Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Due to increasing health and environmental issues, indoor air quality (IAQ) has garnered much research attention with regard to incorporating advanced clean air technologies. Various physicochemical air treatments have been used to monitor, control, and manage air contaminants, such as monitoring devices (gas sensors and internet of things-based systems), filtration (mechanical and electrical), adsorption, UV disinfection, UV photocatalysts, a non-thermal plasma approach, air conditioning systems, and green technologies (green plants and algae).
- indoor air quality
- pollutants
- filtration
- UV disinfection
1. Introduction
The indoor environmental conditions of buildings and houses greatly affect human health [1]. According to the World Health Organization (WHO), indoor air pollution may affect ~4–5 million people per year [2]. Most urban humans spend ~90% of their time indoors [3]. Therefore, the effect of indoor air environments on human health is obvious. Common sources of indoor air pollution include cooking, heating, smoking, garages, cleaning, electronic machines, outdoor air, and other human activities. Harmful indoor air pollutants include oxides of carbon, nitrogen, and sulfur; volatiles; particulates; aerosols; biological pollutants; and many more [4] (Figure 1). Indoor air pollution can lead to a range of physical illnesses, including cardiac, respiratory, nervous system, and even cancer-related diseases [5][6][7]. Consequently, indoor air quality (IAQ) monitoring, control, and management are considered important for preventing the related potential health risks [8]. The measurement of indoor pollutant concentration has been considered to be a crucial strategy for controlling and enhancing IAQ. It is also vital to determine the sources of indoor air pollution to ensure total eradication. The relationships between indoor pollutants and health risks and health effects have been found to be significant enough to justify adopting suitable remediation strategies.
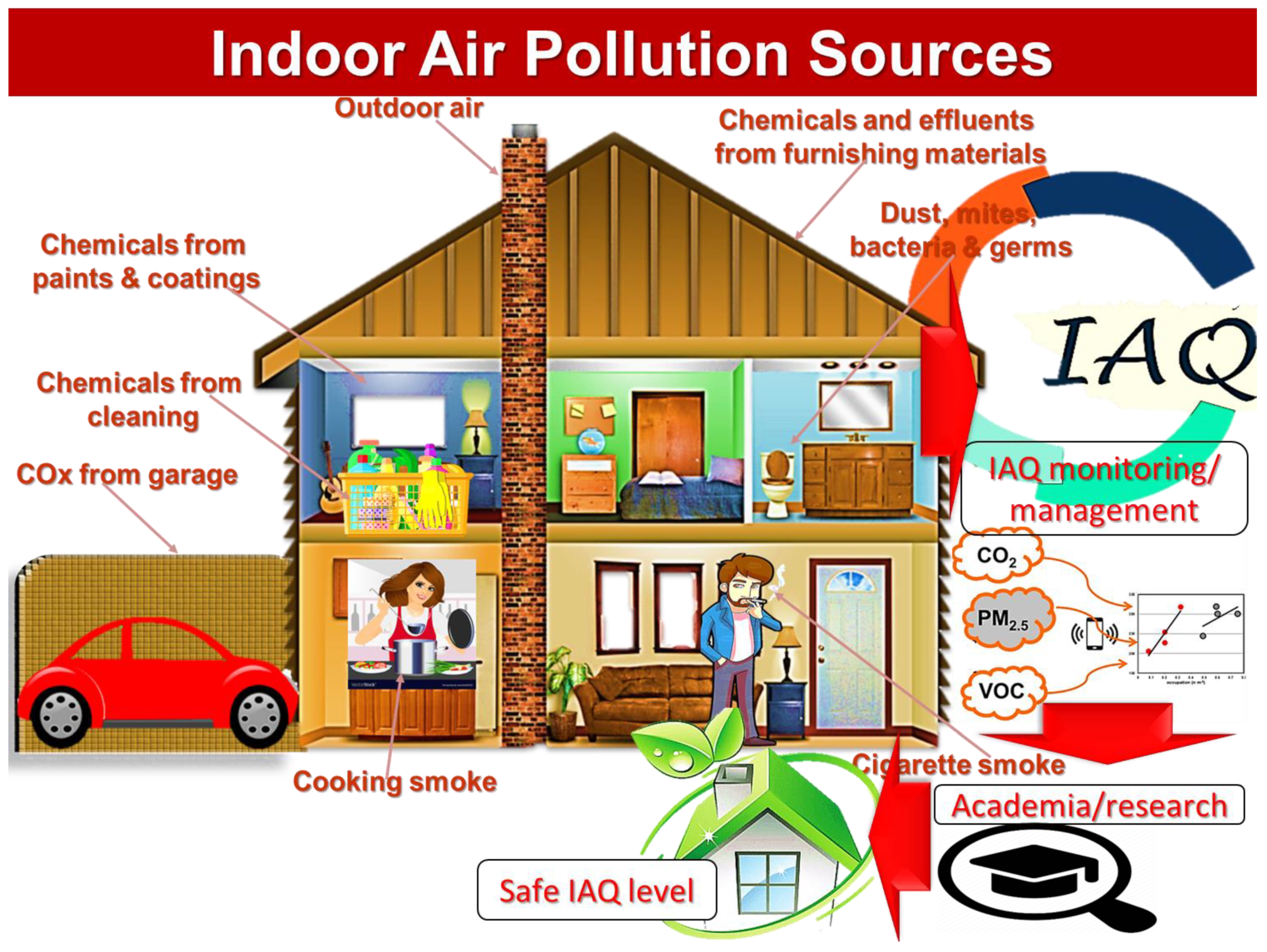
Figure 1. Common pollutants and sources in indoor air.
2. Indoor Air Pollution: A Serious Threat to Human Health
2.1. Indoor Pollutants
IAQ is generally affected by factors such as outdoor air quality, building/construction materials, and human activity inside buildings [9]. Outdoor air pollutants directly influence IAQ due to the possible transfer of toxins from the outdoors to indoor atmosphere [10]. Outdoor pollutants result from industrial and transport activities [11]. Construction/building materials have been a source of indoor pollution due to the evolution of toxic organic compounds from paints, adhesives, coatings, poly(vinyl chloride) floor covers, rubber carpets, etc. [12]. Moreover, daily human activities (cooking, smoking, heating, cleaning, solvent uses, etc.) produce lots of indoor pollutants such as noxious gases, particulate matter, allergens, bacteria, viruses, insects, mites, etc. [13][14][15]. Major pollution-causing noxious gases include oxides of carbon (COx) such as carbon monoxide (CO) and carbon dioxide (CO2); oxides of sulfur (SOx) such as sulfur dioxide (SO2); oxides of nitrogen (NOx) as nitric oxide (NO), nitrogen dioxide (NO2), particulate matter (PM), and volatile organic matter (PM) [16]. All indoor human activities and building materials are a rich source of PM, VOC, NOx, COx, SOx, ozone, Radon, etc. The ozone (O3) is also a toxic indoor pollutant from computers, photocopying machines, printers, etc.
PM has varying size of <10 µm (large diameter coarse particles), fine particles of diameter <2.5 µm, and ultrafine particles of diameter <0.1 µm [17]. Inhalation of PM causes damaging effects to the lungs, heart, respiratory, and cardiovascular systems.
VOC consist of toxic gases and volatile chemicals from liquids or solids [18]. Formaldehyde is a toxic form of VOC emitted from building materials such as plywood, paints, coatings, coverings, etc. VOC are also penetrated in indoor environment from the outdoor air. The long term exposure to VOC can cause serious health risks like cancer [19].
NOx such as NO and NO2 result from cooking, combustion, and other heating, and fire sources [20]. NO is a primary pollutant which is oxidized to form NO2. NO2 can easily react with water to produce nitrous acid (HONO)which is a harmful indoor contaminant. Common health risks of NOx are asthmatic reactions and lung infections [21].
SOx, especially SO2 is a harmful indoor pollutant originating from outdoor air, cooking, smoking, heaters, and coal/wood burning [22]. Human exposure to SOx harms respiratory and cardiac functions causing asthmatic, pulmonary, and cardiovascular diseases.
COx such as CO emerges from indoor combustion (tobacco, cooking, gas heaters, stoves, furnaces, chimneys, etc.) and comes from outdoor air [23]. Even at low concentrations, CO can harm the cardiovascular, respiratory, and nervous systems [24].
Ozone is generally produced in the indoor environment due to photochemical reactions of VOC, COx, NOx, etc. [25]. It arises from outdoor sources, indoor photocopying, the and use of machines. O3 can seriously affect lungs, DNA, and human organs causing asthmatic and respiratory diseases.
Radon is an indoor pollutant from building materials, soil, and tap water [26]. In indoor buildings, concentrations of radioactive radon (222Rn) gas can attain harmful levels [27]. Lethal dose LD50 for radon inhalation is ~1.0 g causing toxic effects such as lung cancer and respiratory diseases [28].
Pesticides are used in an indoor environment to prevent pests, bacteria, fungi, insects, etc. Pesticides cause irritating effects on eyes, nose, and throat. Moreover, these chemicals cause damaging effects to the central nervous system, kidneys, and cancer risks [29].
Aerosols originated in indoor environments from various outdoor sources and also result from indoor gas-to-particle conversion of VOC [30]. Aerosols can be of different types such as carbonaceous aerosols, biological aerosols, and gas-to-particle aerosols. Carbonaceous aerosols originate from combustion, while biological aerosols are formed from animals, bacteria, and microorganisms. Aerosols frequently affect the human heart and brain-related systems.
Indoor biological pollutants include biological allergens (pets’ saliva, dust, cockroaches, mites, pollens, etc.) and microorganisms (bacteria, viruses, fungi, etc.) [31]. Biological pollutants emerge from outdoor air. The most common human health effects include respiratory and allergic diseases.
To control and monitor all the above-mentioned pollutants, precise techniques need to be developed. To some extent, IAQ depends on indoor ventilation rates and related systems.
2.2. Health Effects–Short and Long Term
Indoor air pollutants may cause short-term or long-term health effects. Short-term exposure involves interaction with low concentrations of indoor pollutants or contact with indoor pollutants for a short span of time. Short-term exposure to indoor pollutants such as particulate matter, volatile organic compounds, NOx, COx, etc., does not cause serious health effects [32]. In some cases, short-term exposure to indoor pollutants may initiate headaches. Especially, NOx level of 28.97 μg/m3, PM2.5 concentration of 21.51 μg/m3, PM10 level of 37.79-μg/m3, and COx concentration of 1.15-ppm were found to cause headaches in indoor inhabitants [33]. On the other hand, long-term exposure to indoor air pollutants has their serious health effects. Usually, exposure to indoor pollutants for more than one month results in serious health risks [34]. Consequently, daily exposure or long term exposure may lead to cancer-causing effects [35]. Other important effects include sick building syndrome [36][37], building-related illness [38][39], pulmonary diseases [40][41], cardiovascular diseases [42][43][44], and many more. Table 1 illustrates common indoor pollutants and resulting hazardous effects on human health.
Table 1. Common indoor pollutants and their effects on human health.
| Pollutant | Source | Health Influence | Ref |
|---|---|---|---|
| Particulate matter |
|
|
[45][46][47] |
| VOCs |
|
|
[48][49] |
| NO2 |
|
|
[50][51] |
| O3 |
|
|
[52][53] |
| SO2 |
|
|
[54][55] |
| COx |
|
|
[56][57][58] |
| Aerosol |
|
|
[59][60] |
| Radon |
|
|
[61] |
| Pesticides |
|
|
[62][63] |
| Biological allergens |
|
|
[64] |
| Microorganism |
|
|
[65][66] |
According to literature reports, high indoor particulate matter PM1, PM2.5, and PM10 concentration of up to 2000–9000 μg/m3 (mainly due to indoor cooking and heating activities) cause pulmonary infections, lungs diseases, and cancer risks [67][68]. Moreover, PM and CO2 emissions due to tobacco smoke instigated coughing, sneezing, and eye irritation in indoor inhabitants [69]. Presence of indoor gaseous pollutants such as CO, NO2, SO2, O3 was found to be associated with asthma risks and nervous system issues [70]. High indoor dust ingestion of ~8.79–34.39 ng/g, containing polychlorinated biphenyl concentrations, had serious health effects such as cancer risks and loss of indoor working productivity [71]. Indoor inhalation of flame retardants (up to concentrations of 128,000 ng.g−1) revealed respiratory issues and loss of indoor working productivity [72]. Furthermore, high levels of indoor microflora and bacteria ~10,000–15,000 cfu m−3 caused respiratory and cancer risks [73][74].
3. Monitoring of Indoor Air Quality (IAQ)
Indoor air quality (IAQ) is defined as air value inside and around the buildings [75]. IAQ is important for health and coziness of building inhabitants. Harmful air pollutants (volatile organic compounds, particulate matter, and physical, chemicals, and biological aspects) at high concentration levels in indoor air cause negative health effects on human body.
An analysis of air quality level of south-east Asian countries (Pakistan, India, Nepal, Sri Lanka, Bangladesh, and Bhutan) has been carried out [76]. Comparative evaluation was performed for indoor pollutants such as PM10, PM2.5 and CO. WHO standards were considered for comparison. The WHO standards set for indoor PM10 level were 50 μg/m3 and PM2.5 was 25 μg/m3. Air quality level (200–5000 μg/m3) was attained much higher than the WHO standard value for safe IAQ [77]. Moreover, carbon monoxide level was found much higher (~29.4 ppm) than the WHO set standards (<5 ppm). The suggested reason was conventional indoor fuel burning sources, which affected >50% of indoor population. Consequently, employment of IAQ policies was found indispensable to safeguard public health in these countries [78]. Moreover, rising indoor pollutant levels pointed to increasing respiratory, nervous, and mortality rates in population [79].
Research, analysis, and monitoring for IAQ levels have arisen as a significant research field [80]. Purpose of supervising IAQ is to protect humans occupying non-industrial buildings from harmful pollutants. It is important to mention that IAQ assessments are found to be affected by indoor conditions such as temperature, light, humidity, air flow, etc. [81]. Initially, indoor pollutants have been controlled through adjusting indoor temperature and humidity. Figure 2 demonstrates a flow chart for steps involved in monitoring, control, and management of indoor air quality.
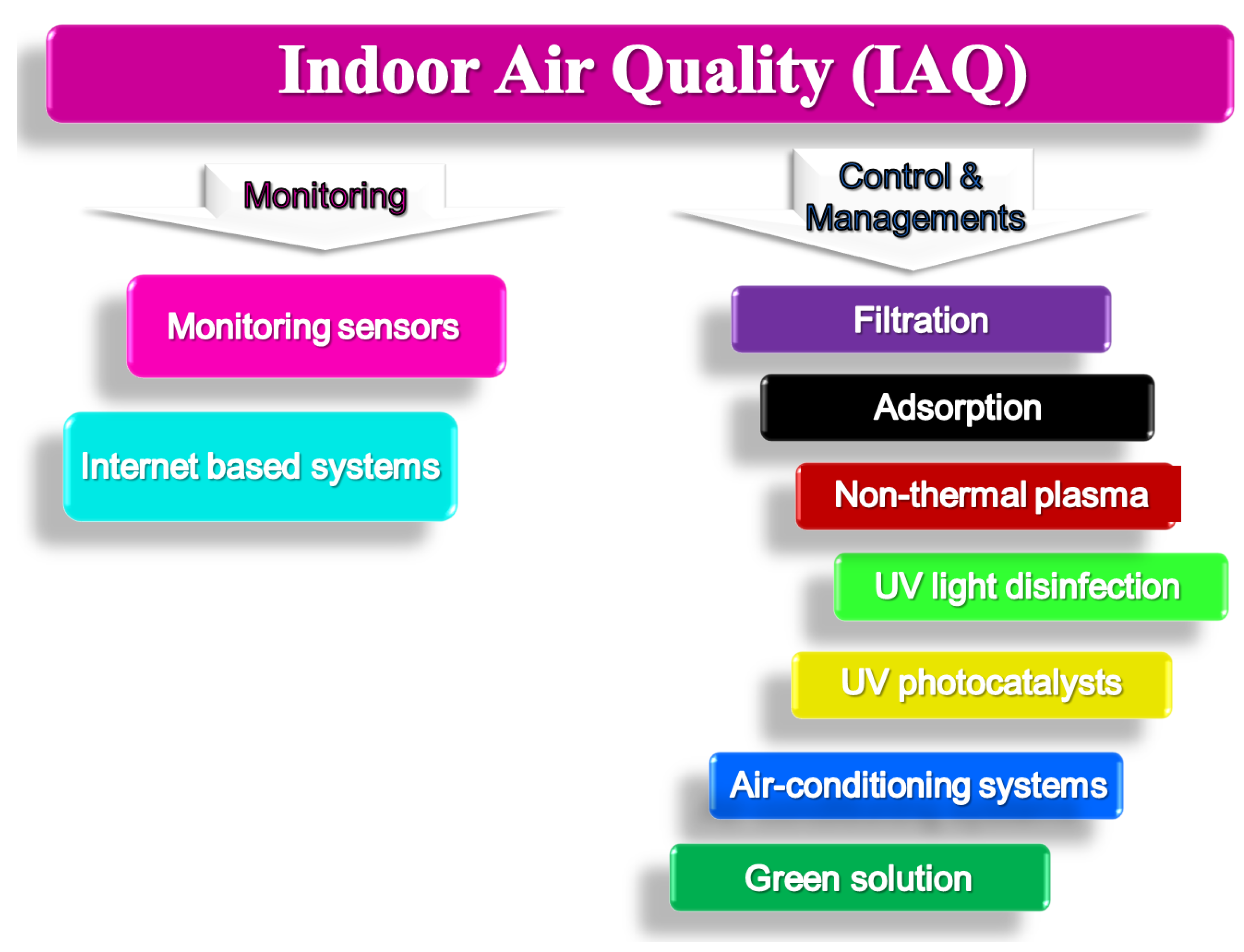
Figure 2. Indoor air quality—Monitoring, control, and management.
3.1. Materials Based IAQ Sensors
For IAQ monitoring systems, sensors have gained considerable research interest [82]. Initially, two-dimensional nanostructured materials have been invented for gas sensing [83]. Later research attempts focused zero-, one-, and three-dimensional nanostructured materials for developing IAQ monitoring sensors. These nanomaterials have been used to develop gas sensors, light sensors, humidity sensors, and temperature sensors. For IAQ monitoring systems, manifold phases of data acquisition, processing, storage, and analysis have been used [84]. Figure 3 shows a conceptual architecture of IAQ monitoring system. The data processing phase is accomplished at hardware as well as software level. The data acquired is sent for storage and processing. The software was used for enhancing data analysis and visualization. Accuracy of sensors has been achieved through calibrations and maintenance procedures. Consequently, development of novel low-cost sensors offers precise output data for advanced IAQ monitoring systems.
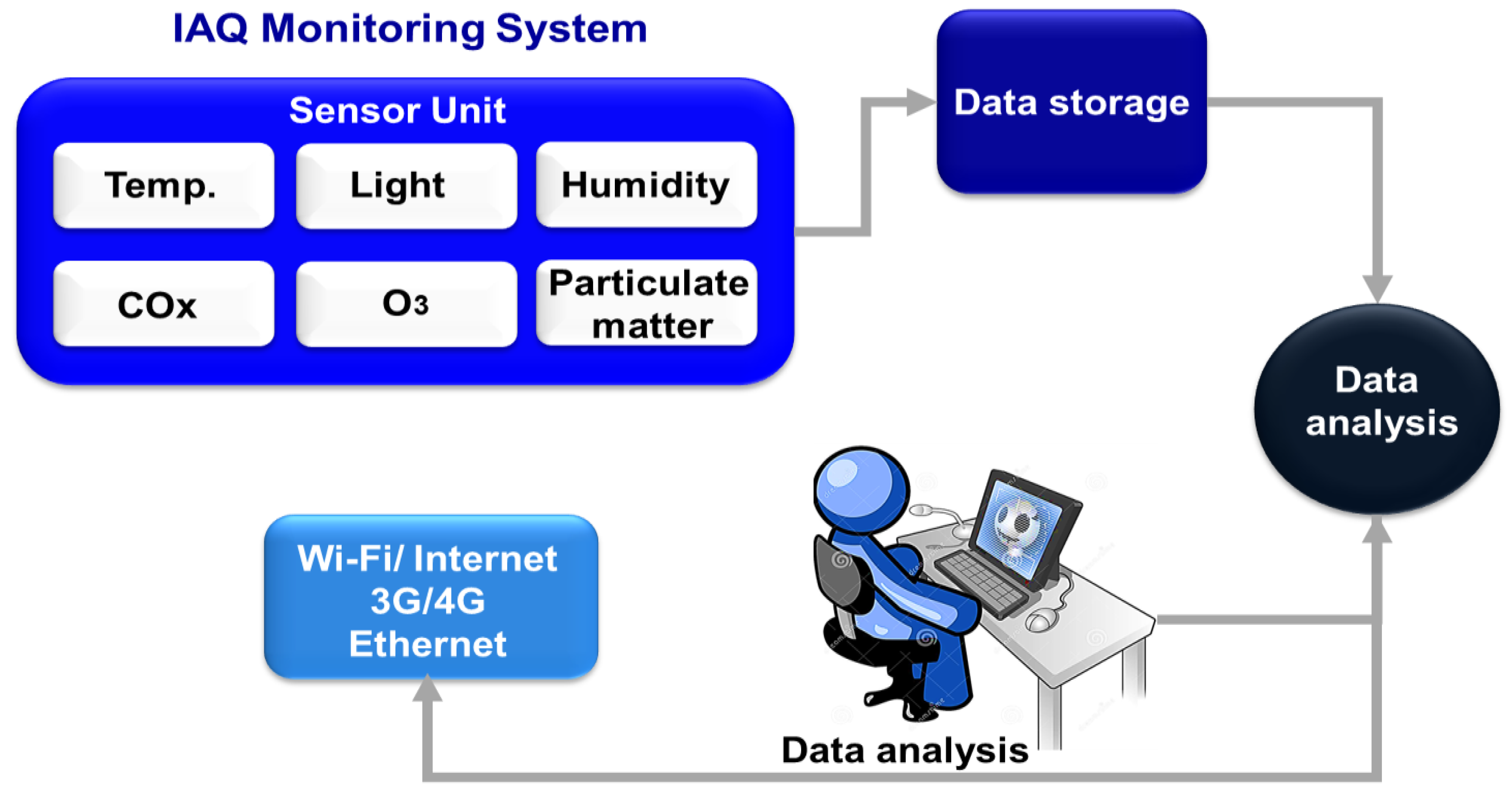
Figure 3. General conceptual architecture of IAQ monitoring system.
3.2. Advanced Technologies for IAQ Monitoring IAQ—Internet of Things (IoT)-Based Systems
Advanced techniques have been developed for IAQ monitoring [85]. Most prominently, internet of things (IoT)-based systems and wireless sensor networks have been developed. The IoT has been used as most popular technique for industrial revolution for IAQ monitoring [86]. Portable IoT devices have been effectively used for IAQ monitoring and control [87]. Recently, electronic noses or e-noses have been used as IoT devices for IAQ monitoring [88]. An e-nose is made up of multi-sensors arrays, processing units, digital software, and artificial neural networks. The e-nose has ability to monitor, detect, and discriminate various gaseous molecules [89]. Moreover, e-noses have low-cost and compactness for developing efficient IAQ monitoring systems [90]. The e-noses can sense numerous air pollutants such as CO, CO2, NO2, and particulate matter [91].
This entry is adapted from the peer-reviewed paper 10.3390/pollutants3010011
References
- Pluschke, P.; Schleibinger, H. Indoor Air Pollution; Springer: Berlin/Heidelberg, Germany, 2018.
- Amegah, A.K.; Jaakkola, J.J. Household air pollution and the sustainable development goals. Bull. World Health Organ. 2016, 94, 215.
- Mendoza, D.L.; Benney, T.M.; Bares, R.; Fasoli, B.; Anderson, C.; Gonzales, S.A.; Crosman, E.T.; Hoch, S. Investigation of Indoor and Outdoor Fine Particulate Matter Concentrations in Schools in Salt Lake City, Utah. Pollutants 2022, 2, 82–97.
- Kraft, M.; Rauchfuss, K.; Fromme, H.; Grün, L.; Sievering, S.; Köllner, B.; Chovolou, Y. Inhalation exposure to PCB from contaminated indoor air—How much is absorbed into the blood? Pollutants 2021, 1, 181–193.
- Keswani, A.; Akselrod, H.; Anenberg, S.C. Health and clinical impacts of air pollution and linkages with climate change. NEJM Evid. 2022, 1, EVIDra2200068.
- Zeng, Y.; Laguerre, A.; Gall, E.T.; Heidarinejad, M.; Stephens, B. Experimental Evaluations of the Impact of an Additive Oxidizing Electronic Air Cleaner on Particles and Gases. Pollutants 2022, 2, 98–134.
- Bain-Reguis, N.; Smith, A.; Martin, C.H.; Currie, J. Indoor CO2 and Thermal Conditions in Twenty Scottish Primary School Classrooms with Different Ventilation Systems during the COVID-19 Pandemic. Pollutants 2022, 2, 180–204.
- Ciccioli, P.; Pallozzi, E.; Guerriero, E.; Iannelli, M.A.; Donati, E.; Lilla, L.; Rinaldi, C.; Svaldi, P.; Ciccioli, P.; Mabilia, R. A New Testing Facility to Investigate the Removal Processes of Indoor Air Contaminants with Different Cleaning Technologies and to Better Assess and Exploit Their Performances. Environments 2021, 9, 3.
- Marć, M.; Śmiełowska, M.; Namieśnik, J.; Zabiegała, B. Indoor air quality of everyday use spaces dedicated to specific purposes—A review. Environmental Science and Pollut. Res. 2018, 25, 2065–2082.
- Peng, Z.; Deng, W.; Tenorio, R. Investigation of indoor air quality and the identification of influential factors at primary schools in the North of China. Sustainability 2017, 9, 1180.
- Liang, J. Chemical Modeling for Air Resources: Fundamentals, Applications, and Corroborative Analysis; Elsevier: Amsterdam, The Netherlands, 2013.
- Gopalakrishnan, P.; Kavinraj, M.; Vivekanadhan; Jeevitha, N. Effect of indoor air quality on human health-A review. In Proceedings of the AIP Conference, Antalya, Turkey, 12–15 May 2021; AIP Publishing LLC: New York, NY, USA, 2021.
- Wang, M.; Li, L.; Hou, C.; Guo, X.; Fu, H. Building and health: Mapping the knowledge development of sick building syndrome. Buildings 2022, 12, 287.
- Li, C.; Zhu, Q.; Jin, X.; Cohen, R.C. Elucidating Contributions of Anthropogenic Volatile Organic Compounds and Particulate Matter to Ozone Trends over China. Environ. Sci. Technol. 2022, 56, 12906–12916.
- Zhang, G.; Xu, H.; Qi, B.; Du, R.; Gui, K.; Wang, H.; Jiang, W.; Liang, L.; Xu, W. Characterization of atmospheric trace gases and particulate matter in Hangzhou, China. Atmos. Chem. Phys. 2018, 18, 1705–1728.
- Mata, T.M.; Felgueiras, F.; Martins, A.A.; Monteiro, H.; Ferraz, M.P.; Oliveira, G.M.; Gabriel, M.F.; Silva, G.V. Indoor air quality in elderly centers: Pollutants emission and health effects. Environments 2022, 9, 86.
- Zhai, Y.; Li, X.; Wang, T.; Wang, B.; Li, C.; Zeng, G. A review on airborne microorganisms in particulate matters: Composition, characteristics and influence factors. Environ. Int. 2018, 113, 74–90.
- Ubando, A.T.; Africa, A.D.M.; Maniquiz-Redillas, M.C.; Culaba, A.B.; Chen, W.-H. Reduction of particulate matter and volatile organic compounds in biorefineries: A state-of-the-art review. J. Hazard. Mater. 2021, 403, 123955.
- Cheng, L.; Wei, W.; Guo, A.; Zhang, C.; Sha, K.; Wang, R.; Wang, K.; Cheng, S. Health risk assessment of hazardous VOCs and its associations with exposure duration and protection measures for coking industry workers. J. Clean. Prod. 2022, 379, 134919.
- Andersen, C.; Omelekhina, Y.; Rasmussen, B.B.; Nygaard Bennekov, M.; Skov, S.N.; Køcks, M.; Wang, K.; Strandberg, B.; Mattsson, F.; Bilde, M. Emissions of soot, PAHs, ultrafine particles, NOx, and other health relevant compounds from stressed burning of candles in indoor air. Indoor Air 2021, 31, 2033–2048.
- Paciência, I.; Cavaleiro Rufo, J.; Moreira, A. Environmental inequality: Air pollution and asthma in children. Pediatr. Allergy Immunol. 2022, 33, 1–21.
- Kureshi, R.R.; Thakker, D.; Mishra, B.K.; Ahmed, B. Use Case of Building an Indoor Air Quality Monitoring System. In Proceedings of the 2021 IEEE 7th World Forum on Internet of Things (WF-IoT), New Orleans, LA, USA, 14–31 July 2021.
- Nair, A.N.; Anand, P.; George, A.; Mondal, N. A review of strategies and their effectiveness in reducing indoor airborne transmission and improving indoor air quality. Environ. Res. 2022, 213, 113579.
- Sakai, H.; Yasuda, S.; Okuda, C.; Yamada, T.; Owaki, K.; Miwa, Y. Examination of central nervous system by functional observation battery after massive intravenous infusion of carbon monoxide-bound and oxygen-bound hemoglobin vesicles in rats. Curr. Res. Pharmacol. Drug Discov. 2022, 3, 100135.
- Zhu, Y.; Wei, Z.; Yang, X.; Tao, S.; Zhang, Y.; Shangguan, W. Comprehensive control of PM 2.5 capture and ozone emission in two-stage electrostatic precipitators. Sci. Total Environ. 2022, 858, 159900.
- Sá, J.P.; Branco, P.T.; Alvim-Ferraz, M.C.; Martins, F.G.; Sousa, S.I. Radon in Indoor Air: Towards Continuous Monitoring. Sustainability 2022, 14, 1529.
- Stanley, F. An Analysis of Human Exposure to Alpha Particle Radiation; University of Calgary: Calgary, Canada, 2018.
- Patocka, J. Human health and environmental uranium. Mil. Med. Sci. Lett. 2014, 83, 120–131.
- Figueiredo, D.M.; Duyzer, J.; Huss, A.; Krop, E.J.; Gerritsen-Ebben, M.; Gooijer, Y.; Vermeulen, R.C. Spatio-temporal variation of outdoor and indoor pesticide air concentrations in homes near agricultural fields. Atmos. Environ. 2021, 262, 118612.
- Mostafa, M.Y.A.; Khalaf, H.N.B.; Zhukovsky, M. Attachment rate characteristics of different wide used aerosol sources in indoor air. J. Environ. Health Sci. Eng. 2021, 19, 867–879.
- López, A.; Yusà, V.; Villoldo, E.; Corpas-Burgos, F.; Coscollà, C. Indoor air pesticide in dwellings of breastfeeding mothers of the Valencian Region (Spain): Levels, exposure and risk assessment. Atmos. Environ. 2021, 248, 118231.
- Błaszczyk, E.; Rogula-Kozłowska, W.; Klejnowski, K.; Kubiesa, P.; Fulara, I.; Mielżyńska-Švach, D. Indoor air quality in urban and rural kindergartens: Short-term studies in Silesia, Poland. Air Qual. Atmos. Health 2017, 10, 1207–1220.
- Dales, R.E.; Cakmak, S.; Vidal, C.B. Air pollution and hospitalization for headache in Chile. Am. J. Epidemiol. 2009, 170, 1057–1066.
- Sun, S.; Zheng, X.; Villalba-Díez, J.; Ordieres-Meré, J. Indoor air-quality data-monitoring system: Long-term monitoring benefits. Sensors 2019, 19, 4157.
- Maroni, M.; Seifert, B.; Lindvall, T. Indoor Air Quality: A Comprehensive Reference Book; Elsevier: Amsterdam, The Netherlands, 1995.
- Sarkhosh, M.; Najafpoor, A.A.; Alidadi, H.; Shamsara, J.; Amiri, H.; Andrea, T.; Kariminejad, F. Indoor Air Quality associations with sick building syndrome: An application of decision tree technology. Build. Environ. 2021, 188, 107446.
- Hou, J.; Sun, Y.; Dai, X.; Liu, J.; Shen, X.; Tan, H.; Yin, H.; Huang, K.; Gao, Y.; Lai, D. Associations of indoor carbon dioxide concentrations, air temperature, and humidity with perceived air quality and sick building syndrome symptoms in Chinese homes. Indoor Air 2021, 31, 1018–1028.
- Fan, L.; Ding, Y. Research on risk scorecard of sick building syndrome based on machine learning. Build. Environ. 2022, 211, 108710.
- Kalender-Smajlović, S.; Kukec, A.; Dovjak, M. The problem of indoor environmental quality at a general Slovenian hospital and its contribution to sick building syndrome. Build. Environ. 2022, 214, 108908.
- Hansel, N.N.; Putcha, N.; Woo, H.; Peng, R.; Diette, G.B.; Fawzy, A.; Wise, R.A.; Romero, K.; Davis, M.F.; Rule, A.M. Randomized clinical trial of air cleaners to improve indoor air quality and chronic obstructive pulmonary disease health: Results of the CLEAN AIR study. Am. J. Respir. Crit. Care Med. 2022, 205, 421–430.
- Kamal, R.; Srivastava, A.K.; Kesavachandran, C.N.; Bihari, V.; Singh, A. Chronic obstructive pulmonary disease (COPD) in women due to indoor biomass burning: A meta analysis. Int. J. Environ. Health Res. 2022, 32, 1403–1417.
- Mannucci, P.M. An ecological alliance against air pollution and cardiovascular disease. Bleeding Thromb. Vasc. Biol. 2022, 1, 21.
- Münzel, T.; Sørensen, M.; Daiber, A. Transportation noise pollution and cardiovascular disease. Nat. Rev. Cardiol. 2021, 18, 619–636.
- Zheng, C.; Tang, H.; Wang, X.; Chen, Z.; Zhang, L.; Kang, Y.; Yang, Y.; Chen, L.; Zhou, H.; Cai, J. Left ventricular diastolic dysfunction and cardiovascular disease in different ambient air pollution conditions: A prospective cohort study. Sci. Total Environ. 2022, 831, 154872.
- Miller, M.R.; Shaw, C.A.; Langrish, J.P. From particles to patients: Oxidative stress and the cardiovascular effects of air pollution. Future Cardiol. 2012, 8, 577–602.
- Brook, R.D.; Rajagopalan, S.; Pope, C.A., III; Brook, J.R.; Bhatnagar, A.; Diez-Roux, A.V.; Holguin, F.; Hong, Y.; Luepker, R.V.; Mittleman, M.A. Particulate matter air pollution and cardiovascular disease: An update to the scientific statement from the American Heart Association. Circulation 2010, 121, 2331–2378.
- Al-Kindi, S.G.; Brook, R.D.; Biswal, S.; Rajagopalan, S. Environmental determinants of cardiovascular disease: Lessons learned from air pollution. Nat. Rev. Cardiol. 2020, 17, 656–672.
- Tran, V.V.; Park, D.; Lee, Y.-C. Indoor air pollution, related human diseases, and recent trends in the control and improvement of indoor air quality. Int. J. Environ. Res. Public Health 2020, 17, 2927.
- Weschler, C.J.; Nazaroff, W.W. Dermal uptake of organic vapors commonly found in indoor air. Environ. Sci. Technol. 2014, 48, 1230–1237.
- Bernstein, J.A.; Alexis, N.; Bacchus, H.; Bernstein, I.L.; Fritz, P.; Horner, E.; Li, N.; Mason, S.; Nel, A.; Oullette, J. The health effects of nonindustrial indoor air pollution. J. Allergy Clin. Immunol. 2008, 121, 585–591.
- Ghaffarianhoseini, A.; AlWaer, H.; Omrany, H.; Ghaffarianhoseini, A.; Alalouch, C.; Clements-Croome, D.; Tookey, J. Sick building syndrome: Are we doing enough? Archit. Sci. Rev. 2018, 61, 99–121.
- Salonen, H.; Salthammer, T.; Morawska, L. Human exposure to ozone in school and office indoor environments. Environ. Int. 2018, 119, 503–514.
- Huang, Y.; Yang, Z.; Gao, Z. Contributions of indoor and outdoor sources to ozone in residential buildings in nanjing. Int. J. Environ. Res. Public Health 2019, 16, 2587.
- Seow, W.J.; Downward, G.S.; Wei, H.; Rothman, N.; Reiss, B.; Xu, J.; Bassig, B.A.; Li, J.; He, J.; Hosgood, H.D. Indoor concentrations of nitrogen dioxide and sulfur dioxide from burning solid fuels for cooking and heating in Yunnan Province, China. Indoor Air 2016, 26, 776–783.
- Du, W.; Li, X.; Chen, Y.; Shen, G. Household air pollution and personal exposure to air pollutants in rural China—A review. Environ. Pollut. 2018, 237, 625–638.
- Mattiuzzi, C.; Lippi, G. Worldwide epidemiology of carbon monoxide poisoning. Hum. Exp. Toxicol. 2020, 39, 387–392.
- Hampson, N.B.; Weaver, L. Carbon monoxide poisoning: A new incidence for an old disease. Undersea Hyperb. Med. 2007, 34, 163–168.
- Harper, A.; Croft-Baker, J. Carbon monoxide poisoning: Undetected by both patients and their doctors. Age Ageing 2004, 33, 105–109.
- Oh, H.-J.; Jeong, N.-N.; Sohn, J.-R.; Kim, J. Personal exposure to indoor aerosols as actual concern: Perceived indoor and outdoor air quality, and health performances. Build. Environ. 2019, 165, 106403.
- Cao, Q.; Li, F.; Zhang, T.T.; Wang, S. A ventilator that responds to outdoor conditions for ventilation and air filtration. Energy Build. 2020, 229, 110498.
- Schabath, M.B.; Cote, M.L. Cancer progress and priorities: Lung cancer. Cancer Epidemiol. Biomark. Prev. 2019, 28, 1563–1579.
- Hwang, H.-M.; Park, E.-K.; Young, T.M.; Hammock, B.D. Occurrence of endocrine-disrupting chemicals in indoor dust. Sci. Total Environ. 2008, 404, 26–35.
- Lucattini, L.; Poma, G.; Covaci, A.; de Boer, J.; Lamoree, M.H.; Leonards, P.E. A review of semi-volatile organic compounds (SVOCs) in the indoor environment: Occurrence in consumer products, indoor air and dust. Chemosphere 2018, 201, 466–482.
- Baldacci, S.; Maio, S.; Cerrai, S.; Sarno, G.; Baïz, N.; Simoni, M.; Annesi-Maesano, I.; Viegi, G.; Study, H. Allergy and asthma: Effects of the exposure to particulate matter and biological allergens. Respir. Med. 2015, 109, 1089–1104.
- Hospodsky, D.; Qian, J.; Nazaroff, W.W.; Yamamoto, N.; Bibby, K.; Rismani-Yazdi, H. Human occupancy as a source of indoor airborne bacteria. PLoS ONE 2012, 7, e34867.
- Adams, R.I.; Miletto, M.; Taylor, J.W.; Bruns, T.D. Dispersal in microbes: Fungi in indoor air are dominated by outdoor air and show dispersal limitation at short distances. ISME J. 2013, 7, 1262–1273.
- Colbeck, I.; Nasir, Z.A.; Ali, Z. Characteristics of indoor/outdoor particulate pollution in urban and rural residential environment of Pakistan. Indoor Air 2010, 20, 40–51.
- Junaid, M.; Syed, J.H.; Abbasi, N.A.; Hashmi, M.Z.; Malik, R.N.; Pei, D.-S. Status of indoor air pollution (IAP) through particulate matter (PM) emissions and associated health concerns in South Asia. Chemosphere 2018, 191, 651–663.
- Naeem, A.; Rafiq, L.; Nazar, R.; Kashif, M.; Naqvi, S.H.Z. An assessment of Risk Factors and Health Impacts Associated with Indoor Air Pollution and Tobacco Smoke in Lahore, Pakistan. J. Qual. Assur. Agric. Sci. 2022, 2, 37–45.
- Aslam, R.; Sharif, F.; Baqar, M.; Nizami, A.-S.; Ashraf, U. Role of ambient air pollution in asthma spread among various population groups of Lahore City: A case study. Environ. Sci. Pollut. Res. 2022, 30, 8682–8697.
- Khalid, F.; Qadir, A.; Hashmi, M.Z.; Mehmood, A.; Aslam, I.; Zhang, G.; Ahmed, Z. Evaluation of ceiling fan dust as an indicator of indoor PCBs pollution in selected cities of Punjab, Pakistan: Implication on human health. Arab. J. Geosci. 2022, 15, 876.
- Cao, Z.; Xu, F.; Covaci, A.; Wu, M.; Yu, G.; Wang, B.; Deng, S.; Huang, J. Differences in the seasonal variation of brominated and phosphorus flame retardants in office dust. Environ. Int. 2014, 65, 100–106.
- Nasir, Z.A.; Colbeck, I.; Sultan, S.; Ahmed, S. Bioaerosols in residential micro-environments in low income countries: A case study from Pakistan. Environ. Pollut. 2012, 168, 15–22.
- Sidra, S.; Ali, Z.; Sultan, S.; Ahmed, S.; Colbeck, I.; Nasir, Z.A. Assessment of airborne microflora in the indoor micro-environments of residential houses of Lahore, Pakistan. Aerosol Air Qual. Res. 2015, 15, 2385–2396.
- Rajagopalan, P.; Goodman, N. Improving the indoor air quality of residential buildings during bushfire smoke events. Climate 2021, 9, 32.
- Khwaja, M.A.; Shams, T. Pakistan National Ambient Air Quality Standards: A Comparative Assessment with Selected Asian Countries and World Health Organization (WHO); Sustainable Development Policy Institute: Islamabad, Pakistan, 2020.
- Yasmin, N.; Grundmann, P. Home-cooked energy transitions: Women empowerment and biogas-based cooking technology in Pakistan. Energy Policy 2020, 137, 111074.
- Shams, Z.I.; Javed, T.; Zubair, A.; Waqas, M.; Ali, S.; Ahmed, A. Carbon Monoxide Concentrations in Kitchens of Gas-fired Burners, Karachi, Pakistan: Carbon Monoxide in Karachi Bungalow and Apartment Kitchens. Pak. J. Sci. Ind. Res. Ser. A Phys. Sci. 2022, 65, 25–32.
- Qayyum, F.; Mehmood, U.; Tariq, S.; Nawaz, H. Particulate matter (PM2.5) and diseases: An autoregressive distributed lag (ARDL) technique. Environ. Sci. Pollut. Res. 2021, 28, 67511–67518.
- Argunhan, Z.; Avci, A.S. Statistical evaluation of indoor air quality parameters in classrooms of a university. Adv. Meteorol. 2018, 2018, 4391579.
- Wolkoff, P. Indoor air humidity, air quality, and health—An overview. Int. J. Hyg. Environ. Health 2018, 221, 376–390.
- Chojer, H.; Branco, P.; Martins, F.; Alvim-Ferraz, M.; Sousa, S. Development of low-cost indoor air quality monitoring devices: Recent advancements. Sci. Total Environ. 2020, 727, 138385.
- Bag, A.; Lee, N.-E. Gas sensing with heterostructures based on two-dimensional nanostructured materials: A review. J. Mater. Chem. C 2019, 7, 13367–13383.
- Hapsari, A.A.; Hajamydeen, A.I.; Abdullah, M.I. A review on indoor air quality monitoring using iot at campus environment. Int. J. Eng. Technol. 2018, 7, 55–60.
- Saini, J.; Dutta, M.; Marques, G. A comprehensive review on indoor air quality monitoring systems for enhanced public health. Sustain. Environ. Res. 2020, 30, 6.
- Saini, J.; Dutta, M.; Marques, G. Indoor air quality monitoring systems based on internet of things: A systematic review. Int. J. Environ. Res. Public Health 2020, 17, 4942.
- Pitarma, R.; Marques, G.; Caetano, F. Monitoring indoor air quality to improve occupational health. In New Advances in Information Systems and Technologies; Springer: Berlin/Heidelberg, Germany, 2016; pp. 13–21.
- Kim, J.-J.; Jung, S.K.; Kim, J.T. Wireless monitoring of indoor air quality by a sensor network. Indoor Built Environ. 2010, 19, 145–150.
- Li, Z.; Askim, J.R.; Suslick, K.S. The optoelectronic nose: Colorimetric and fluorometric sensor arrays. Chem. Rev. 2018, 119, 231–292.
- Taştan, M.; Gökozan, H. Real-time monitoring of indoor air quality with internet of things-based E-nose. Appl. Sci. 2019, 9, 3435.
- Chen, K.; Gao, W.; Emaminejad, S.; Kiriya, D.; Ota, H.; Nyein, H.Y.Y.; Takei, K.; Javey, A. Printed carbon nanotube electronics and sensor systems. Adv. Mater. 2016, 28, 4397–4414.
This entry is offline, you can click here to edit this entry!
