Three-dimensional (3D) printing technology has become increasingly used in the medical field, with reports demonstrating its superior advantages in both educational and clinical value when compared with standard image visualizations or current diagnostic approaches. Patient-specific or personalized 3D printed models serve as a valuable tool in cardiovascular disease because of the difficulty associated with comprehending cardiovascular anatomy and pathology on 2D flat screens. Additionally, the added value of using 3D-printed models is especially apparent in congenital heart disease (CHD), due to its wide spectrum of anomalies and its complexity.
1. Introduction
Three-dimensional (3D) printing technology is being increasingly used in the medical field, with studies documenting its application in a range of areas, from its original application in maxillofacial and orthopedic surgery to cardiovascular disease [
1,
2,
3,
4,
5,
6,
7,
8,
9,
10,
11,
12]. Of various cardiovascular abnormalities, congenital heart disease (CHD) represents a very challenging area due to the complexity of the congenital anomalies, the broad spectrum of conditions and the high variability between individuals. In the pediatric sub-specialization, a basic understanding of common CHD is necessary and plays an important role in clinical decision making and patient management. However, the standard visualization techniques, including cardiac CT, MRI and echocardiography, are limited in their ability to convert 2D images into a 3D object on a flat screen and so do not allow full comprehension of complex intracardiac anatomy and defects [
19,
36]. To overcome these limitations, 3D-printed physical models demonstrate superior advantages and strengths over the current image visualizations by providing realistic 3D representations of the spatial relationships between these cardiac structures and abnormal changes that are difficult to acquire on traditional 2D and 3D image reconstructions. In addition to its enhancement in understanding complex anatomy, 3D-printed heart models serve as a valuable tool to guide surgical planning, to train junior or inexperienced pediatric residents, and to educate healthcare professionals or parents of patients [
13,
14,
15,
16,
17,
18,
19,
20,
21,
22,
23,
24,
25,
26,
28,
29,
30,
31,
32,
33,
34,
35].
2. Generation of 3D-Printed Heart Models
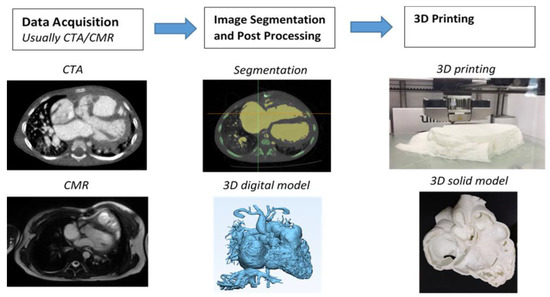
The steps from processing the original 2D digital imaging and communications in medicine (DICOM) images to 3D volume data, and from there to the segmentation of the image is well explained in the literature, and usually involves semi-automatic along with manual editing processes. Figure 1 shows a flow chart representing the creation of a 3D-printed heart model from an example of cardiac CT images.
Figure 1. Steps to generate 3D printed heart models. CTA-computed tomography angiography, CMR-cardiac magnetic resonance. Reprinted with permission under the open access from Sun et al. [
7].
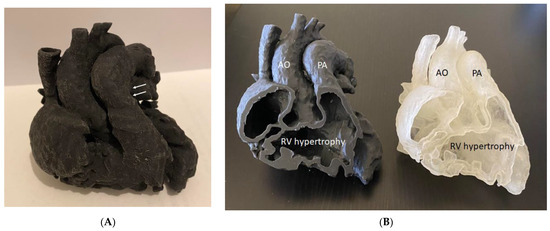
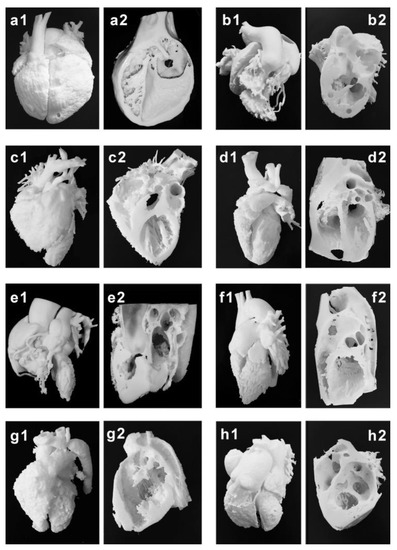
Mimics is the most commonly used commercial software tool in image post-processing of 3D datasets for 3D printing, while 3D Slicer is an open-source tool commonly used for segmentation of volumetric data for 3D printing. Usually, hollow heart models are generated to show both outside and inside views of cardiac anatomy and pathology as shown in
Figure 2, while blood pool models can also be printed to accurately demonstrate the spatial relationships between cardiac structures [
38] as shown in
Figure 3.
Figure 2. Three-dimensional-printed heart model of a case with Tetralogy of Fallot (ToF). (A): The model was printed in one piece. (B): The model was printed in two halves (with the same material, Agilus30, but different colors) showing the internal cardiac chambers and vascular abnormalities. Arrows indicate the pulmonary artery stenosis. AO—aorta (overriding aorta); PA—pulmonary artery; RV—right ventricle.
Figure 3. Three-dimensional printing of the blood pool and myocardium (showing inside views of cardiac structures at different angles) models for eight typical CHD cases (
a–
h). (
a1–
h1) are blood pool models, while (
a2–
h2) are myocardium models showing internal cardiac structures. Case 1: congenital corrected transposition of the great arteries. Case 2: double outlet right ventricle. Case 3: Williams syndrome. Case 4: coronary artery fistula. Case 5: Tetralogy of Fallot. Case 6: patent ductus arteriosus. Case 7: coarctation of the aorta. Case 8: ventricular septal defect. Reprinted with permission under the open access from Liang et al. [
38].
3. Accuracy of 3D-Printed Heart Models Derived from Imaging Modalities
Three-dimensional-printed models must accurately replicate anatomical details with high accuracy so that the models can be reliably used for different purposes. Current research has shown a very small difference between 3D-printed models and original source imaging data, whether they are acquired with CT, echocardiography, MRI or rotational angiography. It is noted that the mean difference in dimensional measurements between 3D-printed models and original images is less than 0.5 mm indicating the high accuracy of the 3D models, with excellent correlations between different observers and measurement approaches.
4. Three-Dimensional-Printing Materials for Printing Patient-Specific Models
While commonly used 3D printers including fused deposition modelling (FDM), stereolithography (SLA), polyjet and selective laser sintering (SLS) are the most well known printers in the literature. Printing materials play an important role in determining the final printed models that are most appropriate to serve the purpose of different applications. The models can be printed with rigid materials (such as polylactic acid, rigid resin and rigid photopolymer (VeroClear)) as shown in many early studies [
37], however, for printing heart or vascular models, soft and elastic materials with tissue properties similar to normal heart or vascular tissues are more important for the production of realistic heart models. Elastic materials include thermoplastic polyurethane (TPU), Tango materials such as TangoPlus, TangoGray, and Agilus A30 and Visiject CE-NT, and show great promise in printing CHD models. This is especially important when using 3D-printed models to simulate cardiac surgery or interventional cardiac procedures, as operators need to acquire similar tactile experience when performing simulation procedures on realistic 3D printed models [
37].
5. Educational and Clinical Value of 3D-Printed Heart Models in CHD
Three-dimensional-printed models are useful in medical and clinical education as the 3D-printed personalized models demonstrate superior advantages over current image visualization tools for the enhancement of students and medical graduates’ understanding of the complex 3D cardiac anatomy and pathology. Of the current applications of 3D printing in cardiovascular disease, 3D-printed CHD models represent the most common application in medical education according to the current literature [
37,
50,
51,
52,
53]. Studies have provided strong evidence in support of the use of 3D-printed models in CHD education, both for medical students, medical graduates (pediatric residents) and healthcare professionals.
3D-printed heart models significantly enhance medical students, pediatric residents, clinicians and pediatric cardiac nurses’ knowledge in learning normal cardiac anatomy and CHD [
25,
26,
28,
29,
30,
31,
33,
34,
35,
38,
54,
55]. Three-dimensional-printed CHD models were rated highly in terms of their accuracy and satisfaction scores by the study or experimental groups when compared with the control groups, and this is particularly obvious when assessing the complex CHD in comparison with simple CHD [
34]. In their recent report, Lau and Sun did not show significant improvements in knowledge retention among second and third year medical students when 3D-printed CHD models were compared with the current teaching methods using DICOM images and digital 3D heart models, although slightly higher scores were achieved in the 3D printing group [
25].
Another innovative tool in CHD education is the use of either virtual reality (VR), augmented reality (AR) or mixed reality (MR) as an alternative to 3D-printed models in education and pre-surgical planning of CHD. A user is immersed in a virtual environment during VR visualization, while AR is different from VR with virtual objects overlaying on the real world. MR extends the ability of VR and AR by allowing the user to interact with combined virtual and real objects (such as 3D-printed physical models) [
56,
57,
58,
59,
60].
6. 3D-Printed Models in CHD
6.1. Pre-Surgical Planning of CHD Surgery
The use of 3D-printed heart CHD models assisted pre-surgical planning, with up to 50% of surgical decisions changed by 3D-printed models according to a multi-center study [40]. Similarly, a number of studies reporting their single center experience with inclusion of either small or large number of cases also confirmed the usefulness of 3D-printed heart models in guiding surgical procedures in the management of pediatric CHD [21,23,63,64,65,66,67].
6.2. Hands-on Surgical Training for Congenital Heart Surgery Procedures and Medical Education
Congenital heart surgery is a technically challenging field of in pediatrics because of the wide variation of CHD, the rarity of each pathology and the smaller size of the patients. These technical challenges place strong demands for the development of appropriate training programs for surgical trainees to acquire technical skills comparable to experienced surgeons. Three-dimensional-printed heart models with high fidelity for replicating complex anatomy serve as a valuable simulation-based training program for surgical trainees to develop their technical skills prior to performing operations on patients. The hands-on surgical training (HOST) course enables participants to perform surgical procedures on 3D-printed models [
68,
69,
70,
84].
6.3. Improving Physician–Patient Communication/Facilitating Communication with Colleagues
Physician–patient communication plays an important role in the clinical setting with patients’ compliance and satisfaction with physicians having an impact on clinical outcomes [
91]. Visual aids are commonly used in clinical practice for physicians to explain information to patients regarding the disease condition and treatment options [
92]. However, conventional approaches of using 2D diagrams make it difficult for patients to imagine a 3D structure, and this is particularly challenging in CHD as patient and family tend to not possess adequate knowledge and understanding of complex heart anatomy or congenital defects. Three-dimensional-printed models have overcome this limitation by presenting a physically touchable model to the patient with improved understanding of both anatomy and pathology, thus enhancing communication between a physician and their patient and between a physician and their colleagues.
This entry is adapted from the peer-reviewed paper 10.3390/children10020319