Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Total knee arthroplasty (TKA) is widely used in clinical practice as an effective treatment for end-stage knee joint lesions. It can effectively correct joint deformities, relieve painful symptoms, and improve joint function. The reconstruction of lower extremity joint lines and soft tissue balance are important factors related to the durability of the implant; therefore, it is especially important to measure the joint lines and associated angles before TKA.
- knee osteoarthritis
- total knee arthroplasty
- AI measurement
1. Introduction
Total knee arthroplasty (TKA) is the most conclusive treatment for severe knee osteoarthritis, and its efficacy relies on the reconstruction of joint lines and soft tissue balance in the lower extremity. The reconstruction of the knee joint, among various structures in the human skeletal and soft tissue systems, is the most complex, for it requires the integration of anatomy, kinesiology, biomechanics, and even tissue engineering. In the reconstructed knee, it is important to take into account the reconstruction of joint lines, the soft tissue balance, and patellar tracking so as to achieve the “forgotten knee” status. The ultimate goal of accurate reconstruction is pursued by orthopaedic surgeons of all ages.
In order to achieve more accurate alignment, more perfect soft tissue balance, and better prosthesis matching so as to obtain longer prosthesis life, better postoperative function, and higher patient satisfaction, AI-assisted TKA preoperative design can accurately carry out preoperative planning, artificial intelligence segmentation, and key point recognition of joint CT data and establish standardized measurement model by adjusting the joint orientation. After introducing the open/closed wedge parameters or prosthesis parameters, one must accurately judge the shape parameters, such as the height and inclination of the osteotomy surface, and finally form a highly reliable surgical prediction model and simulate the postoperative image.
Therefore, thorough preoperative planning, that is, the measurement of joint lines and angles, helps guide the surgeon during the procedure. Preoperative measurements taken for TKA include traditional plain film radiographic measurements, digital templating, computer navigation, and artificial intelligence (AI) measurements. AI has multiple definitions and is largely agreed upon as the intelligence demonstrated by machines. In the field of computer science, AI research is defined as the study of “intelligent agents”, which are “devices that perceive the environment and act to maximize the achievement of a goal”. In a broad sense, process digitization, computer navigation, and robotics all fall into the category of AI. Existing AI-assisted technologies have enabled modern medicine to make great strides toward precision, intelligence, and individualization.
2. Computer Navigation Technology-Aided Measurement
In computer-assisted orthopaedic surgery, information contained in the multimodal imaging data is digitally processed and combined with stereo-navigation systems to identify and display anatomical structures. The computer plans the surgical path and formulates a surgical plan for preoperative surgical simulation under the guidance of appropriate image monitoring and stereo-navigation systems. A certain guidance system is used to perform intraoperative surgical interventions, wherein computers and medical robots assist surgeons to complete the operation. Numerous studies have confirmed that computer navigation-assisted total knee arthroplasty (TKA) can improve the accuracy of lower extremity alignment and prosthesis placement [1][2][3][4].
In the field of orthopaedics, computer-aided systems were first used in spine surgery, and Saurol et al. first developed and applied a pedicle screw navigation system in 1992. In 1993, research on knee surgical navigation systems began in France, and Sal’agaglia’s [5] group pioneered the development of a knee surgical navigation system that did not require imaging data. Consequently, in 1997, the first computer-assisted TKA was performed successfully. The earliest computer navigation systems were based on CT images and were used in clinical surgery.
Computer navigation systems can be divided into two broad categories: The first is based on imaging data (CT and MRI), wherein preoperative imaging is entered into the computer, and preoperative images based on the recorded anatomical landmarks are compared with the intraoperative morphology. The second type of navigation system does not require imaging data. Instead, it contains a large amount of anatomical data and determines the movable surface of the knee and the alteration of the biomechanical axis of the femur and tibia through passive flexion and extension activities of the knee joint [6]. The difference between the two in actual surgery is that the former facilitates more precise preoperative planning, while the latter facilitates intraoperative joint line control, soft tissue balance, and restoration of joint mobility [7].
Although computer navigation systems can improve the accuracy of joint line estimation and prosthesis placement in TKA, there are no clear studies showing that the application of computer navigation significantly improves lower extremity function after TKA. Accelerometer-based portable navigation systems, such as OrthAlign™ and iASSIST®, have the advantages of a shorter operation time, shorter learning curve, and lower cost over traditional computer navigation. The perception of spatial position is through precise accelerometers and gyroscopes, and some studies have shown that this system has significant advantages in osteotomy of the femoral condyle and tibial plateau [8][9]. Iorio et al. [10] performed TKA in 53 patients with the assistance of the accelerometer-based navigation system and showed that the tibial component of the prosthesis was aligned within 3° vertically, relative to the mechanical axis, in all patients. Nam et al. [11] also indicated that the portable navigation system was equally accurate in femoral osteotomy. In their study, measurements on 48 patients showed a mean absolute difference of (0.8 ± 0.6)° between the intraoperative goal of 0° and the actual postoperative femoral component alignment measured on radiographs, with 95.8% positioned within 2° of the intraoperative goal and 100% positioned within 3° of the intraoperative goal. However, a limitation of the iASSIST® navigation system is that it is not able to plan the type of prothesis to be used in advance and requires the surgeon to decide on the type of prothesis during the surgery using traditional surgical methods. The system requires intraoperative rotation of the limb to obtain the 13 femoral positioning points for calculating the centroid of the femoral head, which, together with other intraoperative positioning manoeuvres, takes more time than conventional surgery.
Notably, the development of novel computer navigation systems has risen markedly in recent years. The new computer navigation system, Knee 3 software, from Brainlab, Germany, was launched in China in 2020. The system comes with the advantage of simple and fast registration. It enables intraoperative visualization of osteotomy positioning and dynamic real-time display of knee flexion and extension gaps throughout the procedure, which helps the surgeon create individualized lower extremity alignment and soft tissue balance in patients. Compared with conventional computer navigation systems, Knee 3 software not only ensures accurate osteotomy but also improves the soft tissue balance in the knee joint. The Knee 3 system provides real-time intraoperative display of the joint gap in the form of gap values and gap graphs, allowing the operator to visually assess the knee flexion and extension gap balance. When planning the surgery, the surgeon can adjust the angle and position of the femoral and tibial osteotomy according to the patient’s lower extremity joint lines, and the system can also display the impact of the corresponding osteotomy changes on the joint space in real time. The disadvantage of the Knee 3 system is that it includes system setup, tracker fixation, and registration steps. Moreover, since the Knee 3 software dynamically displays the lower limb joints line and knee gap information in real time, the operator needs to quickly interpret the relevant information and devise a suitable surgical plan, which increases the operation time. In addition, because computer navigation-assisted surgery requires the installation of fixation pins to fix the tracker, there is a risk of fracture [12][13][14][15]. Smith et al. [16] reported that during computer navigation system-assisted and robot-assisted TKA, the incidence of fractures related to fixation pins was 0.06%–4.8%, and most of the fractures occurred in the femoral shaft. In recent years, AI deep learning technology has been successfully applied in the field of medical image processing, realizing automatic recognition and segmentation of the lesion or target area, and with high accuracy. AI deep learning technology was applied to independently build neural network PointRend_ Unet on the basis of ensuring the accuracy and robustness of segmentation, which realizes the fast segmentation of knee joint CT image data to improve the work efficiency and reduce the preparation cost. The segmentation results obtained by clinical evaluation are satisfactory, and the steps are as follows: First, establish a CT image database, import a large number of knee joint CT images of patients into Mimics software (Materialise Company-Technologielaan 15, Heverlee, Leuven, Flemish, Belgium), reconstruct the bone structure according to the bone threshold setting on the basis of the threshold method, select the target bone structure, and then conduct threshold growth segmentation; then, conduct manual trimming, and finally, save the data in mask format. Secondly, the neural network is built and trained. Through the segmentation of the neural network, the knee joint CT image data form the femur, tibia, fibula, and patella regions, respectively. Finally, the visualization of the target bone structure 3D model is generated through 3D reconstruction technology. Although non-imaging mode and ultrasound and other non-radiation exposure technologies are emerging, the new TKA auxiliary technology commonly used in clinical practice is based mainly on CT images, which extract the three-dimensional anatomical model of the knee joint from the patient’s CT images for subsequent surgical planning. The manual processing of CT image data is time-consuming and laborious. The realization of simplified, automatic, and accurate segmentation of knee joint CT image is the key to the wide range clinical application of TKA new auxiliary technology. The development of artificial intelligence technology has led to the development and research of a large number of medical image automatic segmentation systems. The commonly used neural networks are deeplab or Unet. These methods have effectively improved the stability of automatic segmentation and the efficiency of the treatment plan workflow.
3. Patient-Specific Instrumentation Measurement Technology
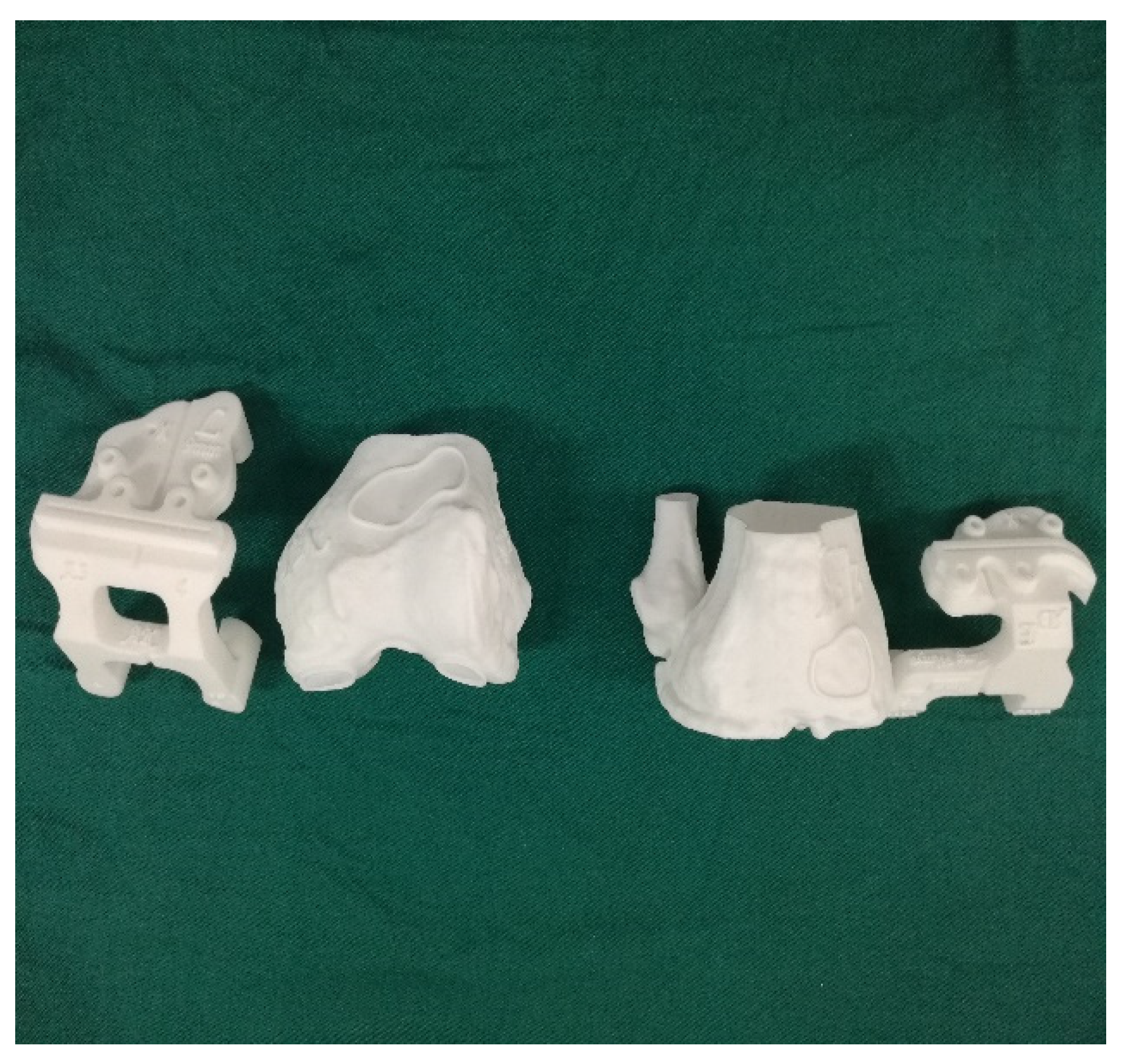
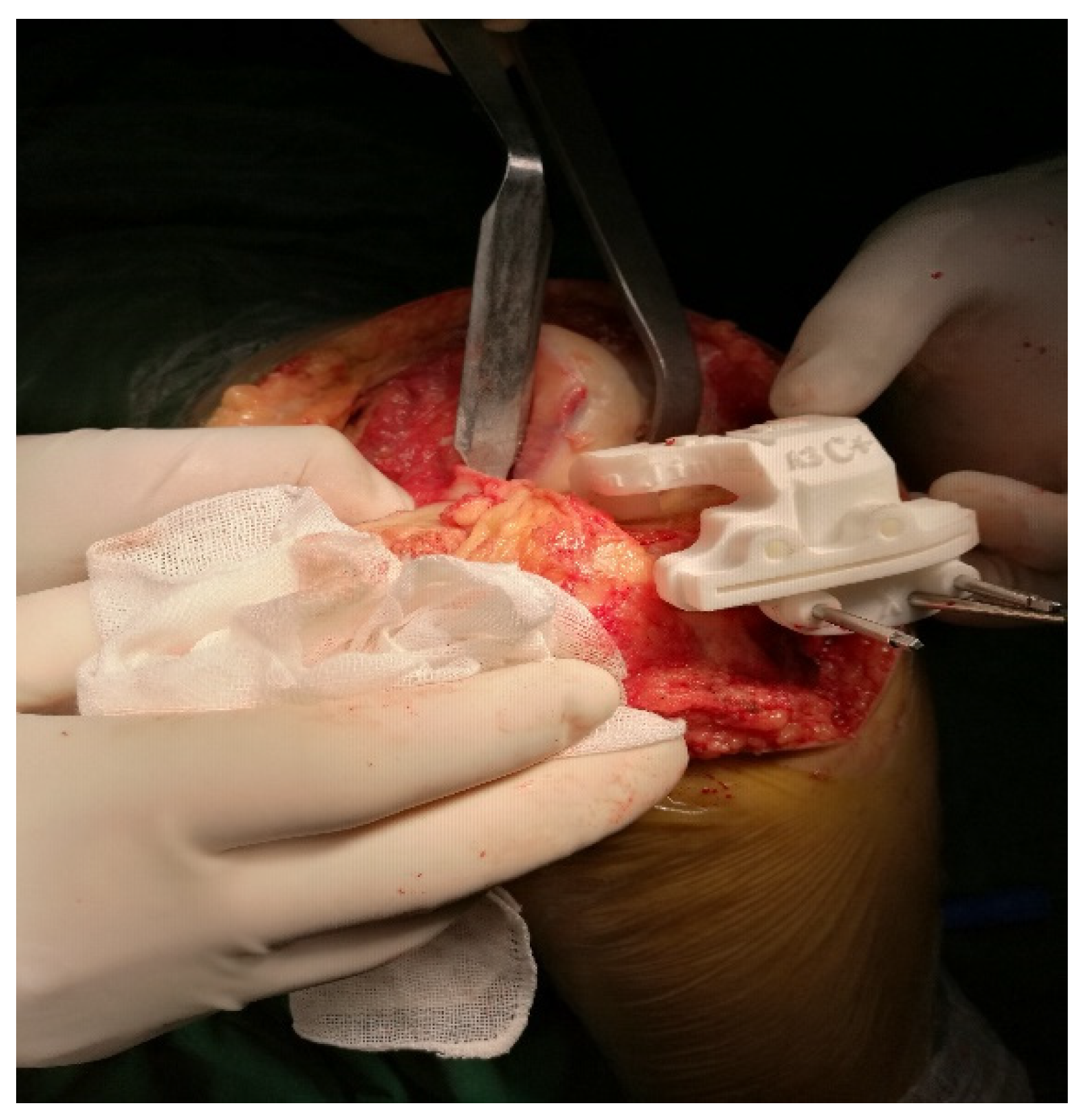
Some scholars do not support the inclusion of patient-specific instrumentation (PSI) under the category of artificial intelligence, though some scholars do not agree with this view. PSI also requires data on the hip joint, knee joint, and ankle joint of the patient to be obtained through CT imaging, which are then digitally processed. The two-dimensional data are reconstructed into a 3D model, and then the corresponding osteotomy volume, angle, and prosthesis type are determined. After planning, the PSI is automatically generated, and the personalized osteotomy surgical guide is obtained via 3D printing technology (Figure 1 and Figure 2).
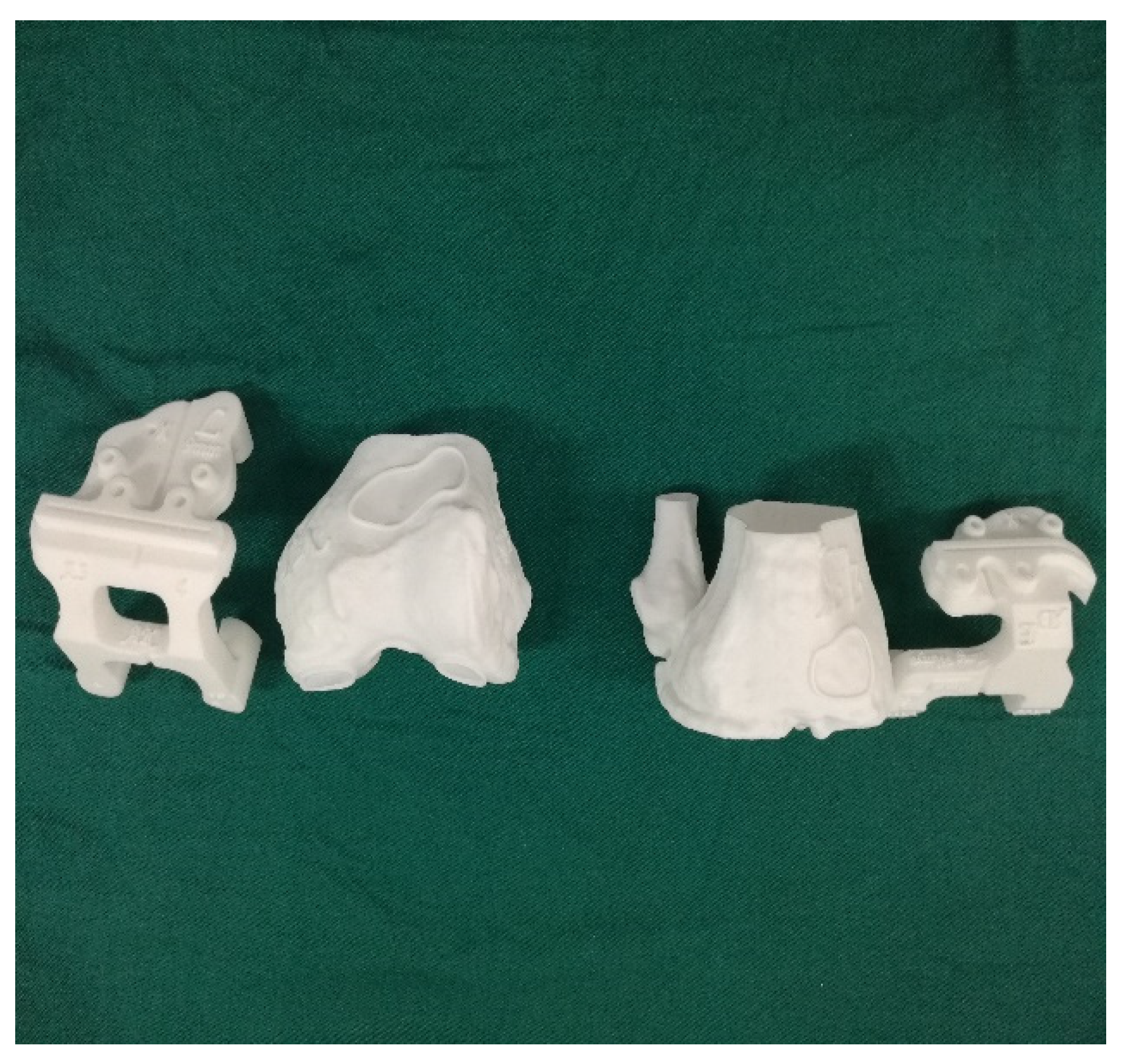
Figure 1. 3D printing pre-operative template.
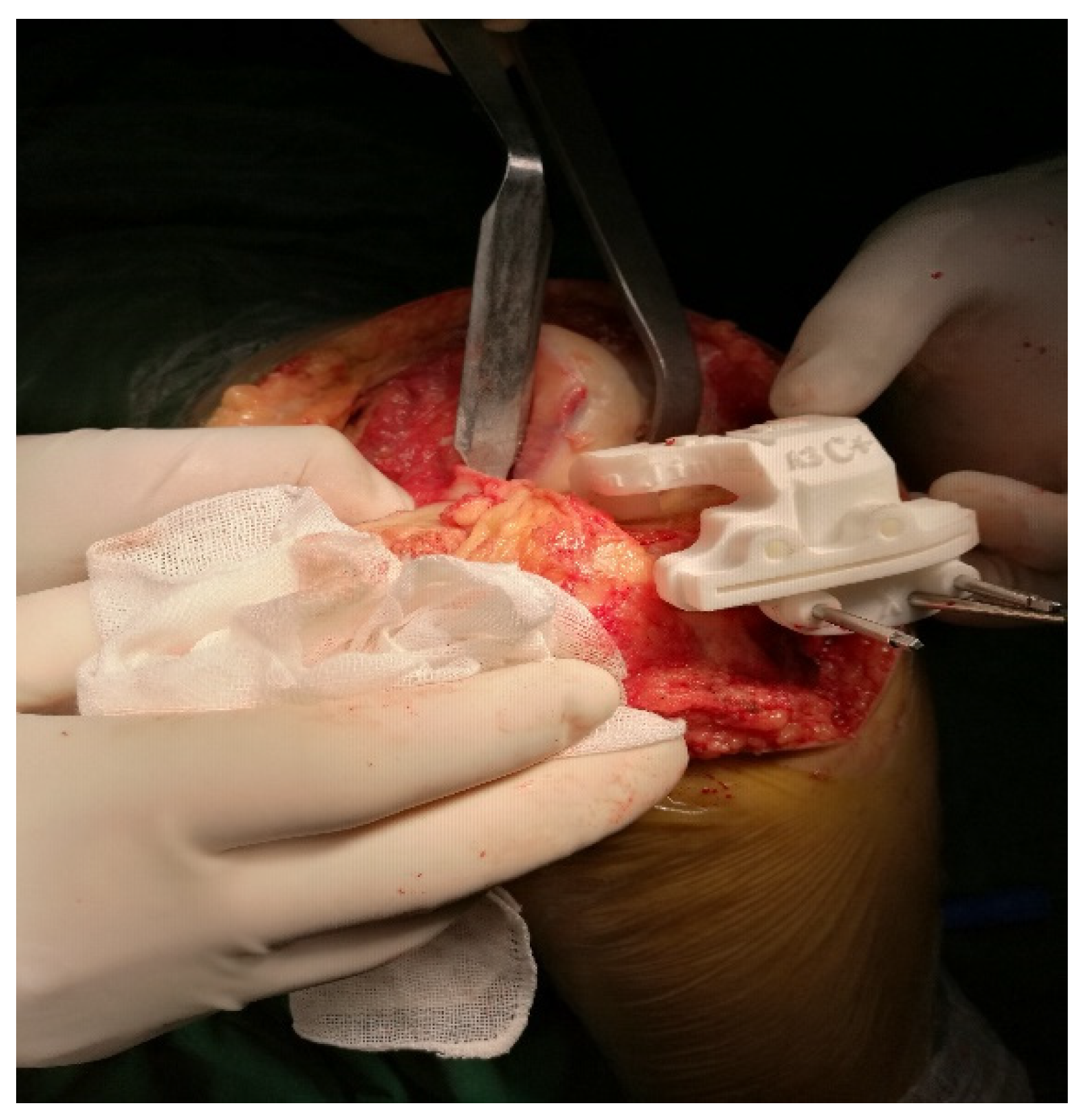
Figure 2. Intraoperative application of 3D printing template.
Several studies have shown that the use of 3D-printed osteotomy guides can achieve favourable lower limb force lines during TKA [17][18], shorten the operation time, and achieve good results in controlling the femoral component rotation and tibial slope [19][20][21] and pre-operative planning of the required prosthesis type. However, TKA with PSI takes into account only the osteotomy aspect, while the soft tissue release and balance need to be controlled by the surgeons on the basis of their surgical experience. The PSI is based on CT and on bony landmarks. Intraoperatively, however, the guide may be inaccurately attached due to soft tissue coverage or obscuration. The future of this technique involves the inclusion of nuclear magnetic imaging.
4. Preoperative Planning of Robot-Assisted TKA
Before robot-assisted total knee arthroplasty, the AIHIP/KNEE software system was used in the preoperative planning of hip arthroplasty or knee arthroplasty. The system applies computer 3D data analysis based on CT or MRI, applies computer depth learning algorithm to segment joint CT data and identify key points, establishes a standardized measurement model, and then introduces prosthesis parameters to accurately judge parameters, such as osteotomy plane height and posterior inclination angle.
Institutions performing robotic research in China and abroad have explored the introduction of robotic surgery in arthroplasty, and the use of robot-assisted TKA systems is an historic moment. Robot-assisted TKA is currently the highest-level embodiment of artificial intelligence (AI) in knee surgery.
AI technology was once limited by basic hardware, barren databases, deficits of algorithms, and so on.
Alan Turing first invented artificial intelligence in 1950. He established the Turing test, which is the earliest prototype of AI. Turing proposed that the concept of AI technology is a computer algorithm similar to human brain intelligence, but at the same time, its complexity and efficiency are no less than or even higher than human brain intelligence. At that time, due to the backwardness of basic hardware equipment, poor databases, lack of algorithms, and other limitations, the development of AI technology was basically at a standstill. However, in recent years, the rapid development of computer technology and Internet technology has brought about the improvement of computer hardware, computing power, and large databases; thus, intelligent algorithms, such as machine learning, reinforcement learning and deep learning have gradually emerged, which have ushered in the great-leap-forward development of AI technology and produced several macro technical directions, such as computer vision, speech recognition, natural language recognition, decision planning, and big data analysis. Great breakthroughs have been made in the intelligent identification, understanding, and decision-making of data. During this period, many scholars published important works on AI, and the important scientific discoveries in the development process of AI embodied important historical significance.
Robot-assisted preoperative planning system includes mainly high-precision 3D reconstruction based on CT and MRI images, image-based determination of preoperative osteotomy area and osteotomy plane, joint prosthesis design and preparation, preoperative joint line measurement, biomechanical analysis of the knee joint after prosthesis implantation, and so on. Current robotic systems can be divided into three categories according to their working modes: active, semi-active, and passive.
The active robot does not require manual operation and operates according to the preoperative plan. However, the system has potential surgical risks, and its working process needs to be monitored by the doctor throughout to avoid accidents. The semi-active robot, also called the haptic robot, is used to perform surgical planning before the operation, and during the operation, the surgeon completes the operation with the help of the robotic arm. Moreover, if the intraoperative osteotomy exceeds the preoperative planning range, the system gives feedback to the surgeon by means of a sound and force feedback, and the robotic arm automatically stops the operation, thus ensuring that the surgical path and the range are consistent with those planned preoperatively [22][23].
It is generally accepted that excellent long-term postoperative results can be obtained when the postoperative knee varus or valgus is controlled within 3° after TKA surgery, but most of the current coronal lower extremity joint lines are controlled by relying on femoral intramedullary positioning and tibial extramedullary positioning. Further, the operation depends on the surgeon’s experience, which makes it difficult to achieve standardization and reproducibility of surgical outcomes. As can be seen from the above, the gradual deepening of the study of artificial intelligence has brought revolutionary changes in medicine, and concurrently, the preoperative planning of total knee arthroplasty in joint surgery is also moving towards the paradigm of precision medicine.
This entry is adapted from the peer-reviewed paper 10.3390/life13020451
References
- Du, H.; Zhang, J.; Tang, H.; Lv, M.; Zhou, Y.X. Observation on the effect of computer-assisted navigation artificial knee arthroplasty. Shandong Med. 2014, 54, 74–77.
- Mason, J.B.; Fehring, T.K.; Estok, R.; Banel, D.; Fahrbach, K. Meta-analysis of alignment outcomes in computer-assisted total knee arthroplasty surgery. J. Arthroplast. 2007, 22, 1097–1106.
- Cheng, T.; Zhang, G.; Zhang, X. Imageless navigation system does not improve component rotational alignment in total knee arthroplasty. J. Surg. Res. 2011, 171, 590–600.
- Zhao, L.; Xu, F.; Lao, S.; Zhao, J.; Wei, Q. Comparison of the clinical effects of computer-assisted and traditional techniques in bilateral total knee arthroplasty: A meta-analysis of randomized controlled trials. PLoS ONE 2020, 15, e0239341.
- Stiehl, J.B.; Konermann, W.H.; Haaker, R.G.; Saragaglia, D.; Picard, F. Computer-assisted implantation of total knee endoprosthesis with no preoperative imaging: The kinematic model. Navig. Robot. Total Jt. Spine Surg. 2004, 22, 226–233.
- Eric, J.H. Computer-assisted orthopaedic surgery: A new paradigm. Tech. Orthop. 2003, 18, 221–229.
- Fehring, T.K.; Mason, J.B.; Moskal, J.; Pollock, D.C.; Mann, J.; Williams, V.J. When computer-assisted knee replacement is the best alternative. Clin. Orthop. Relat. Res. 2006, 452, 132–136.
- Thiengwittayaporn, S.; Fusakul, Y.; Kangkano, N.; Jarupongprapa, C.; Charoenphandhu, N. Hand-held navigation may improve accuracy in minimally invasive total knee arthroplasty: A prospective randomized controlled trial. Int. Orthop. 2016, 40, 51–57.
- Goh, G.S.H.; Liow, M.H.L.; Lim, W.S.R.; Tay, D.K.J.; Yeo, S.J.; Tan, M.H. Accelerometer-based navigation is as accurate as optical computer navigation in restoring the joint line and mechanical axis after total knee arthroplasty: A prospective matched study. J. Arthroplast. 2016, 31, 92–97.
- Iorio, R.; Mazza, D.; Drogo, P.; Bolle, G.; Conteduca, F.; Redler, A.; Ferretti, A. Clinical and radiographic outcomes of an accelerometer-based system for the tibial resection in total knee arthroplasty. Int. Orthop. 2015, 39, 461–466.
- Nam, D.; Nawabi, D.H.; Cross, M.B.; Heyse, T.J.; Mayman, D.J. Accelerometer-based computer navigation for performing the distal femoral resection in total knee arthroplasty. J. Arthroplast. 2012, 27, 1717–1722.
- Novoa-Parra, C.D.; Sanjuan-Cerveró, R.; Franco-Ferrando, N.; Larrainzar-Garijo, R.; Egea-Castro, G.; Lizaur-Utrilla, A. Complications of computer-assisted navigation in total knee replacement: Retrospective cohort of eight hundred and seventy eight consecutive knees. Int. Orthop. 2020, 44, 2621–2626.
- Blue, M.; Douthit, C.; Dennison, J.; Caroom, C.; Jenkins, M. Periprosthetic fracture through a unicortical tracking pin site after computer navigated total knee replacement. Case Rep. Orthop. 2018, 2018, 2381406.
- Kamara, E.; Berliner, Z.P.; Hepinstall, M.S.; Cooper, H.J. Pin site complications associated with computer-assisted navigation in hip and knee arthroplasty. J. Arthroplast. 2017, 32, 2842–2846.
- Brown, M.J.; Matthews, J.R.; Bayers-Thering, M.T.; Phillips, M.J.; Krackow, K.A. Low incidence of postoperative complications with navigated total knee arthroplasty. J. Arthroplast. 2017, 32, 2120–2126.
- Smith, T.J.; Siddiqi, A.; Forte, S.A.; Judice, A.; Sculco, P.K.; Vigdorchik, J.M.; Springer, B.D. Periprosthetic fractures through tracking pin sites following computer navigated and robotic total and unicompartmental knee arthroplasty: A systematic review. JBJ Rev. 2021, 9, e20.00091.
- Zhang, Y.Z.; Pei, G.X.; Lu, S.; Li, Z.J.; Zhao, J.M.; Wang, Y.W. Establishing lower-extremity mechanical axis by computer-aided design and its application in total knee arthroplasty. Chin. J. Orthop. 2013, 33, 1196–1203.
- Levengood, G.A.; Dupee, J. Accuracy of coronal plane mechanical alignment in a customized, individually made total knee replacement with patient-specific instrumentation. J. Knee Surg. 2018, 31, 792–796.
- Tian, S.C.; Yao, Q.Q.; Yin, X.D.; Liu, S.; Zhou, J.; Hu, J.; Wang, L.M. Effects of iASSIST navigation system and personal specific instrument assisted total knee arthroplasty in the treatment of osteoarthritis. Chin. J. Surg. 2017, 55, 423–429.
- Qiu, B.; Tang, B.S.; Deng, B.Y.; Liu, F.; Liu, F.; Zhen, D.; Zhu, W.M.; Zhang, M.J. Intelligentized surgery based on 3D printing technology for personalized total knee arthroplasty. Chin. J. Orthop. Trauma 2016, 18, 35–41.
- Pauzenberger, L.; Munz, M.; Brandl, G.; Frank, J.K.; Heuberer, P.R.; Laky, B.; Anderl, W. Patient-specific instrumentation improved three-dimensional accuracy in total knee arthroplasty: A comparative radiographic analysis of 1257 to tall knee arthroplasties. J. Orthop. Surg. Res. 2019, 14, 437.
- Netravali, N.A.; Shen, F.; Park, Y.; Bargar, W.L. A perspective on robotic assistance for knee arthroplasty. Adv. Orthop. 2013, 2013, 970703.
- Jacofsky, D.J.; Allen, M. Robotics in Arthoplasty: A Comprehensive Review. J. Arthroplast. 2016, 31, 2353–2363.
This entry is offline, you can click here to edit this entry!
