Enhanced levels of CA 125 are also observed in various non-pathological conditions such as menstruation and pregnancy [
8,
87,
113]. A total of 90% of women with advanced stage ovarian cancer and 40% of humans with intra-abdominal malignant tumors also exhibit high CA 125 levels. Still, approximately 50% of patients diagnosed with primary stage ovarian cancer show normal CA 125 levels [
87,
88,
89]. Other germ cell origin biomarkers such as alpha-fetoprotein/AFP, human chorionic gonadotrophin/HCG as well as Lactate dehydrogenase/LDH are also connected to ovarian cancer [
114,
115]. Increase in CA 125 levels can be used to detect the development of benign tumors into malignant tumors. Enhanced CA 125 levels are also used to identify treatment failure as well as disease recurrence (e.g., high CA 125 levels after bilateral salpingo-oophorectomy or total abdominal hysterectomy, which may occur after first line chemotherapy) [
116,
117,
118,
119,
120]. Altogether, CA 125 is an extremely essential biomarker for detection of cancer, and also for cancer progression monitoring and treatment.
3.7. CA 19-9
This antigen was first identified in pancreatic and colon cancer patient’s serum in 1981. It is a Lewis antigen of the MUC1 glycoprotein [
8,
121]. CA 19-9 normal level in serum is less than 37 U/mL. In the recent decade, on a clinical level, CA 19-9 biomarker has become extremely useful for the diagnosis of pancreatic cancer. Normal human serum CA 19-9 levels can play an outstanding role in clinical diagnosis of urothelial and gastric cancers [
122,
123]. Consequently, there is a necessity to improve highly sensitive methods which can detect CA 19-9 values in patients with cancer.
3.8. Nse (Neuron-Specific Enolase)
This neuron-specific enolase is a popular and unique marker for SCLC as well as NSCLC non-small cell lung cancer. It has a crucial role in glycolysis; in 1980s, NSE expression was noted in SCLC cells. From that time, it has been used as potential biomarker for lung cancer, able to detect increased values of NSCLC and acting as crucial predictor for patient survival (it is not dependent on remaining prognostic factors) [
124,
125,
126]. NSE is also a unique marker for neuro-endocrine cells. Raised NSE values in body fluids might be an indication of tumor proliferation and staging determination in some of brain tumors [
127,
128]. In the recent decade, the value of NSE for prognosis in cancer patients is debatable. Therefore, it is mandatory to improve sensitive techniques to perceive Nse values in patients with cancer.
3.9. Tdt (Terminal Deoxynucleotidyl Transferase)
Tdt is an intracellular marker which has detected in the bone marrow as well as blood (mononucleate) cells in leukemia patients during diagnosis. Overall, TdT values are remarkably raised in several lymphocytic lymphomas. Tdt might be helpful to identify specific leukemia type and supportive sign for the solution of therapy [
129,
130,
131,
132].
3.10. CYFRA21-1
Cytokeratin-19 fragments/CYFRA21-1 have been extensively studied in patients with NSCLC and are widely utilized as predictive, prognostic markers. They have 56% sensitivity as well as 88% specificity when the value is >1.5 ng/mL. Researchers used maximum cut off value for CYFRA21-1 similar to ≥3 ng/mL; it had shown increased specificity at 97%. It has potential capability in lung, esophagal cancer prediction. Raised values are certain but barely sensitive. These values are strongly connected with cancer metastasis. Recent reports explained that CYFRA21-1 is used as independent prediction factor for various phases of lung cancer. This might function as definitive distinction between benign and malignant lung cancer along with clinical information [
133,
134,
135,
136,
137].
This entry is adapted from the peer-reviewed paper 10.3390/bios13030398