Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
The term “vegan diet” comprises a range of eating patterns that prioritize nutrient-rich foods such as fruits and vegetables, legumes, whole grains, nuts, and seeds. In comparison to omnivorous diets, which are often lower in such products, the vegan diet has been favorably connected with changes in cardiovascular disease (CVD) risk markers such as reduced body mass index (BMI) values, total serum cholesterol, serum glucose, inflammation, and blood pressure.
- vegan diet
- plant-based
- health benefits
- nutrients
- cardiovascular health
- CVD
- risk factors
1. Inflammatory Response as a Result of Unhealthy Dietary Patterns
Chronic Inflammation of the Vessel Walls Due to Unhealthy Diet
The standard diet that has become widely embraced in many countries over the past 40 years is rather unhealthy, containing relatively high amounts of alcohol [1] and processed foods [2], especially those with additives [3], and only a few fruits and vegetables and other meals rich in fiber and prebiotics [4][5]. An unhealthy diet can alter the structure and function of the gut microbiota and has been linked to increased gut permeability [6][7][8] and epigenetic modifications in the immune system [6], which can lead to low-grade endotoxemia and systemic chronic inflammation (SCI) of the vessel walls [6][7][8]. Similarly, foods with a high glycemic index, such as pure sugars and refined grains, which play an important role in most ultra-processed foods, can lead to increased oxidative stress and thus activate inflammatory genes [9].
Within this framework, uncontrolled alcohol consumption that triggers various reactions in the body causes chronic inflammation to increase over time rather than resolve. In the gut, for example, excess alcohol can lead to the proliferation of bacterial waste products, particularly endotoxins, substances that cause inflammation by activating proteins and immune cells. With more endotoxin production, the inflammation worsens instead of improving [7].
Trans fats, which raise low-density lipoprotein (LDL) and reduce high-density lipoprotein (HDL), and dietary salt (NaCl) are two other components of an unhealthy diet known to be pro-inflammatory. As stated by a recent cohort study of 44,551 French people, a 10 percent increase in the proportion of highly processed food consumption was associated with a 14 percent higher risk of all-cause mortality, consistent with the predicted adverse health outcomes of eating foods high in trans fats and sodium [10].
In this context, according to another observational study of 80,082 women in the Nurses’ Health Study cohort, it was revealed that higher consumption of trans fats, or to a lesser extent saturated fats, is correlated with an increased risk of coronary heart disease (CHD), while higher consumption of polyunsaturated (non-hydrogenated) and monounsaturated fats is associated with a reduced risk [11]. The relationship to CHD risk can only partially be explained by the unfavorable effect of trans fats on the lipid profile.
At the same time, in a cross-sectional study of 730 women from the same patient cohort, markers of endothelial activation such as CRP (C-reactive protein), E-selectin, soluble intercellular adhesion molecule (ICAM-1), and soluble vascular cell adhesion molecule (VCAM-1) were higher, suggesting that increased trans fatty acid intake may promote inflammation and adversely affect endothelial function. CRP levels were 73% higher in women in the highest quintile of trans fat intake than in the lowest quintile [12].
Endothelial dysfunction contributes significantly to the pathogenesis of atherosclerotic cardiovascular disease (ASCVD), which is a chronic inflammatory disease of the arterial wall mediated mostly by phagocytic (eating) leukocytes (white blood cells) such as monocytes and macrophages. This initiates a complicated pathogenic cascade that starts with the accumulation of circulating LDL in the subendothelial layer of the arteries [13][14][15][16]. Following an endothelial injury, LDL becomes mildly oxidized [17]. Further oxidation of LDL leads to fully oxidized LDL (ox-LDL), which is then avidly taken up by macrophages via scavenger receptors (SR) and ultimately transformed into foam cells (the hallmark of early fatty streak lesions) [18].
The expression and detachment of adhesion glycoproteins on the endothelium regulates leukocyte attachment to endothelial cells. The leukocyte binding to endothelial tissue is mediated by the aforementioned types of adhesion molecules (ICAM-1), (VCAM-1), as well as selectins (e.g., P-selectin and E-selectin) [19]. The pathophysiology of endothelial damage and atherosclerosis due to higher LDL levels resulting from an unhealthy diet is illustrated in Figure 1.
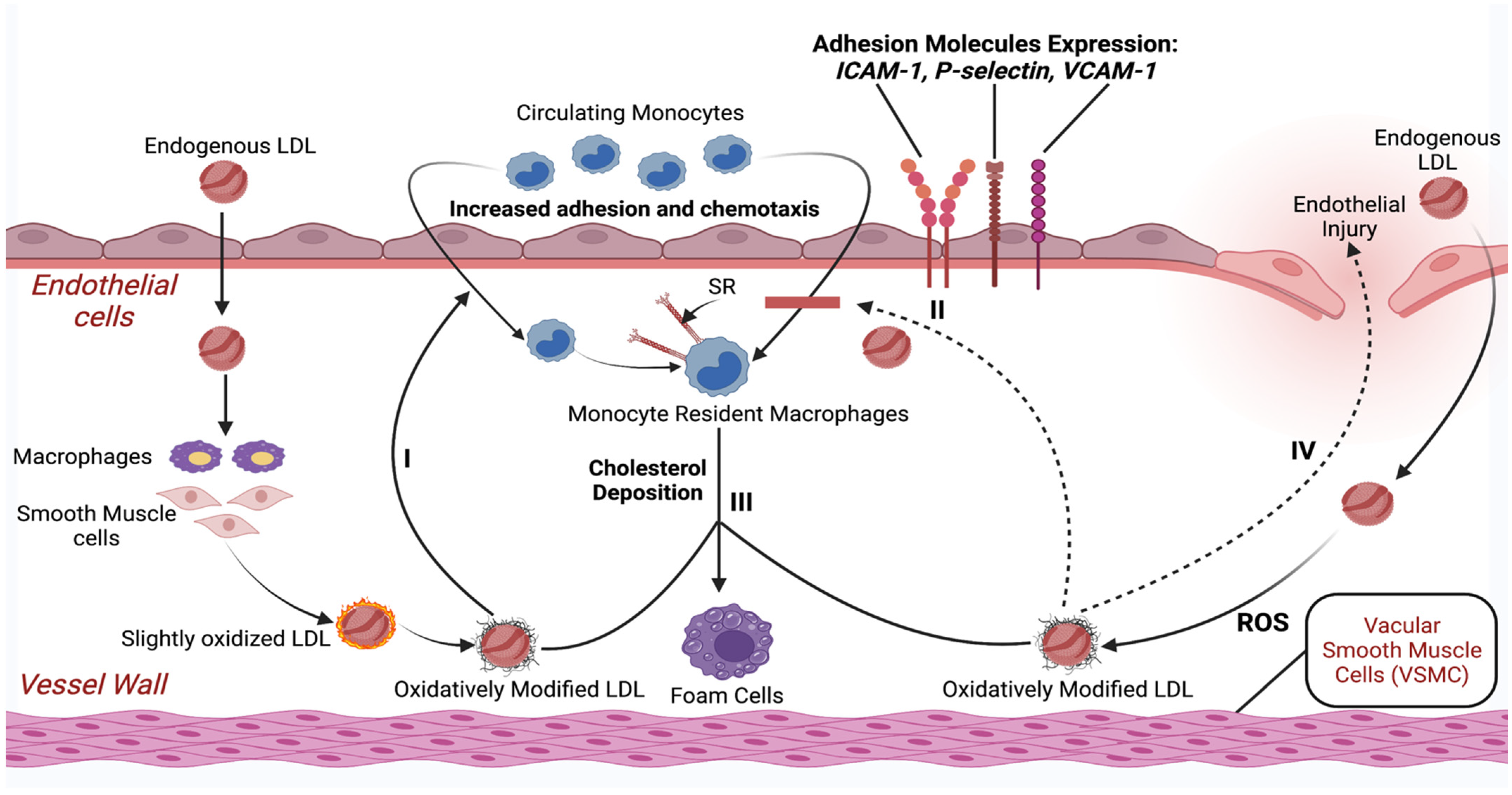
Figure 1. Schematic illustration of endothelial damage and initiation of the atherosclerotic process with only higher LDL levels as a risk factor. Abbreviations: LDL—low-density lipoprotein; ROS—reactive oxygen species; SR—scavenger receptor; ICAM-1—intercellular adhesion molecule-1; VCAM-1—vascular cell adhesion protein-1. Created with BioRender.com (accessed on 17 April 2021).
Overall, dietary patterns that are high in sugar, alcohol, saturated and trans fatty acids, and refined starches and low in natural antioxidants and fiber from fruits, vegetables, and whole grains may activate the innate immune system, most likely through an increase in pro-inflammatory cytokines and a decrease in anti-inflammatory cytokines. This imbalance may stimulate the formation of a pro-inflammatory state, which causes endothelial dysfunction at the vascular level, resulting in a predisposition to atherosclerotic plaque formation. This can lead susceptible people to an increased prevalence of CHD.
It is vital to understand that both an unhealthy diet and a vegan diet can initiate chronic inflammation if a vegan diet contains inadequate amounts of essential vitamins and nutrients as well as omega-3 fatty acids [20].
2. Benefits/Risks of a Vegan Diet for the Cardiovascular System
CVD is the leading cause of mortality, currently accounting for one-third of all deaths worldwide and growing in prevalence. Examples of CVDs include CHD, peripheral artery disease, cerebrovascular disease, rheumatic and congenital heart disease, and venous thromboembolism. In this context, vegan diets are considered to improve health and decrease the risk of CVD. On the other hand, according to some studies, a vegan diet may be related to reduced intake of protein, vitamins, or minerals, and thus should also be evaluated in terms of harmful effects. The research on veganism is contradictory and inadequately evaluated [21]. The vast majority of studies on health effects of vegan and plant-based diets were short term and cannot give accurate data on cardiovascular outcomes, which has mostly been estimated based on the changes in biomarker concentrations. More studies with hard endpoints such as major adverse cardiovascular events are required to fully understand the effects of vegan and vegetarian diet on the cardiovascular system. The potential positive and negative impacts of a vegan diet on the CV system discussed in the following paragraphs are shown in Figure 2.
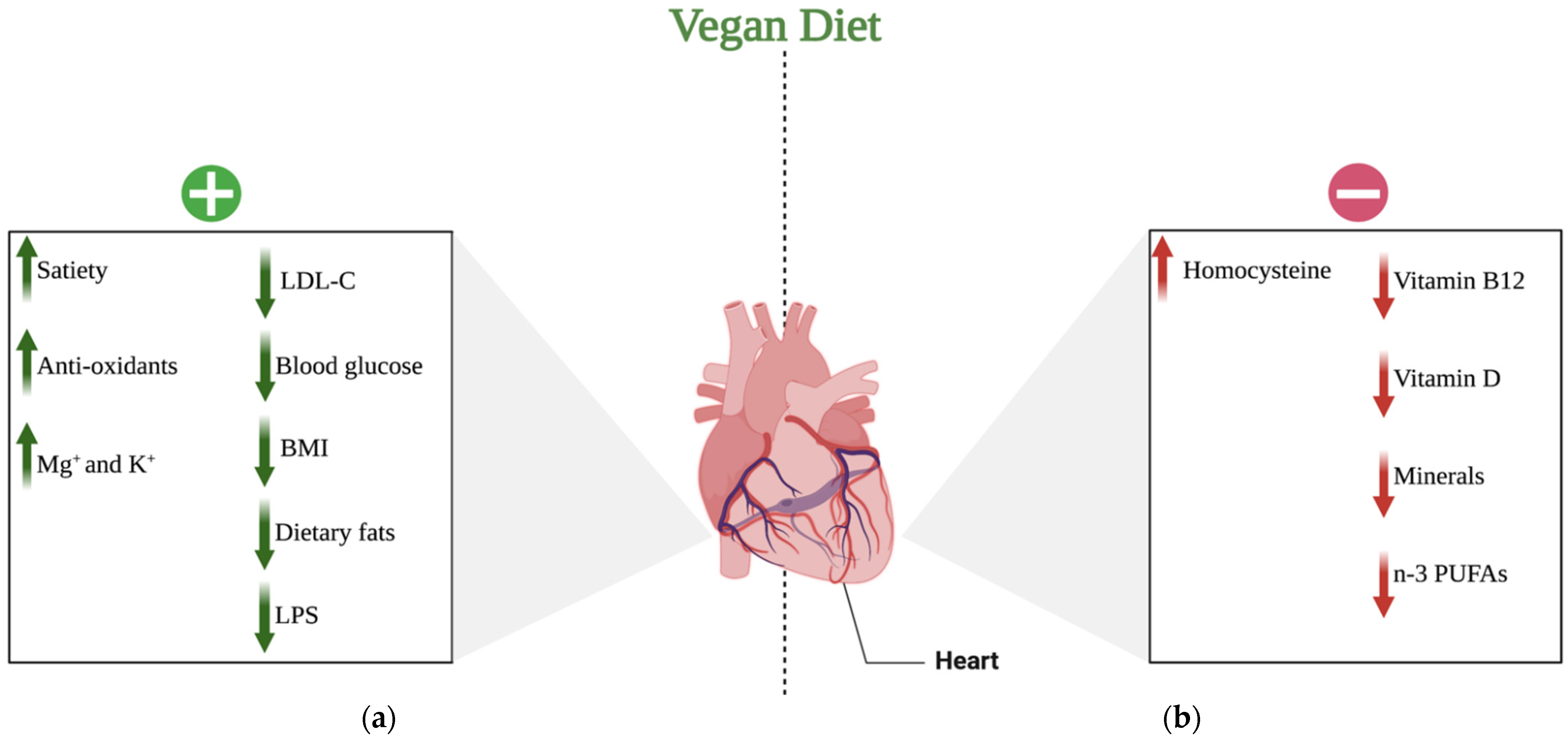
Figure 2. Potential effects of a vegan diet on the cardiovascular system: (a) positive effects of a vegan diet on the cardiovascular system; (b) negative effects of a vegan diet on the cardiovascular system. Abbreviations: (+) positive; (−) negative; ↑ increase; ↓ decrease; LDL-C—low-density lipoprotein-cholesterol; BMI—body mass index; LPS—lipopolysaccharide; K+—potassium cations; Mg+—magnesium cations; n-3 PUFAs—n-3 polyunsaturated fatty acids. Created with BioRender.com (accessed on 17 April 2021).
2.1. The Positive Effects of Veganism on the Cardiovascular System
PBDs, especially vegan diets, have been shown to provide several health benefits [22]. Numerous studies have demonstrated that the benefits of a vegan diet on human health are due to increased daily consumption of fresh fruits, vegetables, cereal grains, nuts, legumes, and seeds, indicating that vegans make healthier lifestyle choices than those who follow other dietary patterns [23]. Some of the potential health merits include a decreased rate of certain conditions, such as CVD. Vegan diets have been reported to be low-risk therapies for decreasing BMI, systolic and diastolic blood pressure (SBP and DBP), and LDL levels, minimizing the incidence of coronary heart disease events by 40% [24].
Additionally, the results of a systematic review and meta-analysis of cohort studies, which were eventually drawn from the analyses of only two studies, indicated that greater adherence to the PBDs was significantly associated with a lower risk of all-cause mortality (10%) (HR: 0.90, 95% CI: 0.82, 0.99; I2 = 90.7%, pheterogeneity < 0.001), and CHD mortality (23%). Based on the same study, it was also found that among vegan diets, compliance with a usual vegetarian diet might protect against CVD and CHD mortality [25].
Because of its low saturated fatty acid (SFAs) and high fiber content, the vegan diet is characterized by low energy intake. Dietary fibers are a diverse group of plant molecules (carbohydrate polymers with ten or more monomer units) with varying physical and chemical characteristics [26]. Water-soluble (SFs) and insoluble fibers (IFs) are the two most common types. Because these fibers are not hydrolyzed by digestive enzymes, they are not completely digested in the human gut [27]. They alter intestinal function by regulating intestinal motions, increasing fecal bulk, and avoiding constipation, among other things. SF, for instance, dissolves in water and forms thick solutions (gels) in the intestinal lumen, delaying or partially reducing carbohydrate, lipid, and cholesterol absorption. These viscous gels can also delay emptying of the stomach and prolong food absorption, enhancing satiety and altering insulin and glycemic post-prandial responses [28].
Moreover, we know that meals of vegetable origin are high in polyphenols, which are natural bioactive chemicals generated by plants as secondary metabolites [29]. Polyphenols may also benefit CV health by inhibiting platelet aggregation, reducing inflammation of the vessel walls, modulating apoptotic processes, lowering LDL oxidation, and improving the lipid profile [30]. Several in vitro investigations have revealed that polyphenols have a high antioxidant capacity due to their ability to neutralize reactive oxygen species (ROS). Their antioxidant properties, presumably paired with their ability to modify nitric oxide (NO) synthesis, allow them to protect endothelial function [31].
Other antioxidant minerals found in a vegan diet include vitamin C, vitamin E, beta-carotene, potassium, and magnesium. Potassium has been proven to decrease blood pressure and the risk of stroke due to its favorable effects on endothelial function and vascular homeostasis [32]. Furthermore, magnesium has been linked to better cardiometabolic outcomes due to its effect on glucose metabolism as well as its anti-inflammatory, vasodilatory, and antiarrhythmic characteristics [33].
The influence on cholesterol metabolism is another important way that a vegan diet might benefit CV health. The low SFA concentration and high unsaturated fat content can enhance the lipid profile. SFAs have been found to activate the pro-inflammatory toll-like receptor-4 (TLR4) signaling pathway, resulting in the production of cytokines capable of triggering a chronic inflammatory state [34][35]. SFAs can also interact with the gut microbiota by facilitating the transfer of lipopolysaccharide (LPS), which is a powerful endotoxin, a mediator of systemic inflammation, and a driver of septic shock [36].
Various studies, however, have revealed that polyunsaturated fatty acids (PUFAs) activate several anti-inflammatory pathways. As a result, a diet high in unsaturated fats and low in SFAs can lower the risk of CVDs through its potential anti-inflammatory effects [37][38].
A meta-analysis of observational studies that compared the vegan diets to omnivorous diets observed that the vegan diet has less energy and saturated fat as a result it protects against cardiometabolic conditions. The authors discovered a decrease in fasting blood glucose and BMI and an improvement in the lipid profile [39].
2.2. The Negative Effect of Veganism on the Cardiovascular System
In contrast, lower intake of n-3 long-chain polyunsaturated fatty acids (i.e., DHA and EPA), vitamins (i.e., vitamin B12 and D), specific nutrients, including selenium, zinc, iodine, and calcium, as well as higher levels of essential amino acids (i.e., homocysteine), may explain some of the unfavorable CV effects associated with vegan diets, such as the potential increased risk of ischemic stroke [40]. One study has found that vegans and vegetarians had a higher risk of ischemic stroke than people who ate animal products (HR, 1.54; 95 percent CI, 0.95–2.48) [21].
Nevertheless, systematic reviews and meta-analyses that compared vegetarians and vegans to nonvegetarians have shown no clear association with stroke or subtypes of stroke for vegans and vegetarians [41][42]. At the same time and as specified by a meta-analysis, with a large-scale study design of 657,433 participants, the incidence of total stroke was lower among vegetarians in studies conducted in Asia than nonvegetarians (HR = 0.66; 95% CI = 0.45–0.95; I2 = 54%, n = 3). Furthermore, the same review found that although there is no strong association between vegetarian diets and a reduced risk of stroke in young adults, there is evidence that older participants aged 50–65 years following a vegetarian pattern exhibited a lower incidence of stroke than nonvegetarians [42].
Although a plant-based diet and especially a vegan diet is believed to be healthy, it can nonetheless result in a higher level of essential amino acids. The most important molecule in this study is homocysteine (Hcy), which has been identified as a risk factor for atherosclerotic vascular disease and hypercoagulability. Given that, there is evidence of a link between hyperhomocysteinemia arising from a vegan diet and CVD, such as heart attacks and strokes [43].
In this regard, and as previously stated, while plant foods provide various nutrients, including dietary fiber and phytochemicals, they do not contain enough vitamin B12 to meet the needs of their consumers, leading to severe deficiency. Deficiency in vitamin B12 will eventually result in hyperhomocysteinemia [44]. Subsequently, because it lowers vascular flexibility and alters homeostasis, elevated homocysteine will induce vascular endothelial impairment. It may also aggravate the negative consequences of risk factors such as hypertension, smoking, cholesterol, and lipoprotein metabolism [45]. Most critically, Hcy has been recognized as a significant CVD risk factor [46].
Besides causing hyperhomocysteinemia, a vitamin B12 deficiency caused by avoiding animal-based meals can also contribute to an increased risk of cardiac conditions via its function in macrocytosis [47]. To be more specific, a deficiency in vitamin B12 can increase the risk of macrocytic anemia, a condition arising from the abnormal growth of red blood cells. In this way, it leads to various diseases, such as heart failure (HF), coronary artery disease, and stroke. It can additionally decrease oxygen delivery and the carrying capacity of blood vessels, undermining circulation’s primary role.
Similarly, vitamin D deficiency, which can be caused by veganism, increases the risk of CVD and is linked to other well-known risk factors for heart diseases such as high blood pressure, obesity, and diabetes [48][49][50]. In particular, low levels of the vitamin may initially predispose the body to congestive heart failure and chronic blood vessel inflammation (associated with hardening of the arteries). It might also change hormone levels, increasing insulin resistance and thus raising the risk of diabetes [51].
To date, certain cross-sectional studies have connected vitamin D deficiency to an increased risk of CVD, such as hypertension, heart failure, and ischemic heart disease [52]. Simultaneously, other prospective studies have found that vitamin D deficiency increases the risk of incident hypertension or sudden cardiac death in individuals who already have CVD [51].
Not only vitamin deficiencies, but other dietary components found in vegan diets can promote an inflammatory response and hence contribute to the development of chronic inflammation [53][54]. These include micronutrient deficiencies, such as zinc and selenium, caused by eating processed or refined foods low in vitamins and minerals, as well as insufficient omega-3 levels, notably EPA and DHA, which impact the resolution phase of inflammation. Eventually, inflammation will induce an atherogenic response, resulting in serious health problems, including arrhythmias, heart failure, and CHD [55].
This entry is adapted from the peer-reviewed paper 10.3390/jcdd10030094
References
- Grant, B.F.; Chou, S.P.; Saha, T.D.; Pickering, R.P.; Kerridge, B.T.; Ruan, W.J.; Huang, B.; Jung, J.; Zhang, H.; Fan, A.; et al. Prevalence of 12-Month Alcohol Use, High-Risk Drinking, and DSM-IV Alcohol Use Disorder in the United States, 2001-2002 to 2012–2013. JAMA Psychiatry 2017, 74, 911.
- Martínez Steele, E.; Baraldi, L.G.; Louzada, M.L.d.C.; Moubarac, J.-C.; Mozaffarian, D.; Monteiro, C.A. Ultra-Processed Foods and Added Sugars in the US Diet: Evidence from a Nationally Representative Cross-Sectional Study. BMJ Open 2016, 6, e009892.
- Chassaing, B.; van de Wiele, T.; de Bodt, J.; Marzorati, M.; Gewirtz, A.T. Dietary Emulsifiers Directly Alter Human Microbiota Composition and Gene Expression Ex Vivo Potentiating Intestinal Inflammation. Gut 2017, 66, 1414–1427.
- Carrera-Bastos, P.; O’Keefe, F.; Lindeberg, S.; Cordain, L. The Western Diet and Lifestyle and Diseases of Civilization. Res. Rep. Clin. Cardiol. 2011, 2, 2–15.
- Bentley, J.U.S. Trends in Food Availability and a Dietary Assessment of Loss-Adjusted Food Availability, 1970–2014. Econ. Inf. Bull. 2017, 166, 2–30.
- Richards, J.L.; Yap, Y.A.; McLeod, K.H.; Mackay, C.R.; Mariño, E. Dietary Metabolites and the Gut Microbiota: An Alternative Approach to Control Inflammatory and Autoimmune Diseases. Clin. Transl. Immunol. 2016, 5, e82.
- Bishehsari, F.; Magno, E.; Swanson, G.; Desai, V.; Voigt, R.M.; Forsyth, C.B.; Keshavarzian, A. Alcohol and Gut-Derived Inflammation. Alcohol Res. 2017, 38, 163–171.
- Lerner, A.; Matthias, T. Changes in Intestinal Tight Junction Permeability Associated with Industrial Food Additives Explain the Rising Incidence of Autoimmune Disease. Autoimmun. Rev. 2015, 14, 479–489.
- Dickinson, S.; Hancock, D.P.; Petocz, P.; Ceriello, A.; Brand-Miller, J. High-Glycemic Index Carbohydrate Increases Nuclear Factor-B Activation in Mononuclear Cells of Young, Lean Healthy Subjects. Am. J. Clin. Nutr. 2008, 87, 1188–1193.
- Schnabel, L.; Kesse-Guyot, E.; Allès, B.; Touvier, M.; Srour, B.; Hercberg, S.; Buscail, C.; Julia, C. Association Between Ultraprocessed Food Consumption and Risk of Mortality Among Middle-Aged Adults in France. JAMA Intern. Med. 2019, 179, 490.
- Rank, F.; Eir, M.; Tampfer, J.S.; Nn, J.O.A.; Anson, E.M.; Imm, R.R.; Olditz, R.A.C.; Osner, E.A.R.; Harles, C.; Ennekens, H.H.; et al. Dietary Fat Intake and the Risk of Coronary Heart Disease in Women. N. Engl. J. Med. 1997, 337, 1491–1499.
- Lopez-Garcia, E.; Schulze, M.B.; Meigs, J.B.; Manson, J.E.; Rifai, N.; Stampfer, M.J.; Willett, W.C.; Hu, F.B. Nutritional Epidemiology Consumption of Trans Fatty Acids Is Related to Plasma Biomarkers of Inflammation and Endothelial Dysfunction. J. Nutr. 2005, 135, 562–566.
- Simionescu, N.; Vasile, E.; Lupu, F.; Popescu, G. Prelesional Events in Atherogenesis. Accumulation of Extracellular Cholesterol-Rich Liposomes in the Arterial Intima and Cardiac Valves of the Hyperlipidemic Rabbit. Am. J. Pathol. 1986, 123, 109–125.
- Schwartz, C.J.; Valente, A.J.; Sprague, E.A.; Kelley, J.L.; Nerem, R.M. The Pathogenesis of Atherosclerosis: An Overview. Clin. Cardiol. 1991, 14, 1–16.
- Ross, R. Atherosclerosis: A Problem of the Biology of Arterial Wall Cells and Their Interactions with Blood Components. Arteriosclerosis 1981, 1, 293–311.
- Virmani, R.; Kolodgie, F.D.; Burke, A.P.; Farb, A.; Schwartz, S.M. Lessons from Sudden Coronary Death. Arter. Thromb Vasc. Biol. 2000, 20, 1262–1275.
- Shi, W.; Haberland, M.E.; Jien, M.L.; Shih, D.M.; Lusis, A.J. Endothelial Responses to Oxidized Lipoproteins Determine Genetic Susceptibility to Atherosclerosis in Mice. Circulation 2000, 102, 75–81.
- Golia, E.; Limongelli, G.; Natale, F.; Fimiani, F.; Maddaloni, V.; Pariggiano, I.; Bianchi, R.; Crisci, M.; D’Acierno, L.; Giordano, R.; et al. Inflammation and Cardiovascular Disease: From Pathogenesis to Therapeutic Target. Curr. Atheroscler. Rep. 2014, 16, 435.
- Panés, J.; Perry, M.; Granger, D.N. Leukocyte-Endothelial Cell Adhesion: Avenues for Therapeutic Intervention. Br. J. Pharmacol. 1999, 126, 537.
- van Winckel, M.; vande Velde, S.; de Bruyne, R.; van Biervliet, S. Clinical Practice: Vegetarian Infant and Child Nutrition. Eur. J. Pediatr. 2011, 170, 1489–1494.
- Kaiser, J.; van Daalen, K.R.; Thayyil, A.; Cocco, M.T.d.A.R.R.; Caputo, D.; Oliver-Williams, C. A Systematic Review of the Association Between Vegan Diets and Risk of Cardiovascular Disease. J. Nutr. 2021, 151, 1539–1552.
- Fontana, L.; Meyer, T.E.; Klein, S.; Holloszy, J.O. Long-Term Low-Calorie Low-Protein Vegan Diet and Endurance Exercise Are Associated with Low Cardiometabolic Risk. Rejuvenation Res. 2007, 10, 225–234.
- Aune, D.; Giovannucci, E.; Boffetta, P.; Fadnes, L.T.; Keum, N.N.; Norat, T.; Greenwood, D.C.; Riboli, E.; Vatten, L.J.; Tonstad, S. Fruit and Vegetable Intake and the Risk of Cardiovascular Disease, Total Cancer and All-Cause Mortality—A Systematic Review and Dose-Response Meta-Analysis of Prospective Studies. Int. J. Epidemiol. 2017, 46, 1029.
- Sacks, F.M.; Lichtenstein, A.H.; Wu, J.H.Y.; Appel, L.J.; Creager, M.A.; Kris-Etherton, P.M.; Miller, M.; Rimm, E.B.; Rudel, L.L.; Robinson, J.G.; et al. Dietary Fats and Cardiovascular Disease: A Presidential Advisory From the American Heart Association. Circulation 2017, 136, e1–e23.
- Jafari, S.; Hezaveh, E.; Jalilpiran, Y.; Jayedi, A.; Wong, A.; Safaiyan, A.; Barzegar, A. Plant-based diets and risk of disease mortality: A systematic review and meta-analysis of cohort studies. Crit. Rev. Food Sci. Nutr. 2021, 62, 7760–7772.
- Holscher, H.D. Dietary Fiber and Prebiotics and the Gastrointestinal Microbiota. Gut Microbes 2017, 8, 172.
- Dhingra, D.; Michael, M.; Rajput, H.; Patil, R.T. Dietary Fibre in Foods: A Review. J. Food Sci. Technol. 2012, 49, 255.
- Hervik, A.K.; Svihus, B. The Role of Fiber in Energy Balance. J. Nutr. Metab. 2019, 2019, 4983657.
- Pandey, K.B.; Rizvi, S.I. Plant Polyphenols as Dietary Antioxidants in Human Health and Disease. Oxid. Med. Cell Longev. 2009, 2, 270.
- Habauzit, V.; Morand, C. Evidence for a Protective Effect of Polyphenols-Containing Foods on Cardiovascular Health: An Update for Clinicians. Ther. Adv. Chronic. Dis. 2012, 3, 87.
- Tangney, C.C.; Rasmussen, H.E. Polyphenols, Inflammation, and Cardiovascular Disease. Curr. Atheroscler. Rep. 2013, 15, 324.
- Key, T.J.; Appleby, P.N.; Rosell, M.S. Health Effects of Vegetarian and Vegan Diets. Proc. Nutr. Soc. 2006, 65, 35–41.
- Pickering, R.; Bradlee, M.; Singer, M.; Moore, L. Higher Intakes of Potassium and Magnesium, but Not Lower Sodium, Reduce Cardiovascular Risk in the Framingham Offspring Study. Nutrients 2021, 13, 269.
- O’Neill, L.A.J. Targeting Signal Transduction as a Strategy to Treat Inflammatory Diseases. Nat. Rev. Drug. Discov. 2006, 5, 549–564.
- Hwang, D.H.; Kim, J.A.; Lee, J.Y. Mechanisms for the Activation of Toll-like Receptor 2/4 by Saturated Fatty Acids and Inhibition by Docosahexaenoic Acid. Eur. J. Pharmacol. 2016, 785, 24.
- Fritsche, K.L. The Science of Fatty Acids and Inflammation. Adv. Nutr. 2015, 6, 293S–301S.
- Willett, W.C. The Role of Dietary N-6 Fatty Acids in the Prevention of Cardiovascular Disease. J. Cardiovasc. Med. 2007, 8, S42–S45.
- Petersson, H.; Basu, S.; Cederholm, T.; Risérus, U. Serum Fatty Acid Composition and Indices of Stearoyl-CoA Desaturase Activity Are Associated with Systemic Inflammation: Longitudinal Analyses in Middle-Aged Men. Br. J. Nutr. 2008, 99, 1186–1189.
- Benatar, J.R.; Stewart, R.A.H. Cardiometabolic risk factors in vegans; A meta-analysis of observational studies. PLoS ONE 2018, 13, e0209086.
- Jabri, A.; Kumar, A.; Verghese, E.; Alameh, A.; Kumar, A.; Khan, M.S.; Khan, S.U.; Michos, E.D.; Kapadia, S.R.; Reed, G.W.; et al. Meta-Analysis of Effect of Vegetarian Diet on Ischemic Heart Disease and All-Cause Mortality. Am. J. Prev. Cardiol. 2021, 7, 100182.
- Dybvik, J.S.; Svendsen, M.; Aune, D. Vegetarian and vegan diets and the risk of cardiovascular disease, ischemic heart disease and stroke: A systematic review and meta-analysis of prospective cohort studies. Eur. J. Nutr. 2022, 62, 51–69.
- Lu, J.-W.; Yu, L.-H.; Tu, Y.-K.; Cheng, H.-Y.; Chen, L.-Y.; Loh, C.-H.; Chen, T.-L. Risk of Incident Stroke among Vegetarians Compared to Nonvegetarians: A Systematic Review and Meta-Analysis of Prospective Cohort Studies. Nutrients 2021, 13, 3019.
- Shenoy, V.; Mehendale, V.; Prabhu, K.; Shetty, R.; Rao, P. Correlation of Serum Homocysteine Levels with the Severity of Coronary Artery Disease. Indian J. Clin. Biochem. 2014, 29, 339.
- Ankar, A.; Bhimji, S.S. Vitamin B12 Deficiency; StatPearls: Treasure Island, FL, USA, 2022.
- Baszczuk, A.; Kopczyński, Z. Hyperhomocysteinemia in Patients with Cardiovascular Disease. Postepy Hig. Med. Dosw. 2014, 68, 579–589.
- Cybulska, B.; Kłosiewicz-Latoszek, L. Homocysteine—Is It Still an Important Risk Factor for Cardiovascular Disease? Kardiol. Pol. 2015, 73, 1092–1096.
- Pawlak, R. Is Vitamin B12 Deficiency a Risk Factor for Cardiovascular Disease in Vegetarians? Am. J. Prev. Med. 2015, 48, e11–e26.
- Chan, J.; Jaceldo-Siegl, K.; Fraser, G.E. Serum 25-Hydroxyvitamin D Status of Vegetarians, Partial Vegetarians, and Nonvegetarians: The Adventist Health Study-2. Am. J. Clin. Nutr. 2009, 89, 1686S–1692S.
- Kendrick, J.; Targher, G.; Smits, G.; Chonchol, M. 25-Hydroxyvitamin D Deficiency Is Independently Associated with Cardiovascular Disease in the Third National Health and Nutrition Examination Survey. Atherosclerosis 2009, 205, 255–260.
- Martini, L.A.; Wood, R.J. Vitamin D Status and the Metabolic Syndrome. Nutr. Rev. 2022, 64, 479.
- Kheiri, B.; Abdalla, A.; Osman, M.; Ahmed, S.; Hassan, M.; Bachuwa, G. Vitamin D Deficiency and Risk of Cardiovascular Diseases: A Narrative Review. Clin. Hypertens. 2018, 24, 9.
- Brøndum-Jacobsen, P.; Benn, M.; Jensen, G.B.; Nordestgaard, B.G. 25-Hydroxyvitamin D Levels and Risk of Ischemic Heart Disease, Myocardial Infarction, and Early Death: Population-Based Study and Meta-Analyses of 18 and 17 Studies. Arterioscler Thromb. Vasc. Biol. 2012, 32, 2794–2802.
- Craig, W.J. Health Effects of Vegan Diets. Am. J. Clin. Nutr. 2009, 89, 1627S–1633S.
- Menzel, J.; Jabakhanji, A.; Biemann, R.; Mai, K.; Abraham, K.; Weikert, C. Systematic review and meta-analysis of the associations of vegan and vegetarian diets with inflammatory biomarkers. Sci. Rep. 2020, 10, 1–11.
- de Jesus, N.M.; Wang, L.; Herren, A.W.; Wang, J.; Shenasa, F.; Bers, D.M.; Lindsey, M.L.; Ripplinger, C.M. Atherosclerosis Exacerbates Arrhythmia Following Myocardial Infarction: Role of Myocardial Inflammation. Heart Rhythm. Off. J. Heart Rhythm. Soc. 2015, 12, 169.
This entry is offline, you can click here to edit this entry!
